What is the diagnosis code for AAA screening?
Use 2017 CPT® code 76706 Ultrasound, abdominal aorta, real time, with image documentation, screening study for abdominal aortic aneurysm (AAA) for AAA screening.
Where can one find ICD 10 diagnosis codes?
Search the full ICD-10 catalog by:
- Code
- Code Descriptions
- Clinical Terms or Synonyms
What are the new ICD 10 codes?
The new codes are for describing the infusion of tixagevimab and cilgavimab monoclonal antibody (code XW023X7), and the infusion of other new technology monoclonal antibody (code XW023Y7).
What is the ICD 10 diagnosis code for?
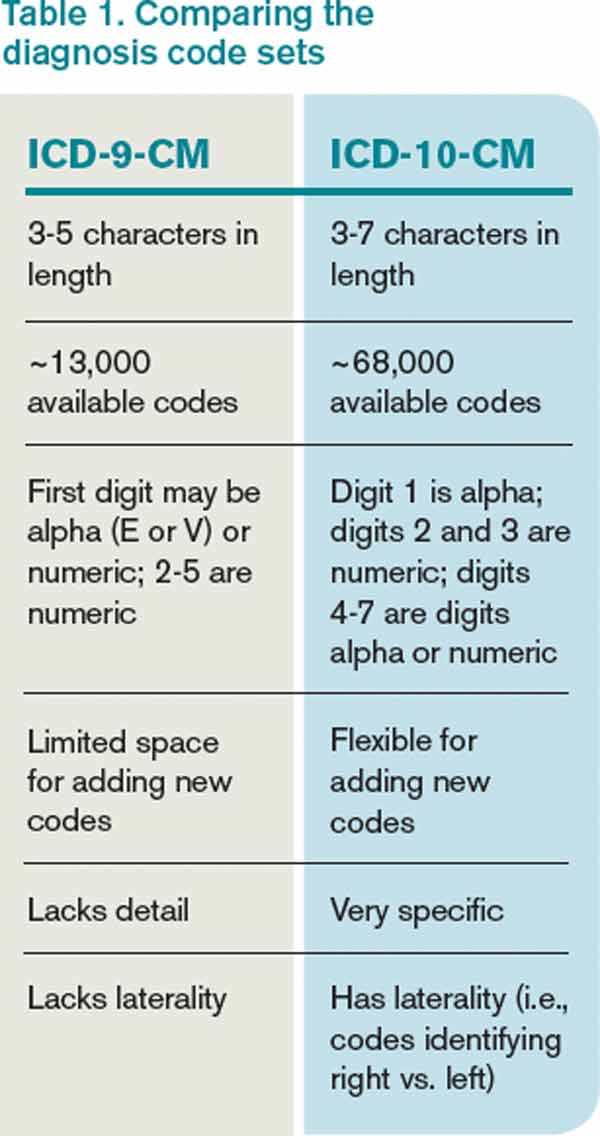
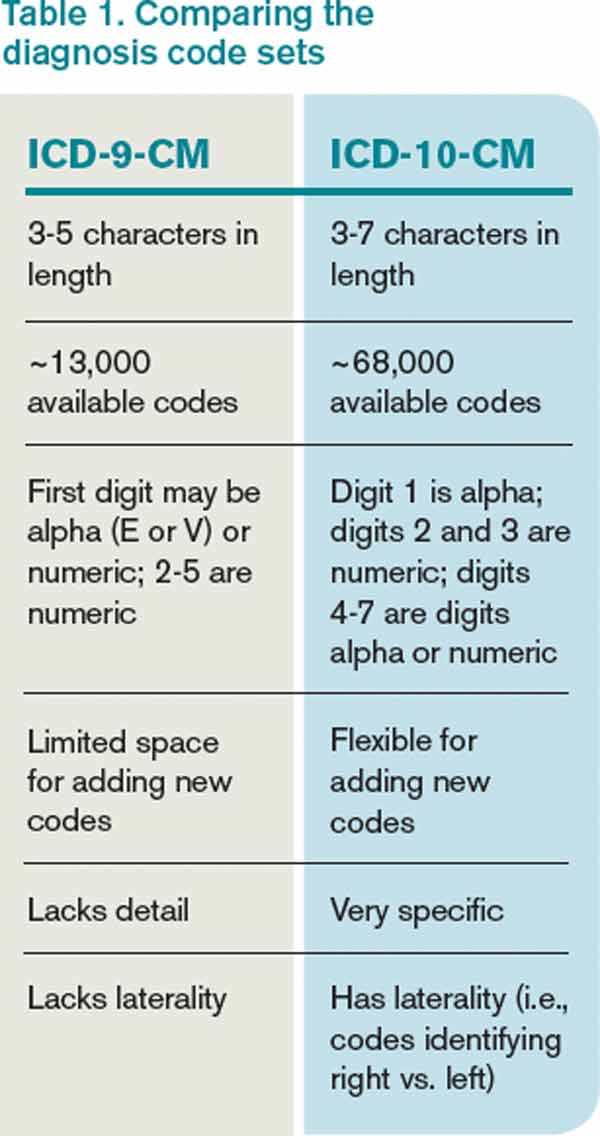
The ICD-10-CM is a catalog of diagnosis codes used by medical professionals for medical coding and reporting in health care settings. The Centers for Medicare and Medicaid Services (CMS) maintain the catalog in the U.S. releasing yearly updates.
What is the ICD-10 code for AAA?
I71.4ICD-10 code I71. 4 for Abdominal aortic aneurysm, without rupture is a medical classification as listed by WHO under the range - Diseases of the circulatory system .
How do you bill AAA screening?
CPT® code 76706: Ultrasound, abdominal aorta, real time with image documentation, screening study for abdominal aortic aneurysm (AAA) Short Descriptor: Us abdl aorta screen AAA.
What is a Triple AAA screening?
Abdominal aortic aneurysm (AAA) screening is a way of checking if there's a bulge or swelling in the aorta, the main blood vessel that runs from your heart down through your tummy. This bulge or swelling is called an abdominal aortic aneurysm, or AAA.
What is the CPT code for screening duplex scan for abdominal aortic aneurysm?
CPT code 93978 - (Duplex scan of aorta, inferior vena cava, iliac vasculature, or bypass grafts; complete study) was requested for screening for abdominal aortic aneurysm.
What ICD 10 code covers AAA screening?
The ICD-10-CM code to support AAA screening is Z13. 6 Encounter for screening for cardiovascular disorders [abdominal aortic aneurysm (AAA)].
How do I code AAA?
I71.0 – Dissection of aortaI71.0 – Dissection of aorta.I71.3 – Abdominal aortic aneurysm, ruptured.I71.4 – Abdominal aortic aneurysm, without rupture.I71.5 – Thoracoabdominal aortic aneurysm, ruptured.I71.6 – Thoracoabdominal aortic aneurysm, without rupture.I71.8 – Aortic aneurysm of unspecified site, ruptured.More items...•
When was AAA screening introduced?
The national implementation of AAA screening, which began in 2009, has been a major public health success story that has prevented many premature deaths. Who's invited? The NHS invites all men for free screening during the year they turn 65.
What is the CPT code for AAA repair?
For repair of an abdominal aortic aneurysm use CPT codes 36200, 36245-36248, and 36140 as appropriate.
How often should you be screened for abdominal aortic aneurysm?
Recommendation Summary The USPSTF recommends 1-time screening for abdominal aortic aneurysm (AAA) with ultrasonography in men aged 65 to 75 years who have ever smoked.
What is the difference between 76706 and 76775?
If a patient has just an abdominal aorta ultrasound, do we use code 76770 or 76775? Code 76706 is assigned when a screening ultrasound for AAA is ordered for a Medicare beneficiary. Otherwise, code 76775 would be assigned.
What is the ICD-10 code for a smoker?
When choosing the appropriate diagnosis code to describe a beneficiary who is a former smoker who meets the tobacco usage criteria for this benefit, ICD-10 diagnosis code Z87.891 can be used. In the case of a beneficiary who is a current smoker, choose the applicable code from F17.210, F17.211, F17.213, F17.218 or F17.219.
What is CMS in healthcare?
The Centers for Medicare & Medicaid Services (CMS), the federal agency responsible for administration of the Medicare, Medicaid and the State Children's Health Insurance Programs, contracts with certain organizations to assist in the administration of the Medicare program. Medicare contractors are required to develop and disseminate Articles. CMS believes that the Internet is an effective method to share Articles that Medicare contractors develop. While every effort has been made to provide accurate and complete information, CMS does not guarantee that there are no errors in the information displayed on this web site. THE UNITED STATES GOVERNMENT AND ITS EMPLOYEES ARE NOT LIABLE FOR ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION, PRODUCT, OR PROCESSES DISCLOSED HEREIN. Neither the United States Government nor its employees represent that use of such information, product, or processes will not infringe on privately owned rights. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information, product, or process.
What is a bill and coding article?
Billing and Coding articles provide guidance for the related Local Coverage Determination (LCD) and assist providers in submitting correct claims for payment. Billing and Coding articles typically include CPT/HCPCS procedure codes, ICD-10-CM diagnosis codes, as well as Bill Type, Revenue, and CPT/HCPCS Modifier codes. The code lists in the article help explain which services (procedures) the related LCD applies to, the diagnosis codes for which the service is covered, or for which the service is not considered reasonable and necessary and therefore not covered.
Is CPT a year 2000?
CPT is provided “as is” without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. AMA warrants that due to the nature of CPT, it does not manipulate or process dates, therefore there is no Year 2000 issue with CPT. AMA disclaims responsibility for any errors in CPT that may arise as a result of CPT being used in conjunction with any software and/or hardware system that is not Year 2000 compliant. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon no upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
Can you use CPT in Medicare?
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials of CMS internally within your organization within the United States for the sole use by yourself, employees and agents. Use is limited to use in Medicare, Medicaid or other programs administered by the Centers for Medicare and Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
Is the ADA a third party beneficiary?
The ADA is a third party beneficiary to this Agreement.
Does CMS have a CDT license?
Organizations who contract with CMS acknowledge that they may have a commercial CDT license with the ADA, and that use of CDT codes as permitted herein for the administration of CMS programs does not extend to any other programs or services the organization may administer and royalties dues for the use of the CDT codes are governed by their commercial license.
How to detect AAA?
The primary way of screening for AAA is with an abdominal ultrasound. This screening test is easy to perform, noninvasive, does not involve radiation, and is highly accurate in detecting AAA. The potential benefit of screening for AAA is detecting and repairing it before rupture, which requires emergency surgery and has a high mortality rate. The only potential harm of screening is related to the risks of surgical repair such as bleeding complications and death.#N#The U.S. Preventive Services Task Force recommendation applies to adults aged 50 years or older who do not have any signs or symptoms of AAA. Early detection of AAA can save lives.#N#Based on current evidence, the USPSTF concludes with moderate certainty that screening for AAA in men aged 65 to 75 years who have ever smoked is of moderate net benefit, even if they have no symptoms. For men aged 65 to 75 years who have never smoked, the USPSTF concludes with moderate certainty that screening is of small net benefit, and should be offered selectively based on medical history and risk factors. There is sufficient evidence that there is no net benefit of screening women who have never smoked and have no family history of AAA. For women aged 65 to 75 years who have ever smoked or have a family history of AAA, there is not enough evidence to adequately assess the balance of benefits and harms of screening for AAA.
What is the risk of a ruptured AAA?
Although the risk for rupture varies greatly by aneurysm size, the associated risk for death with rupture is as high as 81 percent . This is why it is imperative to screen those at risk, and once diagnosed, the size of a patient’s AAA should be monitored periodically.
Is smoking a risk factor for an aortic aneurysm?
Smoking is the strongest predictor of AAA prevalence, growth, and rupture rates. There is a dose-response relationship, as greater smoking exposure is associated with an increased risk for AAA. Most aortic aneurysms do not cause symptoms until they rupture, which is why they are so dangerous.
Is there a net benefit to screening for AAA?
There is sufficient evidence that there is no net benefit of screening women who have never smoked and have no family history of AAA. For women aged 65 to 75 years who have ever smoked or have a family history of AAA, there is not enough evidence to adequately assess the balance of benefits and harms of screening for AAA.
Does Medicare cover AAA screening?
Coding AAA Screening. Medicare covers a one-time AAA screening for beneficiaries with certain risk factors for AAA who have received a referral from their provider. There is no deductible or coinsurance/co-payment for the AAA ultrasound screening test. A patient is considered at risk if they have a family history of abdominal aortic aneurysms, ...
What is the most widely used criteria for screening for AAA?
Carnevale and associates (2020) noted that USPSTF guidelines are the most widely used criteria for screening for AAA. However, when the USPSTF criteria are applied retrospectively to a group of patients who have undergone treatment for AAA, there are many patients who satisfy none of the AAA screening criteria.
Why does Aetna consider AAA screening experimental and investigational?
Aetna considers AAA screening experimental and investigational for all other indications because its effectiveness for indications other than the one listed above has not been established.
How common is an abdominal aortic aneurysm?
Furthermore, an UpToDate review on "Screening for abdominal aortic aneurysm" (Mohler, 2017) states that "The prevalence of AAAs is negligible in individuals under the age of 60, particularly women, but then increases dramatically with age. Screening studies show that AAA occurs in 4 to 9 % of individuals over the age of 60. However, most (57 to 88 %) of these aneurysms are ≤ 3.5 cm in diameter. Clinically important aneurysms over 4.0 cm in diameter are present in about 1 % of men between the ages of 55 and 64; the prevalence increases by 2 to 4 % per decade thereafter … AAAs are 4 to 6 times more common in men than in women. In addition, AAAs develop in women about 10 years later than in men. A model to identify women with multiple cardiovascular risk factors who are at particularly high risk for AAA and may benefit from screening has been developed combining 2 United States data sets, but remains to be validated in other populations … Only one study examined population-based screening in women, a population in whom the prevalence of AAA is significantly lower than in men (1.3 versus 7.6 %). Screening had no effect on AAA-related mortality (OR 1.0, 95 % CI 0.14-7.07) or all-cause mortality (OR 1.05, 0.92-1.19) at 5-year and 10-year follow-up … The USPSTF advises against screening women who have never smoked, but conclude that evidence is insufficient to assess the benefits and harms of screening women aged 65 to 75 who have ever smoked … The Society for Vascular Surgery issued updated guidelines in 2009 recommending one-time screening for all men older than 65 (and at 55 if family history is positive) and screening for women older than 65 who have smoked or have a family history. The guidelines cite that, although the prevalence of AAA is lower in women than men, rupture rates are higher in women and life expectancy is longer … The Canadian Society for Vascular Surgery recommends screening for men between age 65 and 75 who are candidates for surgery. Recommendations are not to screen women > 65 years on a population basis, but to individualize screening for women with multiple risks (smoking, cerebrovascular disease, and family history)".
How small is an AAA?
Brown et al (2013) stated that small AAAs (3.0 cm to 5.4 cm in diameter ) are monitored by US surveillance. The intervals between surveillance scans should be chosen to detect an expanding aneurysm prior to rupture. These researchers performed a meta-analysis to limit risk of aneurysm rupture or excessive growth by optimizing US surveillance intervals. Individual patient data from studies of small AAA growth and rupture were assessed. Studies were identified for inclusion through a systematic literature search through December 2010. Study authors were contacted, which yielded 18 data sets providing repeated US measurements of AAA diameter over time in 15,471 patients. Abdominal aortic aneurysms diameters were analyzed using a random-effects model that allowed for between-patient variability in size and growth rate. Rupture rates were analyzed by proportional hazards regression using the modeled AAA diameter as a time-varying covariate. Predictions of the risks of exceeding 5.5-cm diameter and of rupture within given time intervals were estimated and pooled across studies by random effects meta-analysis. Abdominal aortic aneurysms growth and rupture rates varied considerably across studies. For each 0.5-cm increase in AAA diameter, growth rates increased on average by 0.59 mm per year (95 % CI: 0.51 to 0.66) and rupture rates increased by a factor of 1.91 (95 % CI: 1.61 to 2.25). For example, to control the AAA growth risk in men of exceeding 5.5 cm to below 10 %, on average, a 7.4-year surveillance interval (95 % CI: 6.7 to 8.1) is sufficient for a 3.0-cm AAA, while an 8-month interval (95 % CI: 7 to 10) is necessary for a 5.0-cm AAA. To control the risk of rupture in men to below 1 %, the corresponding estimated surveillance intervals are 8.5 years (95 % CI: 7.0 to 10.5) and 17 months (95 % CI: 14 to 22). The authors concluded that in contrast to the commonly adopted surveillance intervals in current AAA screening programs, surveillance intervals of several years may be clinically acceptable for the majority of patients with small AAA.
What is color flow duplex ultrasound?
Color flow duplex ultrasound scanning has been used as an surveillance modality for clinically significant endoleaks in patients who have undergone endovascular repair of AAAs. Sun (2006) systematically reviewed the findings of diagnostic value of color duplex ultrasound (US) in the follow-up of endovascular repair of AAAs. Studies comparing the diagnostic accuracy of color duplex US with that of computed tomographic (CT) angiography were included, and analysis was performed of the detection of endoleaks and measurement of aneurysm diameter. A total of 21 studies (39 separate comparisons) met the criteria and were included for analysis. Pooled estimates of sensitivity, specificity, positive-predictive value (PPV), negative-predictive value (NPV), and accuracy of color duplex US compared with CT angiography (with 95 % confidence interval [CI]) were 66 % (52 to 81 %), 93 % (89 to 97 %), 76 % (65 to 87 %), 90 % (86 to 95 %), and 91 % (86 to 97 %), respectively, for unenhanced color duplex US; and 81 % (52 to 100 %), 82 % (68 to 97 %), 58 % (26 to 90 %), 95 % (87 to 100 %), and 98 % (91 to 100%), respectively, for enhanced color duplex US. The sensitivity in the detection of endoleak was significantly improved with contrast material-enhanced color duplex US compared with unenhanced color duplex US (p < 0.05); however, no significant difference was found regarding the specificity, PPV, NPV, and accuracy between unenhanced and enhanced color duplex US (p > 0.05). Color duplex US was insensitive in measurement of aneurysm diameter compared with CT angiography in most situations. The authors concluded that color duplex US is not as accurate as CT angiography and can not replace CT angiography in the follow-up of endovascular aortic repair of AAAs. However, the use of contrast material-enhanced color duplex US resulted in improvement of diagnostic accuracy in the detection of endoleak and warrants further study.
How much does an AAA of 5.5 cm reduce?
Open surgical repair for an AAA of at least 5.5 cm leads to an estimated 43 % reduction in AAA-specific mortality in older men who undergo screening. However, there is no current evidence that screening reduces all-cause mortality in this population.
Can you get AAA if you have never smoked?
The USPSTF recommend s against routine screening for AAA in women who have never smoked. (D recommendation).
Popular Posts:
- 1. icd 10 code for 715.96
- 2. icd 10 code for postop
- 3. icd 10 code for bacterial erruption right buttock
- 4. icd 10 code for breast injury
- 5. icd 10 code for prostatomegaly
- 6. icd 10 code for stroke with right sided hemiparesis
- 7. icd 10 code for stable right total hip arthroscopy
- 8. icd-10 code for ureteral stent removal
- 9. 2015 icd 10 code for right intertrochanteric fracture
- 10. icd 10 code for impaired nutrition