What are the new ICD 10 codes?
The new codes are for describing the infusion of tixagevimab and cilgavimab monoclonal antibody (code XW023X7), and the infusion of other new technology monoclonal antibody (code XW023Y7).
How many ICD 10 codes are there?
- ICD-10 codes were developed by the World Health Organization (WHO) External file_external .
- ICD-10-CM codes were developed and are maintained by CDC’s National Center for Health Statistics under authorization by the WHO.
- ICD-10-PCS codes External file_external were developed and are maintained by Centers for Medicare and Medicaid Services. ...
What is the ICD 10 diagnosis code for?
The ICD-10-CM is a catalog of diagnosis codes used by medical professionals for medical coding and reporting in health care settings. The Centers for Medicare and Medicaid Services (CMS) maintain the catalog in the U.S. releasing yearly updates.
What does ICD 10 mean?
ICD-10 is the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD), a medical classification list by the World Health Organization (WHO). It contains codes for diseases, signs and symptoms, abnormal findings, complaints, social circumstances, and external causes of injury or diseases.

What is T81 89XA?
ICD-10 Code for Other complications of procedures, not elsewhere classified, initial encounter- T81. 89XA- Codify by AAPC. Injury, poisoning and certain other consequences of external causes.
What is the ICD-10 code for lymphadenopathy?
Enlarged lymph nodes, unspecified R59. 9 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM R59. 9 became effective on October 1, 2021.
What is the ICD-10 code for lymphedema?
ICD-10 code I89. 0 for Lymphedema, not elsewhere classified is a medical classification as listed by WHO under the range - Diseases of the circulatory system .
What is the ICD-10 code for nonhealing surgical wound?
998.83 - Non-healing surgical wound | ICD-10-CM.
What is localized enlarged lymph nodes?
If swollen lymph nodes are only found in one area of your body, it's called localized swollen lymph nodes. And most of the time, you have a virus so there's no treatment truly needed and it will just run its course. The nodes will gradually shrink back to their normal size.
What is the difference between localized and generalized enlarged lymph nodes?
Normal lymph nodes are usually less than 1 cm in diameter and tend to be larger in adolescence than later in life. A clinically useful approach is to classify lymphadenopathy as localized when it involves only one region, such as the neck or axilla, and generalized when it involves more than one region [1].
What is the ICD-10 code for lymphedema lower extremity?
I89. 0 - Lymphedema, not elsewhere classified. ICD-10-CM.
What is the CPT code for lymphedema?
Medically necessary hands-on MLD is a covered Medicare service and is coded using CPT® 97140 for manual therapy. There is no Medicare coverage for lymphedema compression bandage application as this is considered to be an unskilled service.
What is elephantiasis Nostras Verrucosa?
Elephantiasis nostras verrucosa (ENV) is a rare form of chronic lymphedema that causes progressive cutaneous hypertrophy. It can lead to severe disfiguration of body parts with gravity-dependent blood flow, especially the lower extremities.
How do you code a wound in ICD-10?
The types of open wounds classified in ICD-10-CM are laceration without foreign body, laceration with foreign body, puncture wound without foreign body, puncture wound with foreign body, open bite, and unspecified open wound. For instance, S81. 812A Laceration without foreign body, right lower leg, initial encounter.
How do you code an unspecified wound?
8-, “other injury of unspecified body region,” or T14. 9-, “injury, unspecified,” because these codes don't describe the location or type of wound. These injury codes require a 7th character to indicate the episode of care.
What is the ICD-10 code for Postprocedural intraabdominal abscess?
Postprocedural retroperitoneal abscess The 2022 edition of ICD-10-CM K68. 11 became effective on October 1, 2021.
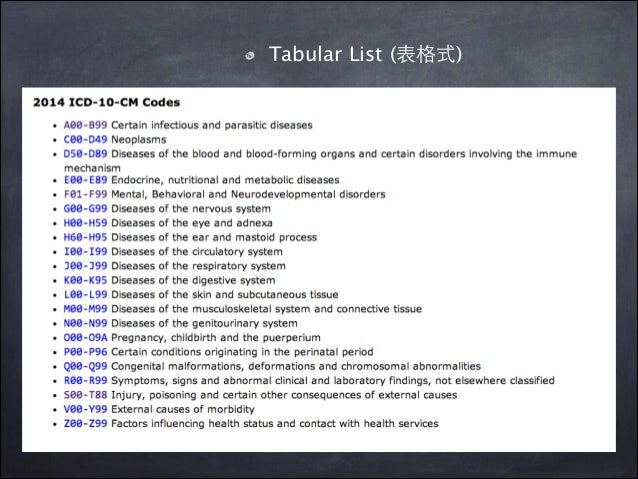
What is the convention of ICd 10?
The conventions for the ICD-10-CM are the general rules for use of the classification independent of the guidelines. These conventions are incorporated within the Alphabetic Index and Tabular List of the ICD-10-CM as instructional notes.
When to assign Y to ICD-10?
two separate conditions classified to the same ICD-10-CM diagnosis code): Assign “Y” if all conditions represented by the single ICD-10-CM code were present on admission (e.g. bilateral unspecified age-related cataracts).
What does NEC mean in coding?
NEC “Not elsewhere classifiable” This abbreviation in the Alphabetic Index represents “other specified.”When a specific code is not available for a condition, the Alphabetic Index directs the coder to the “other specified” code in the Tabular List.
When to use counseling Z code?
Counseling Z codes are used when a patient or family member receives assistance in the aftermath of an illness or injury , or when support is required in coping with family or social problems. They are not used in conjunction with a diagnosis code when the counseling component of care is considered integral to standard treatment.
When assigning a chapter 15 code for sepsis complicating abortion, pregnancy, childbirth, and the
When assigning a chapter 15 code for sepsis complicating abortion, pregnancy, childbirth, and the puerperium, a code for the specific type of infection should be assigned as an additional diagnosis. If severe sepsis is present, a code from subcategory R65.2, Severe sepsis, and code(s) for associated organ dysfunction(s) should also be assigned as additional diagnoses.
Do not code diagnoses documented as “probable”, “suspected,” “questionable,” “
Do not code diagnoses documented as “probable”, “suspected,” “questionable,” “rule out ,” or “working diagnosis” or other similar terms indicating uncertainty. Rather, code the condition(s) to the highest degree of certainty for that encounter/visit, such as symptoms, signs, abnormal test results, or other reason for the visit.
What is the term for a right arm swollen from lymph obstruction?
Right arm lymphedema (swelling from lymph obstruction) Right leg lymphedema (swelling from lymph obstruction) Clinical Information. A condition that is caused by trauma to the lymph system, which disrupts the normal flow of lymph fluid.
What is a type 1 exclude note?
A type 1 excludes note is a pure excludes. It means "not coded here". A type 1 excludes note indicates that the code excluded should never be used at the same time as I89.0. A type 1 excludes note is for used for when two conditions cannot occur together, such as a congenital form versus an acquired form of the same condition.
Popular Posts:
- 1. icd 10 code for impacted fracture of the shoulder lymphedema
- 2. icd 10 code for general surgery
- 3. icd 9 code for intractable migraine
- 4. 2018 icd 10 code for monoclonal gammopathy
- 5. icd-10 code for concussion without loss of consciousness
- 6. icd 10 code for idiopathic peripheraol neuropathy
- 7. icd 10 code for amaurosis fugax
- 8. icd-10 code for sacral sprain strain
- 9. what is the icd 9 code for medical examination by physician employed by state
- 10. icd 9 code for scalp woound