Is an intra-aortic balloon pump (IABP) reported under ICD-10-CM/PCS?
The Central Office on ICD-10-CM/PCS has received numerous requests regarding the reporting of an intra-aortic balloon pump (IABP). The following information regarding an IABP, along with some coding examples, is being provided to help clarify the coding issues.
What is intra-aortic balloon pump?
Intra-aortic balloon pump is the simplest, cost-effective, easy to implant and explant in the coronary catheterization laboratory by an interventional cardiologist and can effectively be managed in an intensive care unit by an intensivist.[2]
What are the precautions for patients with intra-abdominal balloon (IABP) catheterization?
Patients with IABP catheter inserted in the femoral artery need bedrest with as minimal as possible movement of the lower extremity to avoid displacement of the intra-aortic balloon from its recommended position.
What is the ejection fraction of an Intubation Balloon Pump?
Intra-aortic balloon pump insertion. None. Approximately 50 mL. Left common femoral artery and left common femoral vein. ejection fraction of 20%, congestive heart failure. The patient was intubated before cardiac catheterization due to severe congestive heart failure with hypoxemia.
What is the CPT code for intra-aortic balloon pump?
33967: Insertion of intra-aortic balloon assist device, percutaneous.
What is a intra-aortic balloon device?
An intra-aortic balloon pump (IABP) is a type of therapeutic device. It helps your heart pump more blood. You may need it if your heart is unable to pump enough blood for your body. The IABP consists of a thin, flexible tube called a catheter. Attached to the tip of the catheter is a long balloon.
What is augmentation in intra-aortic balloon pump?
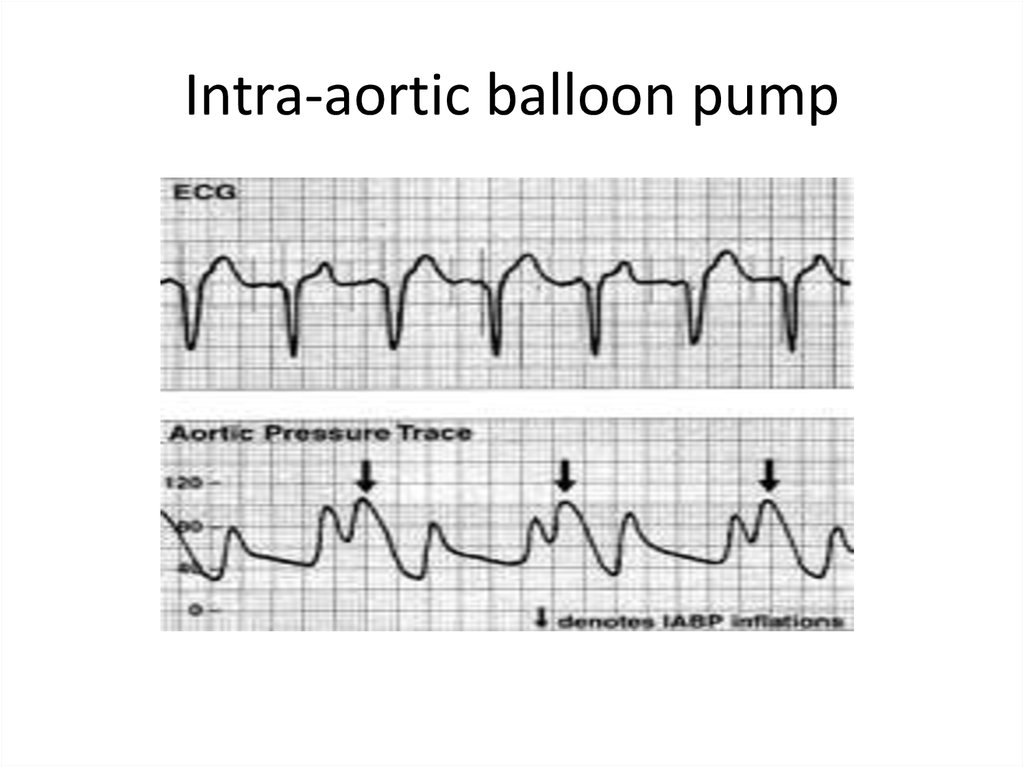
Treatment with the intraaortic balloon pump (IABP) is the most common form of mechanical support for the failing heart. Augmentation of diastolic pressure during balloon inflation contributes to the coronary circulation and the presystolic deflation of the balloon reduces the resistance to systolic output.
What Code S should be reported for a percutaneous insertion of an intra-aortic balloon assist device with removal of the device on the same day?
It is appropriate to report both the intra-aortic balloon pump (IAB) insertion and the intra-aortic balloon pump removal on the same day with code 33967, Insertion of intra-aortic balloon assist device, percutaneous, and code 33968, Removal of intra-aortic balloon assist device, percutaneous.
Is a balloon pump a VAD?
The intra-aortic balloon pumps (IABPs) have been the gold standard for minimally invasive circulatory support for 40 years, but they were joined in recent years by percutaneously deployed ventricular assist devices (P-VADs). IABP makers Teleflex and Maquet claim their devices offer between .
How does an intra-aortic balloon pump work?
The balloon inflates just as the aortic valve closes, which increases the blood pressure above the balloon long enough to push more blood through the coronary arteries, thus increasing delivery of needed oxygen and nutrients to the cardiac muscle.
What does IABP 1 1 mean?
The amount of aid a balloon pump provides can be quantified as a ratio of native beats to assisted beats. Full support is at a ratio of 1:1; that is, every beat is augmented by the IABP.
How long can an intra-aortic balloon pump stay in?
The catheter connects to a computer that controls the rate of inflation and deflation. While most patients only use the IABP for a few days, it can stay in place for up to a month.
Why is helium used in intra-aortic balloon pump?
Helium is used to inflate the balloon as its low density means there is little turbulent flow, so the balloon can inflate quickly and deflate slowly. It is also relatively benign and eliminated quickly if there is a leak or rupture in the balloon.
What is the difference between C9600 and 92928?
The second major coronary artery stenting would be reported using the normal stent codes (92928) for the PC or for the facility if a bare metal stent was placed. If a DES was placed in the RC, you would report C9600 for the facility instead of 92928.
Does Medicare pay for 92929?
Group 1. CPT codes 92921, 92925, 92929, 92934, 92938, and 92944 are status “B” (bundled) codes for Medicare and will not be separately reimbursed. Claims for percutaneous coronary intervention must include the appropriate modifiers to identify which vessel is undergoing a specific procedure.
Can you bill 92928 and 92941 together?
So I can code 92928 for additional stent placement with 92941... Yes you can.
How does IABP reduce afterload?
The intra-aortic balloon, by inflating during diastole, displaces blood volume from the thoracic aorta. In systole, as the balloon rapidly deflates, this creates a dead space, effectively reducing afterload for myocardial ejection and improving forward flow from the left ventricle.
Which condition is a contraindication for IABP use?
Contraindications to intra-aortic balloon pump include: Uncontrolled sepsis. Uncontrolled bleeding diathesis. Moderate to severe aortic regurgitation.
Do you need anticoagulation with IABP?
The authors concluded that anticoagulation should be used whenever possible for all IABP patients. This study differs from our findings and the findings of several retrospective studies demonstrating no difference in thrombotic outcomes when comparing anticoagulation strategies.
What is a physiologic effect of late balloon deflation?
Q 4.3 What are the physiological effects? Late deflation of the IAB has these effects: There is no afterload reduction. The inflated balloon may actually impede left ventricular ejection and increase the afterload.
What is included in an intra aortic balloon pump kit?
Intra-aortic balloon pump kit: That includes an intra-aortic balloon pump system with an IABP catheter, arterial dilator, a guidewire, angiographic needle.
How is an IABP catheter inserted?
The IABP catheter is inserted and advanced over the 0.018" guidewire to the proper positioning of the balloon in the aorta. The location of the intra-aortic balloon with its tip lying distal to the left subclavian artery and the proximal portion ending above the origin of renal arteries is considered as the ‘safe zone,’ and the confirmation of position can be by chest x-ray or fluoroscopy. Following guidewire removal, and the central lumen of the catheter is flushed and connected to the transducer to measure intra-aortic pressure. The IABP catheter gets connected to the extender catheter, which then connects to the IABP console. [14]
How does IABP affect the heart?
The IABP assists the heart indirectly by decreasing the afterload and augments diastolic aortic pressure with subsequent enhancement in diastolic blood flow resulting in better perfusion of the peripheral organ as well as a possible improvement in the coronary blood flow. The intra-aortic balloon inflates during diastole synchronously with aortic valve closure and the appearance of a dicrotic notch resulting in the displacement of blood from the thoracic aorta into the peripheral circulation that is followed by rapid deflation before the onset of systole phase of the cardiac cycle. Theoretically, this results in improved diastolic pressure and reduced systolic aortic pressure by reducing the afterload, which subsequently results in decreased left ventricle wall stress reducing the myocardial oxygen demand. These hemodynamic changes improve the cardiac output by increasing stroke volume, particularly in patients with reduced left ventricular function.
Does IABP help with ventricular failure?
IABP use may also help patients with acute right ventricular failure by reducing the right ventricular afterload by decreasing pulmonary artery pressure and left ventricular end-systolic and end-diastolic pressures and, as a result, improves the cardiac output. [5][6]
Does IABP increase aortic stiffness?
Stefanadis et al. demonstrated a 30% increase in aortic distensibility with IABP, thereby reducing the aortic stiffness constant, resulting in a 24% increase in cardiac index and a 31% reduction in myocardial oxygen demand.[3] In patients with systolic heart failure, IABP improves ventriculoarterial coupling ratio and consequently enhances stroke volume by reducing peripheral arterial elasticity without affecting the left ventricular end-systolic elastance. In these patients with low output, a reduction of end-systolic pressures, end-diastolic pressure, and volume of the left ventricle with IABP result in a leftward shift of pressure-volume loop with a reduced pressure-volume loop area suggesting a decrease myocardial oxygen demand. [4]
Do you need informed consent before IABP?
Prior to the insertion of IABP, informed consent is necessary with a clear explanation of the risks and benefits of IABP insertion.
Do you have to flex your leg before IABP?
These instructions include not to flex the leg if femoral artery access of that leg was the entry point for IABP insertion and inability to walk till the device is in place in case of femoral artery access used for device insertion.

Popular Posts:
- 1. icd 10 code for high risk colon cancer surveillance
- 2. icd 10 cm code for pulmonary infiltrates
- 3. icd 10 code for displaced colles' fracture of right radius
- 4. icd 10 code for trauma to left ear canal
- 5. icd 10 code for bilateral l5 spondylolysis
- 6. icd-10 code for liver cirrhosis with ascites
- 7. icd 10 cm code for laceration,r finger
- 8. what is the icd 10 code for blood loss anemia
- 9. icd 10 code for gastroc strain
- 10. icd 10 code for history of cancer of appendix