What is the EMS Code for unresponsive?
Unfortunately, "unresponsive" does not code to anything. "Unconscious" codes to R4020 Unspecified coma. You can take a look at nursing documentation perhaps, if you don't have access to the EMS run sheet. Sign In or Register to comment.
Is unresponsive diagnosis sufficient to code the GCS?
Is there any coding guidance that states that ANY associated documented diagnosis (even if not indexed), such as unresponsive (provided its not an expected finding, or inherent (syncope/seizure)) is sufficient to code the GCS. We are getting pushback from coding that since unresponsive is not indexed, the GCS can not be captured.
What happens if there is no available ICD-10 code for a diagnosis?
If there is no available ICD-10 code for the associated diagnosis, an auditor will not be able to confirm it from the claim submitted and the supporting medical record information identifying the diagnosis would then have to be submitted on appeal to the auditor.

What is the ICD-10 code for unresponsiveness?
ICD-10-CM R40. 20 is grouped within Diagnostic Related Group(s) (MS-DRG v39.0): 080 Nontraumatic stupor and coma with mcc. 081 Nontraumatic stupor and coma without mcc.
What does R41 89 mean?
R41. 89 - Other symptoms and signs involving cognitive functions and awareness | ICD-10-CM.
What is the code z76 89 for?
Persons encountering health services in other specified circumstances89 for Persons encountering health services in other specified circumstances is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
When do you use R41 89?
89 for Other symptoms and signs involving cognitive functions and awareness is a medical classification as listed by WHO under the range - Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified .
What is R53 83?
ICD-9 Code Transition: 780.79 Code R53. 83 is the diagnosis code used for Other Fatigue. It is a condition marked by drowsiness and an unusual lack of energy and mental alertness. It can be caused by many things, including illness, injury, or drugs.
What does anxiety F41 9 mean?
Code F41. 9 is the diagnosis code used for Anxiety Disorder, Unspecified. It is a category of psychiatric disorders which are characterized by anxious feelings or fear often accompanied by physical symptoms associated with anxiety.
Can z76 89 be a primary DX?
89 – persons encountering health serviced in other specified circumstances” as the primary DX for new patients, he is using the new patient CPT.
What is the ICD-10 code for long term use of medication?
The ICD-10 section that covers long-term drug therapy is Z79, with many subsections and specific diagnosis codes.
What is I10 diagnosis?
ICD-Code I10 is a billable ICD-10 code used for healthcare diagnosis reimbursement of Essential (Primary) Hypertension. Its corresponding ICD-9 code is 401.
What is the ICD 10 code for loss of consciousness?
Unspecified intracranial injury with loss of consciousness of unspecified duration, initial encounter. S06. 9X9A is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
What is the ICD 10 code for cognitive dysfunction?
Cognitive communication deficit R41. 841 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM R41. 841 became effective on October 1, 2021.
What is the ICD 10 code for knowledge deficit?
9 Developmental disorder of scholastic skills, unspecified. Learning: disability NOS.
What is unspecified abnormalities of gait and mobility?
Abnormal gait or a walking abnormality is when a person is unable to walk in the usual way. This may be due to injuries, underlying conditions, or problems with the legs and feet. Walking may seems to be an uncomplicated activity.
What causes Pseudodementia?
Causes of pseudodementia include the following: Increased stress and depression alter the hypothalamic-pituitary axis causing cognitive impairment. Psychosocial and environmental factors, including abuse (mental and physical); poor social support; loss of a job; negative life events; and substance misuse.
What is cognitive functions and awareness?
Cognitive functioning refers to multiple mental abilities, including learning, thinking, reasoning, remembering, problem solving, decision making, and attention.
What is the ICD 10 code for behavior changes?
9 for Unspecified behavioral and emotional disorders with onset usually occurring in childhood and adolescence is a medical classification as listed by WHO under the range - Mental, Behavioral and Neurodevelopmental disorders .
What is the code for papyraceous fetus?
papyraceous fetus (O31.0-); code from category O08 to identify any associated complication.
What is the code for long term use of insulin?
Unsp diabetes in pregnancy, childbirth and the puerperium; code for long-term (current) use of insulin (Z79.4)
What is code Y07.-?
code to identify the perpetrator of abuse ( Y07.-)
What is the code for carrier state?
code to identify the carrier state ( Z22.-)
What is the code for thrombosis in pregnancy?
Phlebitis in pregnancy NOS; Thrombophlebitis of legs in pregnancy; Thrombosis in pregnancy NOS; code to identify the superficial thrombophlebitis (I80.0-)
What is C04.9?
C04.9 Malignant neoplasm of floor of mouth, unspeci ...
What is the code for cholelithiasis?
Sickle-cell thalassemia, unsp, with crisis with oth comp; code to identify complications, such as:; cholelithiasis (K80.-); priapism (N48.32)
What is the code for alcohol abuse and dependence?
if applicable exocrine pancreatic insufficiency (K86.81); code to identify:; alcohol abuse and dependence (F10.-)
What is the C7A.092 code?
malignant carcinoid tumor of the stomach (C7A.092); code to identify:; alcohol abuse and dependence (F10.-)
When to use accord extent body involv?
Corrosions classified accord extent body involv; This category is to be used as the primary code only when the site of the corrosion is unspecified. It may be used as a supplementary code with categories T20-T25 when the site is specified.
Document Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Italicized font represents CMS national language/wording copied directly from CMS Manuals or CMS transmittals.
Coverage Guidance
Overview Non-invasive peripheral arterial vascular studies utilize ultrasonic Doppler and physiologic studies to assess the irregularities in blood flow in arterial systems.
What is the only requirement for an ICD-10 code?
The only requirement is “ documentation ” without reference to whether an indexed code must be assigned. The “cleanest” claim would include a code for the associated diagnosis. If there is no available ICD-10 code for the associated diagnosis, an auditor will not be able to confirm it from the claim submitted and the supporting medical record information identifying the diagnosis would then have to be submitted on appeal to the auditor.
What is the term for an alteration in consciousness?
Anything that indicates an alteration in level of consciousness and responsiveness. Common ones might be encephalopathy, confusion, altered mental status, lethargy, drowsiness, obtundation, stuporous any description of decreased responsiveness, an intracranial process (e.g. trauma, hemorrhage, CVA, brain tumor),
Does "unresponsive" code to anything?
Unfortunately, "unresponsive" does not code to anything. "Unconscious" codes to R4020 Unspecified coma. You can take a look at nursing documentation perhaps, if you don't have access to the EMS run sheet.
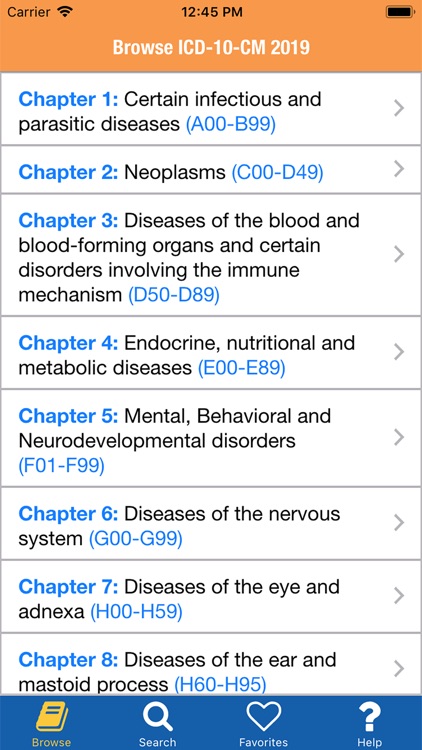
What is the convention of ICd 10?
The conventions for the ICD-10-CM are the general rules for use of the classification independent of the guidelines. These conventions are incorporated within the Alphabetic Index and Tabular List of the ICD-10-CM as instructional notes.
When to use counseling Z codes?
Counseling Z codes are used when a patient or family member receives assistance in the aftermath of an illness or injury, or when support is required in coping with family or social problems.
How many external cause codes are needed?
More than one external cause code is required to fully describe the external cause of an illness or injury. The assignment of external cause codes should be sequenced in the following priority:
What is code assignment?
Code assignment is based on the provider’s documentation of the relationship between the condition and the care or procedure, unless otherwise instructed by the classification. The guideline extends to any complications of care, regardless of the chapter the code is located in. It is important to note that not all conditions that occur during or following medical care or surgery are classified as complications. There must be a cause-and-effect relationship between the care provided and the condition, and an indication in the documentation that it is a complication. Query the provider for clarification, if the complication is not clearly documented.
When assigning a chapter 15 code for sepsis complicating abortion, pregnancy, childbirth, and the?
When assigning a chapter 15 code for sepsis complicating abortion, pregnancy, childbirth, and the puerperium, a code for the specific type of infection should be assigned as an additional diagnosis. If severe sepsis is present, a code from subcategory R65.2, Severe sepsis, and code(s) for associated organ dysfunction(s) should also be assigned as additional diagnoses.
Which code should be sequenced first?
code from subcategory O9A.2, Injury, poisoning and certain other consequences of external causes complicating pregnancy, childbirth, and the puerperium, should be sequenced first, followed by the appropriate injury, poisoning, toxic effect, adverse effect or underdosing code, and then the additional code(s) that specifies the condition caused by the poisoning, toxic effect, adverse effect or underdosing.
Do not code diagnoses documented as “probable”, “suspected,” “questionable,” “?
Do not code diagnoses documented as “probable”, “suspected,” “questionable,” “rule out ,” or “working diagnosis” or other similar terms indicating uncertainty. Rather, code the condition(s) to the highest degree of certainty for that encounter/visit, such as symptoms, signs, abnormal test results, or other reason for the visit.
Popular Posts:
- 1. icd 10 code for iliac crest bone graft
- 2. icd-10-cm code for airway disease due to cotton dust is reported with code ____.
- 3. icd 10 cm code for irregular heartbeat
- 4. icd 10 code for retinitis pigmentosa
- 5. icd 9 code for concussion with loss of consciousness lasting 10 min
- 6. icd 10 code for chf systolic
- 7. icd 9 code for adipose tissue
- 8. icd 10 cm code for hx kaposi sarcoma
- 9. icd 10 code for calcification of coronary artery
- 10. icd 9 code for decubitus ulcers