What is the latest version of ICD 10 for stroke?
The 2021 edition of ICD-10-CM I63.9 became effective on October 1, 2020. This is the American ICD-10-CM version of I63.9 - other international versions of ICD-10 I63.9 may differ. Applicable To. Stroke NOS.
What is the latest version of ICD 10 for 2021?
The 2021 edition of ICD-10-CM I63.9 became effective on October 1, 2020. This is the American ICD-10-CM version of I63.9 - other international versions of ICD-10 I63.9 may differ. A type 2 excludes note represents "not included here".
When should the stroke scale codes be sequenced?
The stroke scale codes should be sequenced after the acute stroke diagnosis code(s). At a minimum, report the initial score documented. If desired, a facility may choose to capture multiple stroke scale scores. See Section I.B.14 for NIHSS stroke scale documentation by clinicians other than patient's provider 19. Chapter 19:
What is the ICD 10 code for sunstroke?
ICD-10-CM Diagnosis Code T67.09. Other heatstroke and sunstroke. 2020 - New Code 2021 Non-Billable/Non-Specific Code. in evolution I63.9. ICD-10-CM Diagnosis Code I63.9. Cerebral infarction, unspecified. 2016 2017 2018 2019 2020 2021 Billable/Specific Code. Applicable To. Stroke NOS.
What is the ICD-10 code for a stroke?
ICD-10 | Cerebral infarction, unspecified (I63. 9)
What is the ICD-10 code for recent stroke?
Unspecified sequelae of cerebral infarction I69. 30 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM I69. 30 became effective on October 1, 2021.
What is ICD-10 code for history of stroke?
73 for Personal history of transient ischemic attack (TIA), and cerebral infarction without residual deficits is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
What is the ICD-10-CM code for ischemic stroke?
ICD-10-CM I67. 81 is grouped within Diagnostic Related Group(s) (MS-DRG v39.0): 061 Ischemic stroke, precerebral occlusion or transient ischemia with thrombolytic agent with mcc.
What's the code for stroke?
For ischaemic stroke, the main codes are ICD-8 433/434 and ICD-9 434 (occlusion of the cerebral arteries), and ICD-10 I63 (cerebral infarction).
How do you code an acute stroke?
Acute Ischemic Stroke (ICD-10 code I63.
What is the ICD-10 code for history of CVA with residual deficits?
Cognitive deficits following cerebral infarction The 2022 edition of ICD-10-CM I69. 31 became effective on October 1, 2021. This is the American ICD-10-CM version of I69. 31 - other international versions of ICD-10 I69.
How do you code chronic stroke?
How should this be coded? Answer: Assign 434.91 Occlusion of Cerebral arteries, cerebral artery occlusion, unspecified with cerebral infarction AND 431- intracerebral hemorrhage, for the description subacute ischemic right posterior parietal watershed infarct with small focus of subacute hemorrhage.
How is a stroke classified?
Stroke is classified by the type of tissue necrosis, such as the anatomic location, vasculature involved, etiology, age of the affected individual, and hemorrhagic vs. Non-hemorrhagic nature. (from Adams et al., Principles of Neurology, 6th ed, pp777-810) A stroke is a medical emergency.
How long does it take for a patient to have a hemorrhage?
Infarction or hemorrhage may be demonstrated either directly by imaging, laboratory, or pathologic examination in patients with symptom duration less than 24 hours, or inferred by symptoms lasting greater than or equal to 24 hours (or fatal within 24 hours) that cannot be attributed to another cause.
What is the term for a loss of blood flow to the brain?
An ischemic condition of the brain, producing a persistent focal neurological deficit in the area of distribution of the cerebral arteries. In medicine, a loss of blood flow to part of the brain, which damages brain tissue. Strokes are caused by blood clots and broken blood vessels in the brain.
What are brackets used for?
[ ] Brackets are used in the Tabular List to enclose synonyms, alternative wording or explanatory phrases. Brackets are used in the Alphabetic Index to identify manifestation codes.
What does NEC mean in a table?
NEC “Not elsewhere classifiable” This abbreviation in the Tabular List represents “other specified”. When a specific code is not available for a condition, the Tabular List includes an NEC entry under a code to identify the code as the “other specified” code.
What is the convention of ICd 10?
The conventions for the ICD-10-CM are the general rules for use of the classification independent of the guidelines. These conventions are incorporated within the Alphabetic Index and Tabular List of the ICD-10-CM as instructional notes.
How many external cause codes are needed?
More than one external cause code is required to fully describe the external cause of an illness or injury. The assignment of external cause codes should be sequenced in the following priority:
What are conventions and guidelines?
The conventions, general guidelines and chapter-specific guidelines are applicable to all health care settings unless otherwise indicated. The conventions and instructions of the classification take precedence over guidelines.
What is code assignment?
Code assignment is based on the provider’s documentation of the relationship between the condition and the care or procedure, unless otherwise instructed by the classification. The guideline extends to any complications of care, regardless of the chapter the code is located in. It is important to note that not all conditions that occur during or following medical care or surgery are classified as complications. There must be a cause-and-effect relationship between the care provided and the condition, and an indication in the documentation that it is a complication. Query the provider for clarification, if the complication is not clearly documented.
What does "with" mean in coding?
The word “with” or “in” should be interpreted to mean “associated with” or “due to” when it appears in a code title, the Alphabetic Index (either under a main term or subterm), or an instructional note in the Tabular List. The classification presumes a causal relationship between the two conditions linked by these terms in the Alphabetic Index or Tabular List. These conditions should be coded as related even in the absence of provider documentation explicitly linking them, unless the documentation clearly states the conditions are unrelated or when another guideline exists that specifically requires a documented linkage between two conditions (e.g., sepsis guideline for “acute organ dysfunction that is not clearly associated with the sepsis”).For conditions not specifically linked by these relational terms in the classification or when a guideline requires that a linkage between two conditions be explicitly documented, provider documentation must link the conditions in order to code them as related.
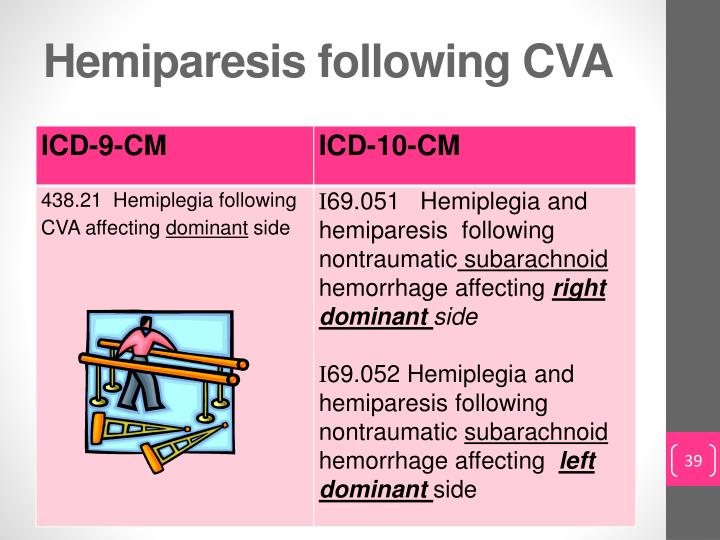
What is the ICD-10 code for stroke?
Explicitly document findings to support diagnoses of › Stroke sequela codes (ICD-10 category I69.-) should acute stroke, stroke and subsequent sequela of be used at the time of an ambulatory care visit stroke, and personal history of stroke without sequela, oce, which is considered subsequent to any acute
What is the term for a stroke that occurs when there is disruption of blood flow to brain tissue?
stroke occurs when there is disruption of blood flow to brain tissue, this leads to ischemia (deprivation of oxygen) and potentially infarction (dysfunctional scar tissue). Strokes can be either hemorrhagic, or embolic/thrombotic. Hemorrhagic strokes occur as a result of a ruptured cerebral blood vessel. Embolic/thrombic strokes occur as a result of an obstructed cerebral vessel.
How long does focal ischemic dysfunction last?
Brief reversible episodes of focal, nonconvulsive ischemic dysfunction of the brain having a duration of less than 24 hours, and usually less than one hour, caused by transient thrombotic or embolic blood vessel occlusion or stenosis.
What is a brief attack of cerebral dysfunction of vascular origin?
A brief attack (from a few minutes to an hour) of cerebral dysfunction of vascular origin, with no persistent neurological deficit. A disorder character ized by a brief attack ( less than 24 hours) of cerebral dysfunction of vascular origin, with no persistent neurological deficit.
Popular Posts:
- 1. icd 10 code for right great toe
- 2. icd 10 cm code for tonic clonic epileptic
- 3. icd 10 code for history of gout
- 4. icd 10 code for depression nos
- 5. what's the icd-10-cm code for "acute salpingitis"?
- 6. icd 10 code for neprolithisis
- 7. icd code for encounter for med refill
- 8. icd 10 code for active chronic colitis
- 9. icd-10 code for "routine annual gynecological visit and exam with pap smear"?
- 10. icd 10 code for paranoid schizophrenic patient in remission