What are the unusual ICD-10 codes?
Jul 11, 2019 · Under ICD-10 Codes that Support Medical Necessity Group 3: Codes added O99.891, O99.892, and O99.893. This revision is due to the Annual ICD-10 Code Update and is effective on 10/1/20. This revision is due to the Annual …
What is the Medicare Code for A1c?
Oct 01, 2015 · Under ICD-10 Codes That Support Medical Necessity Group 3: Codes added ICD-10 codes O24.415, O24.425 and O24.435 and the code descriptions were revised for O24.011, O24.012, O24.013, O24.019, O24.111, O24.112, O24.113, and O24.119. This revision is due to the Annual ICD-10 Code Update and becomes effective 10/1/16. Provider Education/Guidance
What are the common ICD 10 codes?
Unit Code: 16600 CPT: 83036 HgA1C D13.7 Benign neoplasm of endocrine pancreas E08.00 Diabetes mellitus due to underlying condition with hyperosmolarity without nonketotic hyperglycemic-hyperosmolar coma (NKHHC) E08.01 Diabetes mellitus due to underlying condition with hyperosmolarity with coma
What are the new ICD 10 codes?
abnormal a1c range icd-10 medicare Hcc codes medicare 2017 icd 10 diabetes with elevated a1c this is the 2017 version of the icd-10-cm diagnosis code e11.65. valid for. diabetes means your blood glucose , or blood sugar , levels are too high.. one type of test, the a1c, can also check on how you are managing your diabetes …
Does Medicare cover A1c?
Hemoglobin A1c Tests: Your doctor might order a hemoglobin A1c lab test. This test measures how well your blood glucose has been controlled over the past 3 months. Medicare may cover this test for anyone with diabetes if it is ordered by his or her doctor.
What codes will cover a A1c?
Table 1: HCPCS/CPT Codes and DescriptorsHCPCS/CPT CodesCode Descriptors82947Glucose; quantitative, blood (except reagent strip)82950Glucose; post glucose dose (includes glucose)82951Glucose Tolerance Test (GTT); three specimens (includes glucose)83036Hemoglobin A1C
Is ICD-10 covered by Medicare?
The ICD-10 transition is a mandate that applies to all parties covered by HIPAA, not just providers who bill Medicare or Medicaid.
Does Medicare cover 83036?
(2) the service must be medically necessary or indicated. Once these two criteria are met, Medicare pays for most clinical laboratory tests based on the Laboratory Fee Schedule.
How often is A1C covered by Medicare?
The A1c test, which doctors typically order every 90 days, is covered only once every three months. If more frequent tests are ordered, the beneficiary needs to know his or her obligation to pay the bill, in this case $66 per test.Jun 12, 2012
What are the ICD-10 codes for diabetes?
Common Diabetes ICD-10 Diagnosis Codes.E10.22/E11.22 Diabetes, Renal Complication.PLUS.Diabetes, Circulatory/Vascular Complication.Diabetes, Neurological Complication.E10.9. Type 1 Diabetes, w/o complication. E11.9. ... Diabetes, with other Spec. Complications.Type 1 Diabetes with Hypoglycemia.More items...
What diagnosis codes are not covered by Medicare?
Non-Covered Diagnosis CodesBiomarkers in Cardiovascular Risk Assessment.Blood Transfusions (NCD 110.7)Blood Product Molecular Antigen Typing.BRCA1 and BRCA2 Genetic Testing.Clinical Diagnostic Laboratory Services.Computed Tomography (NCD 220.1)Genetic Testing for Lynch Syndrome.More items...•Feb 9, 2022
What CPT codes are not covered by Medicare?
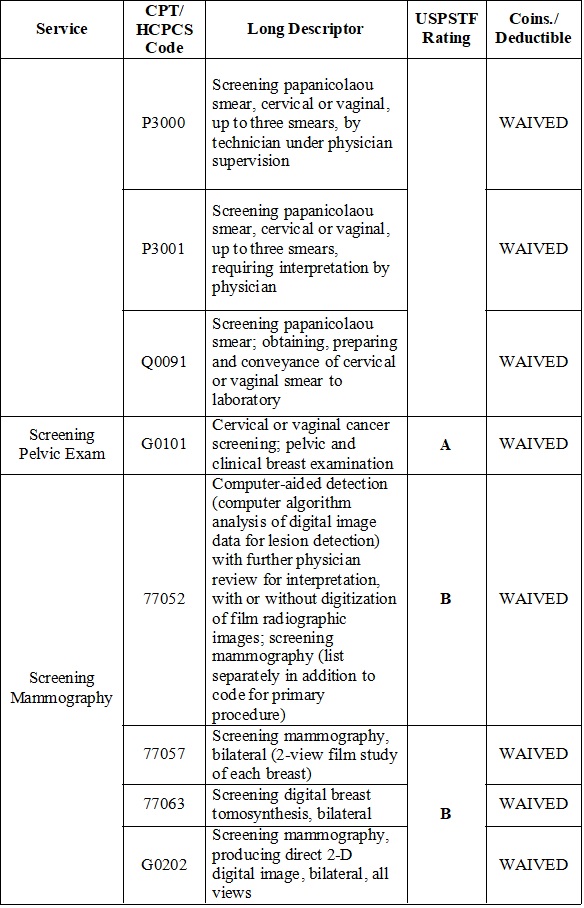
Certain services are never considered for payment by Medicare. These include preventive examinations represented by CPT codes 99381-99397. Medicare only covers three immunizations (influenza, pneumonia, and hepatitis B) as prophylactic physician services.
What ICD-10 code covers lipid panel for Medicare?
Encounter for screening for lipoid disorders 220 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM Z13. 220 became effective on October 1, 2021.
What ICD 10 covers hemoglobin A1C?
2022 ICD-10-CM Diagnosis Code R73. 09: Other abnormal glucose.
What diagnosis covers TSH for Medicare?
APPENDIX CDiagnoses Currently Covered by Medicare for Serum TSH TestingICD-9-CM CodePersistent (P), Thyroid (T), or Short-term (S)?Diagnosis244.0–244.9TAcquired hypothyroidism245.0–245.9TThyroiditis246.0–246.9TOther disorders of thyroid250.00–250.93PDiabetes mellitus153 more rows
Does diabetes qualify you for Medicare?
Medicare Part B covers screenings if your doctor determines you're at risk for diabetes. You may be eligible for up to two diabetes screenings each year. No coinsurance, copayment, or Part B deductible for screenings.Oct 2, 2017
Document Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Title XVIII of the Social Security Act, §1862 (a) (1) (A) allows coverage and payment for only those services are considered to be reasonable and necessary for the diagnosis or treatment of illness or to improve the functioning of a malformed body member.#N#CMS Internet-Only Manual, Pub.
Coverage Guidance
Hemoglobin A1c (HbA1c) refers to the major component of hemoglobin A1.#N#Performance of the HbA1c test at least 2 times a year in patients who are meeting treatment goals and who have stable glycemic control is supported by the American Diabetes Association Standards of Medical Care in Diabetes - 2016 (ADA Standards).
What is the ICD-10 code for prediabetes?
(HIPAA). The change to ICD-10 does not affect CPT coding for outpatient procedures and physician services. The ICD-10 code for prediabetes is R73.09.
What is the V77.1 code?
V77.1. To indicate that the purpose of the test (s) is diabetes screening for a beneficiary who meets the *definition of prediabetes. The screening diagnosis code V77.1 is required in the header diagnosis section of the claim and the modifier “TS” (follow-up service) is to be reported on the line item.
What is CMS coding?
Important Note: The Center s for Medicare and Medicaid Services (CMS) monitors the use of its preventive and screening benefits. By correctly coding for diabetes screening and other benefits, providers can help CMS more accurately track the use of these important services and identify opportunities for improvement.
What are the risk factors for Medicare?
Medicare beneficiaries who have any of the following risk factors for diabetes are eligible for this screening benefit: Hypertension. Dyslipidemia. Obesity ( a body mass index equal to or greater than 30 kg/m 2) Previous identification of elevated impaired fasting glucose or glucose tolerance.
Does Medicare cover behavioral therapy?
Effective in 2011, Medicare covers intensive behavioral counseling and behavioral therapy to promote sustained weight loss for Medicare beneficiaries. Many Medicare patients with prediabetes are eligible for this benefit.
What does it mean when you have a high blood glucose level?
This condition is seen frequently in diabetes mellitus, but also occurs with other diseases and malnutrition. Pre-diabetes means you have blood glucose levels that are higher than normal but not high enough to be called diabetes. Glucose comes from the foods you eat.
Can diabetes cause high blood glucose levels?
Too much glucose in your blood can damage your body over time. If you have pre-diabetes, you are more likely to develop type 2 diabetes, heart disease, and stroke.most people with pre-diabetes don't have any symptoms. Your doctor can test your blood to find out if your blood glucose levels are higher than normal.
Popular Posts:
- 1. icd 10 code for dilocated iol
- 2. icd-9 code for mayo bunionectomy
- 3. icd 10 code for acute on chronic cholecystitis with gallstomes
- 4. icd 9 code for phlegm
- 5. icd 10 code for chronic opiod
- 6. icd 10 code for adenolymphoma of right female breast
- 7. icd code for diabetic cataract
- 8. icd 10 diagnosis code for 692.9
- 9. icd 10 code for right knee meniscal tear
- 10. icd 10 code for assault gun