Full Answer
What is the total number of CPT codes?
There are a total of 249 new, 63 deleted and 93 revised CPT codes for 2022. That brings the total number of CPT codes to 10,819 per the AMA. Here is a breakdown:
What are CPT codes used for?
Specifically, CPT®codes are used to report procedures and services to federal and private payers for reimbursement of rendered healthcare. In 1966, the American Medical Association (AMA)created CPT®codes to standardize reporting of medical, surgical, and diagnostic services and procedures performed in inpatient and outpatient settings.
How to check diagnostic codes?
Things You'll Need
- Your Vehicle
- A Pen
- A Notepad
- A Computer w/ Internet
- Your Vehicle's Key
What are the CPT codes for lab tests?
Laboratory CPT Codes 86805 – 86999. Procedures for testing blood antigens and antibodies for blood transfusions during/after surgery or for testing mother/baby compatibility. Procedure codes for infusion of blood products such as fresh frozen plasma, platelets, white cells and red cells. XI.

What is a CPT category 1?
This category is usually identified with the 5-character CPT Codes that identify a service or process sanctioned by the FDA and performed by a doctor or healthcare professional. This class is broken down into six segments and they are:
What is the ICd 9 code?
CPT Codes operate along with ICD Codes. ICD-9-CM is a list of codes which correspond to investigations and procedures recorded in concurrence with hospital care in the U.S. ICD-10-M is the system used by healthcare providers and doctors to identify and code all symptoms diagnoses and procedures listed in concurrence with hospital care in the U.S.
What is an add on code?
Add-on codes are always performed in addition to the primary service or procedure and must never be reported as a stand-alone code. These codes are designated with the + symbol.
What does modifiers mean in a provider?
Providers can indicate that a service or procedure has been altered by a specific circumstance but has not changed in its definition or code. For example, modifiers may be used to report:
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Title XVIII of the Social Security Act (SSA), 1862 (a) (1) (A), states that no Medicare payment shall be made for items or services that “are not reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member.” Title XVIII of the Social Security Act, 1862 (a) (7) and 42 Code of Federal Regulations, Section 411.15, exclude routine physical examinations. Title XVIII of the Social Security Act, 1833 (e), prohibits Medicare payment for any claim lacking the necessary documentation to process the claim. CMS Manual System, Pub.
Article Guidance
Article Text The following coding and billing guidance is to be used with its associated Local coverage determination. Supportive documentation evidencing the condition and treatment is expected to be documented in the medical record and be available upon request. Documentation in the patient’s medical record must substantiate the medical necessity of the service, including the following: • A clinical diagnosis, • The specific reason for the study, • Reason for performing a stress echocardiogram as opposed to only an electrical stress test, • The reason for using any pharmacological stress, and • The reason for a stress echocardiogram if a stress nuclear test is also performed for the same patient for the same clinical condition. Document the referral order (written or verbal) in the patient’s medical record.
ICD-10-CM Codes that Support Medical Necessity
The following list of ICD-10-CM codes applies to cardiovascular stress testing CPT codes 93015, 93016, 93017, 93018, 93350, 93351 93352 and J0153. Since J0395, J1245, and J1250 may be billed for indications other than pharmacological stress agents with cardiovascular testing, the use of these drugs is not subject to the following list of ICD-10-CM diagnoses:.
ICD-10-CM Codes that DO NOT Support Medical Necessity
Any diagnosis inconsistent with the Indications and Limitations of Coverage and/or Medical Necessity section, or the ICD-10-CM descriptors in the ICD-10-CM Codes That Support Medical Necessity section.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
General Information
CPT codes, descriptions and other data only are copyright 2021 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
This article provides information regarding CPT/HCPCS codes that describe diagnostic procedures (and some materials required to perform the diagnostic procedures, i.e., radioactive tracers) that may be performed in an independent diagnostic testing facility (IDTF).
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
General Information
CPT codes, descriptions and other data only are copyright 2021 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Title XVIII of the Social Security Act, Section 1833 (e) states that no payment shall be made to any provider of services or other person under this part unless there has been furnished such information as may be necessary in order to determine the amounts due such provider or other person under this part for the period with respect to which the amounts are being paid or for any prior period.
Article Guidance
This Billing and Coding Article provides billing and coding guidance for Local Coverage Determination (LCD) L33910 Independent Diagnostic Testing Facility (IDTF). Please refer to the LCD for reasonable and necessary requirements.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
What is the billing code for a gynecologist?
CPT ® code 99072 can be utilized by all payers, although there has not been widespread acceptance. Obstetrician-gynecologists should inquire with the payers they contract with to see if they can bill 99072 for each patient seen in the office. The code is intended to be billed once per patient on the date of service, regardless how many services or physicians and health care professionals the patient encountered at that practice. For more information or to answer questions, submit a ticket.
How often is a code billed?
The code is intended to be billed once per patient on the date of service, regardless how many services or physicians and health care professionals the patient encountered at that practice. For more information or to answer questions, submit a ticket.
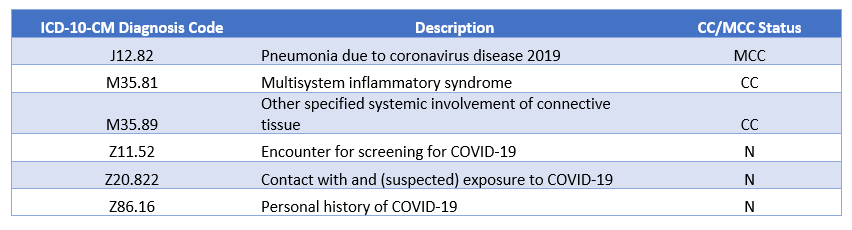
What is the code for U07.1?
Coding Rules for U07.1: U07.1 should only be used for confirmed cases of COVID-19 with positive or presumptive-positive test results. U07.1 should be sequenced first, followed by the appropriate codes for associated manifestations, except in the case of obstetrics patients. Obstetric patients with confirmed COVID-19 during pregnancy, ...
When does CMS require telehealth?
CMS requires group and individual health plans to cover visits that result in the administration of COVID-19 testing provided on or after March 18, 2020 without prior authorization or cost-sharing, including telehealth and non-traditional care settings, such as drive-through COVID-19 screening sites.
Is there a CPT code for swabbing the enduring?
There is no specific code for swabbing the enduring for COVID-19. Swab collection is included in E/M service. However, if collected in the office and transported to the laboratory, CPT code 99000 can be billed:
General Information
CPT codes, descriptions and other data only are copyright 2021 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Title XVIII of the Social Security Act, Section 1833 (e) states that no payment shall be made to any provider of services or other person under this part unless there has been furnished such information as may be necessary in order to determine the amounts due such provider or other person under this part for the period with respect to which the amounts are being paid or for any prior period..
Article Guidance
This Billing and Coding Article provides billing and coding guidance for Local Coverage Determination (LCD) L38916, Respiratory Pathogen Panel Testing.
ICD-10-CM Codes that Support Medical Necessity
It is the provider’s responsibility to select codes carried out to the highest level of specificity and selected from the ICD-10-CM code book appropriate to the year in which the service is rendered for the claim (s) submitted. The following ICD-10-CM codes support medical necessity and provide coverage for CPT codes: 87428, 87631, 87636, 87637, 0240U, 0241U when used in the outpatient setting as outlined in the related LCD..
ICD-10-CM Codes that DO NOT Support Medical Necessity
All those not listed under the “ICD-10 Codes that Support Medical Necessity” section of this article.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
What is the test technique and/or allergens tested?
The test technique and/or allergens tested must have proven efficacy demonstrated through scientifically valid medical studies published in peer-reviewed literature. Allergy testing must be performed on patients whose environment provides the reasonable probability of exposure to the specific antigen tested.
When is allergy testing covered?
Allergy testing is covered when clinically significant allergic history or symptoms that are not controllable by empiric conservative therapy exists .
What is the best test for allergy?
Percutaneous, Intradermal, Intracutaneous Testing. Percutaneous testing is the usual preferred method for allergy testing. Medicare covers percutaneous (scratch, prick or puncture) testing when IgE-mediated reactions occur to any of the following: Inhalants.
What is allergy skin test?
Allergy skin testing is a clinical procedure that is used to evaluate an immunologic response to allergenic material. The need for testing and interpretation of test findings must be correlated with signs and symptoms of possible allergies as determined by a complete history and physical examination of the patient.
What is allergy testing?
Allergy testing for antigens for which no clinical efficacy is documented in peer-reviewed literature. Such antigens include but are not limited to the following: Grain mill dust (pollen grains of cereals/related crops are large; they do not become airborne).
What is Dermatitis due to unspecified cause?
Dermatitis due to unspecified cause (692.9) is to be utilized for those patients with suspected allergic contact dermatitis but in whom the etiology is not apparent. Prior unresponsive treatments (topical medications, etc.) should be documented in the patient’s chart before initiating patch tests. Limitations.
How long does it take for a patch test to read?
The standard series of 24 patch tests or a specific allergen is applied to the skin on the patient’s back and left in place for 48 hours. The test is read after 48 hours and sometimes again after 96 hours and reactions are graded from no response (grade 0) to a blistering reaction (grade 4).
Popular Posts:
- 1. icd 9 code for peripheral arterial sclerosis
- 2. icd 10 code for history of spinal cord infarction
- 3. icd 10 cm code for gastroesophageal reflux disease
- 4. icd 10 code for seizures from hydrocephalus
- 5. icd 10 code for toxic shock syndrome
- 6. icd 9 code for ulna fx
- 7. icd 10 code for carotid arteriosclerosis
- 8. icd 10 code for ruptured left fallopian tube due to tubal pregnancy
- 9. icd 10 code for place of occurrence bathroom
- 10. icd 9 code for mixed bipolar