The following codes are the most common Pain codes used in ICD-10 G89.0 Central pain syndrome Chronic Condition G89.11 ‑ G89.18 G89.1 Acute pain, not elsewhere classified G89.21 ‑ G89.29 G89.2 Chronic pain, not elsewhere classified G89.3 Neoplasm related pain (acute) (chronic) Chronic Condition
What is the ICD 10 code for severe pain?
What is the ICD 10 code for severe pain? Pain, unspecified . R52 is a billable /specific ICD -10- CM code that can be used to indicate a diagnosis for reimbursement purposes.
What is the ICD 10 code for tailbone pain?
What is the ICD 10 code for tailbone pain? Fracture of coccyx, initial encounter for open fracture. S32.2XXB is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2019 edition of ICD-10-CM S32.2XXB became effective on October 1, 2018.
What is the CPT code for pain management?
Codes for procedures commonly used in the management of postoperative pain include 62318 and 62319 (both introduced in CPT 2000) for continuous epidural analgesia and the series of codes for somatic nerve blocks (64400-64450). It is appropriate to report pain management procedures, including the insertion of an epidural catheter or the ...
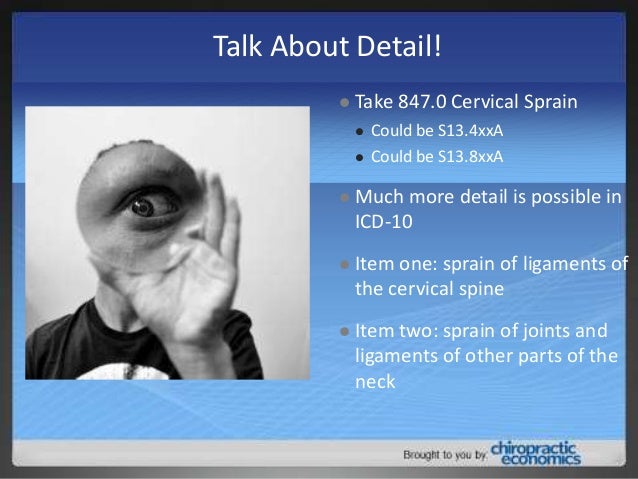
What is the ICD 10 code for neck pain?
Related Concepts SNOMET-CT
- Cervical trigger point syndrome (finding)
- Cervical facet joint pain (finding)
- Cervico-occipital neuralgia (finding)
How do you code pain?
Coding Guidelines for Pain338.0, Central pain syndrome.338.11, Acute pain due to trauma.338.12, Acute post-thoracotomy pain.338.18, Other acute postoperative pain.338.19, Other acute pain.338.21, Chronic pain due to trauma.338.22, Chronic post-thoracotomy pain.338.28, Other chronic postoperative pain.More items...
How do you code chronic pain?
NOTE: To utilize these chronic pain diagnosis codes, the exact nature of pain should be specifically documented in the patient medical records; such as “chronic” to utilize ICD-10 code G. 89.29 or the diagnosis term “chronic pain syndrome” to utilize ICD-10 code G89. 4.
What is an example of an ICD-10 code?
For example, ICD-10-CM code S31. 623A, Laceration with foreign body of abdominal wall, right lower quadrant with penetration into peritoneal cavity, initial encounter, shows an extension used with a laceration code. Note that in ICD-10-CM, the entire code description is written out.
What is the ICD-10 code for acute pain?
G89. 1 - Acute pain, not elsewhere classified | ICD-10-CM.
When do you code pain?
The ICD-10-CM guidelines state that if the cause of the pain is known, you should assign a code for the underlying diagnosis, not the pain code. However, if the purpose of the encounter is to manage the pain rather than the underlying condition, then you should assign a pain code and sequence it first.
What is the ICD-10 designation for pain?
ICD-10 code R52 for Pain, unspecified is a medical classification as listed by WHO under the range - Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified .
What is an example of medical coding?
Medical Coding Example 1 In this medical coding example, the coder receives a patient record on abscess drainage and needs to translate the information regarding the indications, medication and procedure into medical codes according to intervention radiology CPT codes.
What are some common ICD-10 codes?
Top 10 Outpatient Diagnoses at Hospitals by Volume, 2018RankICD-10 CodeNumber of Diagnoses1.Z12317,875,1192.I105,405,7273.Z233,219,5864.Z00003,132,4636 more rows
How do you write ICD-10 codes?
ICD-10-CM is a seven-character, alphanumeric code. Each code begins with a letter, and that letter is followed by two numbers. The first three characters of ICD-10-CM are the “category.” The category describes the general type of the injury or disease. The category is followed by a decimal point and the subcategory.
What is the ICD-10 code for chronic pain unspecified?
G89. 4 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
Is nociceptive pain acute or chronic?
Nociceptive pain can often be acute pain. Acute pain is a kind of short-term pain that lasts less than 3 to 6 months. It can often be caused by an injury, and it will usually go away once the injury has healed. Acute, nociceptive pain often feels different from neurological or long-term pain.
Can chronic pain be a primary diagnosis?
Only report pain diagnosis codes from the G89 category as the primary diagnosis when: The acute or chronic pain and neoplasm pain provide more detail when used with codes from other categories; or. The reason for the service is for pain control or pain management.
What is the ICd 10 code for pain?
The ICD-10-CM Official Guidelines for Coding and Reporting provide extensive notes and instruction for coding pain (category G89). Review these guidelines in full. The following summary identifies key points.#N#When seeking a pain diagnosis, identify as precisely as possible the pain’s location and/or source. If pain is the primary symptom and you know the location, the Alphabetic Index generally will provide all the information you need.#N#Only report pain diagnosis codes from the G89 category as the primary diagnosis when: 1 The acute or chronic pain and neoplasm pain provide more detail when used with codes from other categories; or 2 The reason for the service is for pain control or pain management.
How long does chronic pain last?
Chronic pain may last for months or years, and may persist even after the underlying injury has healed or the underlying condition has been treated. There is no specific timeframe identifying when you can define the pain as chronic. Determine the code assignment based on provider documentation.
What is the most important factor to consider when selecting the ICD-10 code that best describes a patient’s pain
But that golden drop of wisdom doesn’t just apply to zip codes and cross streets. For physical therapists, location is probably the most important factor to consider when selecting the ICD-10 code that best describes a patient’s pain.
Can external cause codes be used as primary diagnosis?
It sounds like you might be thinking of external cause codes. External cause codes cannot be used as the primary diagnosis code, but are often used as a supplemental code in conjunction with codes from chapter 19 (which includes injury codes). I found a list of all ICD-10 codes that cannot be used as the primary diagnosis from ...
Types of Pain
Pain can occur alone or arise from an underlying condition or injury. In order to select the correct code, it is important to first understand the terminology used to describe the type (s) of pain the patient is experiencing:
Sequencing Pain Codes
Codes that describe pain are reported and sequenced based on the encounter notes and the reason for the admission/encounter. Sometimes more than one code will need to be assigned to fully describe the type or cause of the pain documented.
Pain as Described in Chapter 6 (G89)
Only pain that falls into one of the following categories should be reported with a code from category G89.
Encounter for Pain Control or Pain Management
When a patient presents for admission/encounter for pain management the pain diagnosis code is assigned and sequenced first (reported as the first diagnosis) in the following situations:
Surgical Encounter for Pain Control
Surgical encounters are assigned diagnosis codes following the same rules. For example, a patient may undergo surgical implantation of a neurostimulator or intrathecal pain pump for pain control. In this situation, the main reason for the encounter is for pain control and not for correction of a condition or disease.
Site-Specific Pain Codes
Pain codes may also refer to a specific anatomic site (e.g., left forearm pain, right ocular pain). Codes from category G89 may be reported along with site-specific pain codes to provide a more complete description of the type of pain the patient presents with.
Postoperative Pain
There is a normal and expected degree of postoperative pain that accompanies every surgical procedure, but abnormal levels of postoperative pain may be indicative of something wrong such as an implanted device breaking or a wound reopening. Postoperative pain should be reported when it is specifically documented as such in the medical record.
Types of Pain
Pain can occur alone or arise from an underlying condition or injury. In order to select the correct code, it is important to first understand the terminology used to describe the type (s) of pain the patient is experiencing:
Sequencing Pain Codes
Codes that describe pain are reported and sequenced based on the encounter notes and the reason for the admission/encounter. Sometimes more than one code will need to be assigned to fully describe the type or cause of the pain documented.
Pain as Described in Chapter 6 (G89)
Only pain that falls into one of the following categories should be reported with a code from category G89.
Encounter for Pain Control or Pain Management
When a patient presents for admission/encounter for pain management the pain diagnosis code is assigned and sequenced first (reported as the first diagnosis) in the following situations:
Surgical Encounter for Pain Control
Surgical encounters are assigned diagnosis codes following the same rules. For example, a patient may undergo surgical implantation of a neurostimulator or intrathecal pain pump for pain control. In this situation, the main reason for the encounter is for pain control and not for correction of a condition or disease.
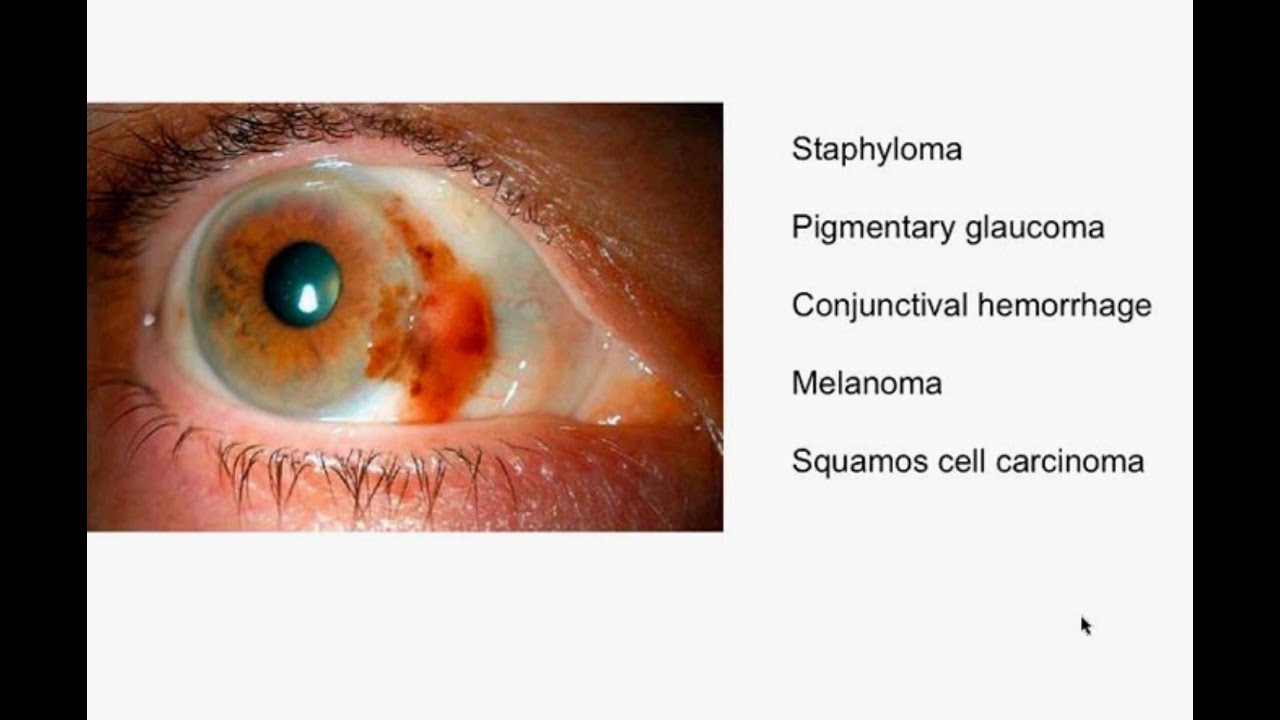
Site-Specific Pain Codes
Pain codes may also refer to a specific anatomic site (e.g., left forearm pain, right ocular pain). Codes from category G89 may be reported along with site-specific pain codes to provide a more complete description of the type of pain the patient presents with.
Postoperative Pain
There is a normal and expected degree of postoperative pain that accompanies every surgical procedure, but abnormal levels of postoperative pain may be indicative of something wrong such as an implanted device breaking or a wound reopening. Postoperative pain should be reported when it is specifically documented as such in the medical record.
What is the ICd 10 code for chronic pain?
For G89.2- Chronic pain, not elsewhere classified, the ICD-10-CM tabular list provides separate codes for pain due to trauma, post-thoracotomy pain, other postprocedural pain, and other pain. But what you won’t find is a definition for chronic. The OGs tell you that “There is no time frame defining when pain becomes chronic pain. The provider’s documentation should be used to guide use of these codes” (Section I.C.6.b.4).
When to use G89 pain code?
The general rule is that you should sequence the G89.- pain code first when the reason for the admission or encounter is pain control or pain management. Here are some examples:
Is pain coding ICd 10?
ICD-10-CM is picky about pain coding, and it’s no wonder considering all the possible variations. Fortunately you can turn to the 2019 ICD-10-CM Official Guidelines for Coding and Reporting (OGs) to keep your coding skills sharp. Today we’ll take a look at some of these pain pointers.
Popular Posts:
- 1. what is the icd 10 code for hepatic hydrothorax
- 2. icd 10 code for indwelling catheter
- 3. icd 10 code for asymptomatic covid 19 positive
- 4. what is the icd-10-cm code(s) assigned for kaposi's sarcoma of the skin due to hiv disease?
- 5. icd 10 code for effusion right knee
- 6. icd 10 code for abnormal involuntary movements
- 7. icd 10 code for contusion right elbow
- 8. icd code for left hand
- 9. icd 10 code for left hip fx
- 10. icd-9 code for sickle cell disease with crisis