For CPT code 90837 (psychotherapy, 60 minutes with patient), a physician or other qualified health care professional can report a prolonged service code if the psychotherapy service, not performed with an E/M service, is 90 minutes or longer involving direct patient contact.
Full Answer
When to use the 90837 CPT code?
While some therapists are inclined to use the 90837 for any session over 45 minutes, the AMA has defined these codes using standard rounding practices, rounding down to the 90834 for a 52 minute session, and rounding up to a 90837 for a 53 minute session.
What does CPT code 90837 stand for?
What does CPT code 90837 mean? Both 90834 and 90837 are designed to bill for the same service – psychotherapy. The primary distinguishing factor between the two codes is time; 90834 is defined as 45 minutes of psychotherapy, while 90837 is defined as 60 minutes. Likewise, who can bill CPT code 90837? Individual therapy codes (90832-90837 ...
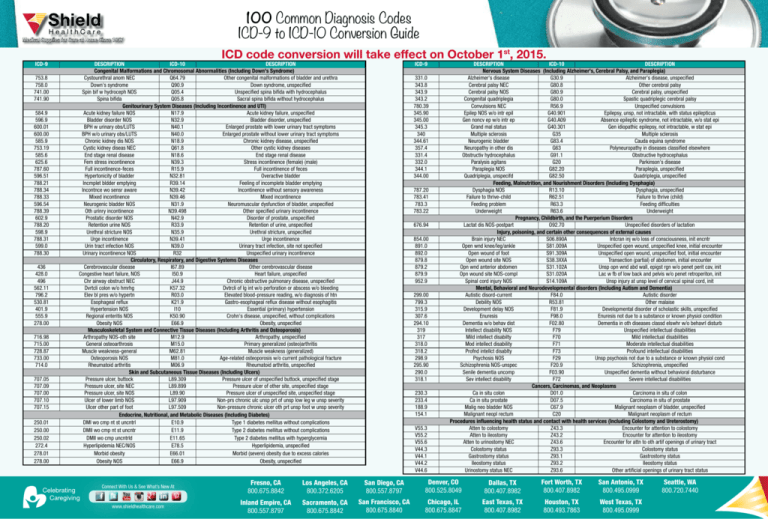
What are the new ICD 10 codes?
The new codes are for describing the infusion of tixagevimab and cilgavimab monoclonal antibody (code XW023X7), and the infusion of other new technology monoclonal antibody (code XW023Y7).
What is Procedure Code 90837?
What is procedure code 90837? CPT Code 90837 is a procedure code that describes a 60 minute individual psychotherapy session performed by a licensed mental health provider. 90837 is considered a routine outpatient CPT Code and is one of the most common CPT codes used in mental health insurance claims coding and billing.
How do you bill for extended psychotherapy?
If you are billing with CPT Code 99416, you must use CPT Code 99415. 30 minutes, Psychotherapy provided alongside evaluation and management services. 45 minutes, Psychotherapy provided alongside evaluation and management services.
Can 99354 be used with 90837?
99354 (Prolonged service[s] in the outpatient setting requiring direct patient contact beyond the time of the usual service; first hour). Procedure code 99354 can only be used in conjunction with procedure code 90837 and can only be used once an additional 30 minutes of services are provided.
Can you bill 90837?
Both 90834 and 90837 are designed to bill for the same service – psychotherapy.
What is the add-on code for 90837?
How to Bill Extended Sessions for Psychotherapy Over 60 MinutesIndividual Therapy CPT CodeAdd-On CPT Code for Extended SessionLength of Session9083216-37 minutes9083438-52 minutes9083753 - 89 minutes908379935490-134 minutes4 more rows
What modifier goes with 90837?
If you provided 60 minutes of telemedicine, you would code 90837 with modifier 95. (Note: Many clients don't have coverage for telehealth. Also, payers have previously asked providers to use the GT modifier to indicate a telehealth session, so it is a good idea to check with plans before billing).
How do you bill a prolonged service?
CPT® developed a prolonged care code, which is in the 2021 CPT®, for each additional 15 minutes of time spent on the calendar day of service. This prolonged services code is used to report total time, both with and without direct patient contact, after the time threshold for 99205 or 99215 is met.
How often can I bill 90837?
CPT code 90837 is another one of the most common CPT codes used by mental health professionals along with 90834 and 90791. Its typical use is for a normal psychotherapy session with a client. Insurers will reimburse this code only once per day, and some only as frequently as twice per week.
Is 90837 a timed code?
The Background Of The 90837 Each of these codes are timed and are well-known to many therapists, as they represent the majority of regularly billed codes, which are the 90832, 90834, and 90837. These, respectively, are described as providing individual psychotherapy for 30 minutes, 45 minutes, or 60 minutes.
How do you bill for a 90 minute psychotherapy session?
Units vs Extended Session CPT Codes Rather, what is required to bill for 90 minutes is an add-on code on a new line in box 24 of your CMS1500 form. To bill an insurance claim for a 90 minute individual therapy session: bill 90837. with add-on code 99354.
Does 90837 require a modifier?
You can use an HO modifier with all of the standard procedure codes for mental health. 90791, 90834, 90837, etc.
How do you bill for a 2 hour therapy session?
You'll want to use your typical 90837 CPT code. Then you'll also want to use the Add On CPT code 99354 which declares an additional 30 to 74 minutes of therapy. So any time you do 90 to 2 hours and 14 minutes of therapy, make sure to use the combination of CPT Codes 90837 and +99354.
How do you justify 90837?
How should I bill 90837?Psychotherapy times are for face-to-face services with the patient and/or family member.The patient must be present for all or some of the service.In reporting, choose the code closest to the actual time (i.e., 53 or more minutes for 90837).Document start and end times.
Billing Extended Sessions for Individual Therapy
It’s important to note that if you are seeing a client for 60 minutes or under, make sure to bill using CPT codes 90832, 90834, or 90837 alone.
Extended Sessions Reimbursement Rates
You can conduct an eligibility and benefits verification call to your client’s insurance company and ask specifically about coverage for those CPT codes used in conjunction with the primary code (90837 or 90847 or 90791).
Example CMS 1500 Form Coding for Extended Sessions
Please note you will need to make sure to fill in your own NPI in box 24J on the CMS-1500 form, in this example.
What is the code for prolonged therapy?
For psychotherapy sessions lasting 90 minutes or longer, the appropriate prolonged service code should be used (99354-99357). The duration of a course of psychotherapy must be individualized for each patient. Prolonged treatment may be subject to medical necessity review.
What is the procedure code for psychoanalysis?
Description: Procedure code 90845 involves the practice of psychoanalysis using special techniques to gain insight into and treat a patient’s unconscious motivations and conflicts using the development and resolution of a therapeutic transference to achieve therapeutic effect. It is a different therapeutic modality than psychotherapy.
When should a psychotherapy code not be billed?
A psychotherapy code should not be billed when the service is not primarily a psychotherapy service, that is, when the service could be more accurately described by an evaluation and management or other code. The duration of a course of psychotherapy must be individualized for each patient.
How long is 90837?
The one being addressed in this blog, is 90837, which is 53 minutes or more.
Why is 90837 necessary?
your client may have a trauma history: “90837 is medically necessary because significant trauma hx necessitates taking time to create safe space for disclosure and then containment. ”. Or: “90837 is medically necessary to address complicated diagnosis and clinical presentation.”.
How much more is 90834 than the insurance company?
Though it is not allowed to give the actual amount of payment by an insurance company because doing so violates the Sherman Antitrust Law, it is safe to say that payment is up to $30 more than what is paid for 90834. Not billing for the time you spend leaves a lot of money on the table.
When were CPT codes revised for psychotherapy?
When CPT codes for psychotherapy were revised in 2017, it became possible to bill for longer therapy sessions. The one being addressed in this blog, is 90837, 53 minutes or more. June 23, 2019 by Beth Rontal 13 Comments.
Can you bill for 90834?
Theoretically, yes. But practically, no. The CPT code is based on face-to-face time, meaning you can only bill for the time actually spent with the client. If the client is late, you need to bill at 90834 (38 – 52 minutes). Otherwise, you risk insurance fraud.
Can you use 90837 for convenience?
According to BCBS, using 90837 “cannot be for the convenience of the provider.”. This means, though specific documentation is not required, play it safe by including justification on your progress note. For example, let’s say:
Does BCBS honor 90837?
Insurance companies have been reluctant to pay for 90837 and slow to get on board so it is best to check with the company. But BCBS does honor this code and so do many other insurance companies. According to Care Paths, the denial rate for BCBS in 2017 was 1.29%, which is a down from 3 to 4% in 2013 and 2015.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
This Billing and Coding Article provides billing and coding guidance for Local Coverage Determination (LCD) L33252 Psychiatric Diagnostic Evaluation and Psychotherapy Services.
ICD-10-CM Codes that Support Medical Necessity
It is the provider’s responsibility to select codes carried out to the highest level of specificity and selected from the ICD-10-CM code book appropriate to the year in which the service is rendered for the claim (s) submitted.
ICD-10-CM Codes that DO NOT Support Medical Necessity
All those not listed under the “ICD-10 Codes that Support Medical Necessity” section of this article.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
Document Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
This LCD supplements but does not replace, modify or supersede existing Medicare applicable National Coverage Determinations (NCDs) or payment policy rules and regulations for psychiatric codes. Federal statute and subsequent Medicare regulations regarding provision and payment for medical services are lengthy. They are not repeated in this LCD.
Coverage Guidance
Compliance with the provisions in this policy may be monitored and addressed through post payment data analysis and subsequent medical review audits. History/Background and/or General Information This LCD provides guidelines for many psychiatric services. However, this LCD does not address all services, including BUT NOT LIMITED TO:
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
This article contains coding and other guidelines that complement the Local Coverage Determination (LCD) for Psychiatry and Psychology Services.
ICD-10-CM Codes that Support Medical Necessity
The correct use of an ICD-10-CM code listed below does not assure coverage of a service. The service must be reasonable and necessary in the specific case and must meet the criteria specified in the related determination.
ICD-10-CM Codes that DO NOT Support Medical Necessity
Severe and profound intellectual disabilities (ICD-10-CM codes F72, F73, and F79) are never covered for psychotherapy services or psychoanalysis (CPT codes 90832-90840, 90845-90849 and 90853). In such cases, rehabilitative, evaluation and management (E/M) codes should be reported.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
What is the status indicator for Medicare 99417?
Medicare has assigned a status indicator of invalid to code 99417, and developed a HCPCS code to replace it, G2212. If using either code, only report it with codes 99205 and 99215, use only clinician time, and use it only when time is used to select the code. There are changes to the rules for use of existing codes 99354, ...
How long does CPT take?
Not only are there different codes depending on payer, the time thresholds are different. CPT® allows you to add the 15 minutes to the lower time threshold in the range, and CMS requires you to add the 15 minutes to the higher time threshold in the range. Just a few reminders.
Is 99202 a non-face to face code?
The non-face-to-face prolonged care codes are still active, billable codes. But, they may not be reported on the same date of service as 99202—99215. If non-face-to-face prolonged care is performed by the billing practitioner on the day of an office/outpatient visit, include that in the total time for the day. See the list of activities that may be included, at the start of this article.
What is CPT code 99354?
CPT Code 99354 is a prolonged service CPT code add-on. It cannot be billed alone and must be billed with an appropriate procedure code. It fits into a sub-group of add-ons from 99354-99359 forming a subgroup of prolonged services codes.
How long is 99354?
99354 is described as an additional 30-74 minutes beyond the other CPT code. This means there is no preset time that you can bill 99354 for. So, the time of the original procedure code is important + a minimum of 30 minutes. See the 99354 time requirements section for further clarification.
How long is a 99354 session?
For mental health professionals, the 99354 is almost always billed with 90837 or 90847. 90837 is defined as 60 minutes, whereas 90847 is defined as 50 minutes. Since 99354 needs to be at least an additional 30 minutes, sessions need to be at least 30 minutes longer beyond the other procedure code. 53-89 minute session – 90837.
Can 99354 be billed by non-medical personnel?
99354 Billing Restrictions. Even though 99354 can now be billed by non-medical personnel it does not mean it is universal ly accepted. Different insurance companies may reimburse for it while others may not. Others may also require authorization.
Is 99354 a reimbursement?
99354 is not universally reimbursed and depends heavil y on the insurance company. The fee schedule often allows for reimbursement along the lines of 90837 when it is. Billing 99354 is a great way to be fairly compensated if you end up seeing clients for a much longer session.
Can you bill 99355 without 99354?
99355 cannot be billed without 99354. In the case of even longer extended sessions, you would bill 99355 as well.
Can a LCSW get 99354?
This means many Licensed Clinical Social Workers (LCSW), Licensed Professional Counselors (LPC), Licensed Marriage Family Therapist (LMFT), clinical psychologists and psychiatrists can get reimbursed with 99354. It is still not commonly known and isn’t billed very frequently, but is a great way to be compensated for extended psychotherapy sessions.
Popular Posts:
- 1. icd 10 pcs code for nasogastric tube placement
- 2. icd 10 cm code for 12 step group councling
- 3. icd 10 code for post op examination
- 4. icd 10 code for dm2 with gastroparesis
- 5. icd 10 code for l wrist fx
- 6. icd 10 code for rectus sheath hematoma
- 7. icd 10 code for allergic to aspirin
- 8. icd 10 code for alcohol hepatitis
- 9. icd 10 code for history of chromosomal abnormalities
- 10. icd 10 code for dorsal somatic dysfunction