What is the CPT code for bandage lenses?
▸ V2599: Contact lens, other type, per lens. (This code is used for intralimbal lenses, etc.) The supply code is billed separately; however, Medicare identifies 99070 as always bundled with the associated code, so there is no separate payment for the bandage contact lens.
Can You bill for bandage lenses?
You can bill for the bandage lens material as well, provided you are not using a trial lens from your inventory. You should also keep in mind that for most presentations there is no difficulty in billing both the office visit and the bandage contact lens fit on the same date of service.
What is the ICD 10 code for contact lens injury?
Z46.0 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. Short description: Encounter for fit/adjst of spectacles and contact lenses.
What are the “V” codes for contact lenses?
Other “V codes” include: ▸ V2599: Contact lens, other type, per lens. (This code is used for intralimbal lenses, etc.) The supply code is billed separately; however, Medicare identifies 99070 as always bundled with the associated code, so there is no separate payment for the bandage contact lens.
Does Medicare cover bandage contact lenses?
However, Medicare does cover bandage contact lenses (BCL) that are used for therapeutic purposes -- e.g., to promote healing or for pain management.
How do I bill my contact lens fitting?
Use CPT 92310, which is defined as: “Prescription of optical and physical characteristics of and fitting of contact lens, with medical supervision of adaptation; corneal lens, both eyes, except for aphakia.” Note that CPT 92310 is for both eyes.
What is a bandage contact lens?
A bandage contact lens is designed to protect an injured or diseased cornea from the mechanical rubbing of the blinking eyelids, therefore allowing it to heal. The Bandage lens often makes the eye feel more comfortable. It is usually a soft lens, but not always. The lens has no focusing power.
How do you code medically necessary contacts?
CPT Codes CPT codes are used to bill the fitting portion during the medically necessary contact lens fitting....WHAT QUALIFIES AS A MEDICALLY NECESSARY CONTACT LENS?CODEDESCRIPTIONV2510Contact Lens, GP, Spherical, Per LensV2511Contact Lens, GP, Toric, Per Lens10 more rows•Feb 1, 2020
Does medical cover contact fitting?
Contact Lens Examination In addition to the basic eye examination, a contact lens fitting is reimbursable with CPT® codes 92071, 92072 and 92310 thru 92312 for recipients with medically necessary conditions.
What is code V2510?
HCPCS code V2510 for Contact lens, gas permeable, spherical, per lens as maintained by CMS falls under Assorted Contact Lenses .
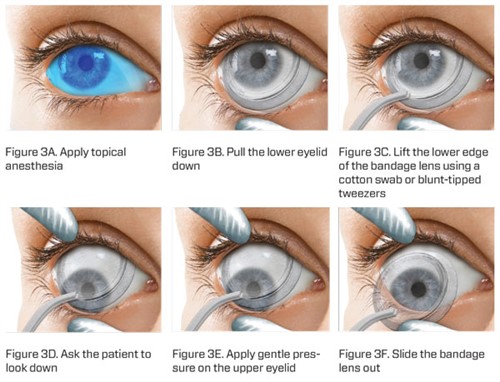
How do you apply bandage to contact lenses?
Methods: The bandage contact lens is picked up with the nozzle of the Minims by suction. The lens is then taken to the patient, placed on the cornea, and released by breaking the vacuum. Results: Examination of the contact lens under the microscope after insertion showed no damage.
Which contact lenses are used for a bandage on the cornea?
Bandage contact lenses (BCL) or therapeutic contact lenses (TCL) are distinct from cosmetic lenses. They are sometimes worn after injury, disease or surgery to protect the cornea, relieve pain and improve the ability of the corneal epithelium to heal.
How long can I wear bandage contact lens?
Bandage lenses must be used until the epithelial adhesion complex has fully recovered—at least 2 months. These lenses may also improve small irregularities of the ocular surface, which can in turn improve visual acuity.
What is the difference between medically necessary and elective contacts?
Non-elective contact lenses, also called medically necessary contact lenses, are prescribed by your optometrist to correct these types of eye problems, whereas elective contacts are chosen by the patient to correct an eye issue that eyeglasses or sometimes laser surgery can also correct.
What are medically necessary lenses?
Medically necessary contact lenses are non-elective contact lenses prescribed when certain medical conditions hinder vision correction through regular eyeglasses and contact lenses are the accepted standard of treatment.
How do I bill medically necessary contacts to VSP?
In order to verify what VSP considers medically necessary, log in and scroll down to visually necessary contact lenses (NCLs) under “plans and coverage” in the “manuals” section. Specific eye conditions can be corrected only with contact lenses.
What is the procedure code for biological bandages?
Therefore, they are not bandage contact lenses and should be not be billed as such. The procedure code that describes these bandages is 65778, or “placement of amniotic membrane on the ocular surface for wound-healing; self-retaining.”.
Is a bandage necessary for corneal abrasion?
There are many different clinical presentations that we encounter, such as corneal abrasions, in which a bandage contact lens is necessary, compared with an exposure keratopathy case, in which a biological bandage can provide improved clinical outcomes.
Does Medicare cover bandages for contact lenses?
By Suzanne L. Corcoran, COE. As you know , Medi-care won't separately reimburse contact lenses that you prescribe to correct refractive error (except for aphakic and pseudo-phakic patients), and other third-party payers only offer limited coverage. However, Medicare does cover bandage contact lenses ...
Does Medicare cover BCL?
However, Medicare does cover bandage contact lenses (BCL) that are used for therapeutic purposes -- e.g., to promote healing or for pain management. During the year 2000, Medicare paid about 18,000 claims for BCLs out of a universe of approximately 24 million eye exams.
Can Medicare deny 92070?
If you bill for 92070 more than once a month per patient, Medicare may deny your claim. In this case, get the patient's signature on an Advanced Beneficiary Notice (ABN) indicating that the patient accepts financial responsibility in the event of a denial, before dispensing the BCL.
Is 92070 billed in the operating room?
The facility fee of the ASC or hospital includes this, so you shouldn't charge 92070 as an adjunct to the surgical procedure. Also, BCLs dispensed in the office to aid in post-surgery recovery are not separately billed or reimbursed.
What is bandage contact lens?
Q What is a bandage contact lens? A contact lens usually contains an optical correction for ammetropia for use in lieu of eyeglasses. Except for postcataract lenses, Medicare doesn't separately reimburse contact lenses prescribed for refractive errors.
What is an ABN for a bandage?
Get the patient's signature on an Advanced Beneficiary Notice (ABN) before dispensing the lens, indicating that the patient accepts financial responsibility in the event of a denial. The ABN must include a brief description of the bandage contact lens and the reason why you expect a denial from Medicare.
Does Medicare cover hydrophilic contact lenses?
The term "hydrophilic contact lens" doesn't include corneal collagen shields as banda ge contact lenses and several Medicare policies specifically preclude coverage of collagen lenses. The Indications and Limitations of Coverage listed in the NCD provides special instructions about reimbursement for bandage contact lenses.
Does Medicare cover more than one lens?
For example, "Medicare doesn't cover more than one replacement lens per month.". During 2000, Medicare paid about 18,000 claims for 92070 out of a universe of approximately 24 million eye exams. CPT code 92070 is probably underused because of the confusion related to coverage policy and billing.
Is hydrophilic contact lens included in the payment for the physician's service?
Payment for the lens is included in the payment for the physician's service to which the lens is incident.".
Does the FDA cover bandage lenses?
However, it does cover bandage contact lenses used for therapeutic purposes. The Food and Drug Administration (FDA) approves only certain lenses as bandage lenses. Current Procedural Terminology lists 92070 (fitting of contact lens for treatment of disease, including supply of lens). Note that this is per eye.
What is the insurance code for contact lens fitting?
Most vision insurances are billed this way. They usually accept a contact lens fitting code (9231X) as one fee, then the V codes as another fee.
What is the ICd 10 code for corneal transplant?
An example may look like this: 1 Jane Doe, 1-1-2001, ID# 1234, Plan XYZ 2 Diagnosis: corneal transplant status, ICD 10 code Z94.7 3 CPT code (s): 92310 (Prescription of Optical and Physical Characteristics of and Fitting of Contact Lens, with Medical Supervision of Adaptation; Corneal Lens, Both Eyes, Except for Aphakia) 4 V code (s): V2511-RT and V2511-LT (contact lens, GP, toric, per lens) 5 Usual and customary rate: $500 for 92310, $250 for V2511-RT, and $250 for V2511-LT 6 Patient has met his or her deductible in full; the co-pay for medically necessary contact lens services and materials is $25 7 The expected reimbursement from the insurance based on diagnosis code, CPT code, V codes, and allowed amounts is $400 total, according to Mary at Insurance Company A.
How to bill specialty lenses?
Step 1 The first step for specialty lens billing is to contact a patient’s insurance (vision and/or medical) and obtain a prior authorization for medically necessary contact lens coverage. This may not occur until after you see patients, so often it cannot be done prior to their appointment.
What is balance billing in insurance?
Balance billing means that it is acceptable to bill the remaining difference to the patient; in this case, the U+C is $1,000 and the insurance payment is $400, so the difference would be $600.
What is billing and coding?
Billing and coding are a source of frustration for both practitioners and patients. Reimbursement methods and rates vary drastically between carriers and even sometimes between patients. Often, it is difficult to obtain a clear answer on what the proper method is, what codes to use, and how to determine coverage.
Do you need prior authorization for contact lenses?
This is very typical, and each insurance has a different contracted rate. This is why it is so important to obtain prior authorizations before fitting medically necessary lenses. As the practitioner, you should be fully aware of the expected reimbursement prior to initiating any contact lens fitting.
What does the 7th character mean in ICD-10?
The seventh character indicates the status of the injury and care. “A” would indicate that this is the initial visit, and the patient is under active management.
Can you bill for a bandage lens?
You can bill for the bandage lens material as well, provided you are not using a trial lens from your inventory. You should also keep in mind that for most presentations there is no difficulty in billing both the office visit and the bandage contact lens fit on the same date of service.
Is bandage contact lens good?
For many patients, a bandage contact lens is an excellent treatment approach; it can provide protection during the healing process, relieve pain and protect the ocular surface. While the clinical presentation and treatment regimen may seem straightforward, the coding for it may not be.

Popular Posts:
- 1. icd 10 code for dislocated ribs
- 2. icd 10 code for aphagia
- 3. icd 10 code for medical neuropsychological evaluation
- 4. icd 10 code for prostatic stone
- 5. icd 10 code for driver of special construction vehicle injured in traffic accident
- 6. icd 10 code for hfe
- 7. icd 10 code for allergen injections
- 8. icd 10 cm code for brain tumor
- 9. icd 10 code for abscess left inguinal region
- 10. icd 10 code for right nose lesion