What is the ICD 10 code for severe pain?
What is the ICD 10 code for severe pain? Pain, unspecified . R52 is a billable /specific ICD -10- CM code that can be used to indicate a diagnosis for reimbursement purposes.
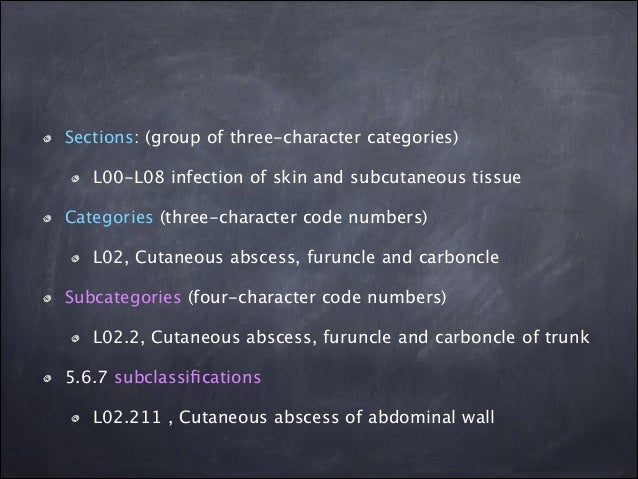
What is the ICD 10 diagnosis code for?
The ICD-10-CM is a catalog of diagnosis codes used by medical professionals for medical coding and reporting in health care settings. The Centers for Medicare and Medicaid Services (CMS) maintain the catalog in the U.S. releasing yearly updates.
What is ICD 10 code for abdominal pain?
ICD 10 Code for Abdominal Pain is R10.0 is a billable ICD-10 code used for healthcare diagnosis reimbursement of acute abdomen. Related Articles: ICD10 codes in medical billing. Categories ICD Codes, Medical Billing Codes Tags icd 10 abdominal pain, icd 10 code for abdominal pain Post navigation.
How do you code acute exacerbation of chronic abdominal pain?
coding acute and chronic pain
- 338.0, Central pain syndrome
- 338.1X, Acute pain
- 338.2X, Chronic pain
- 338.3, Neoplasm-related pain (acute) (chronic)
- 338.4, Chronic pain syndrome
- 780.96, Generalized pain–used when the site of the pain is not specified General Coding Information Codes in category 338 may be used in conjunction with other codes to provide more ...
What is the ICD-10-CM code for pain management?
R52 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM R52 became effective on October 1, 2021. This is the American ICD-10-CM version of R52 - other international versions of ICD-10 R52 may differ.
What is the ICD-10 code for unspecified pain?
ICD-10 code R52 for Pain, unspecified is a medical classification as listed by WHO under the range - Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified .
What is the ICD-10-CM code for chronic pain?
NOTE: To utilize these chronic pain diagnosis codes, the exact nature of pain should be specifically documented in the patient medical records; such as “chronic” to utilize ICD-10 code G. 89.29 or the diagnosis term “chronic pain syndrome” to utilize ICD-10 code G89. 4.
What is the ICD-10 code for intractable pain?
G89. 4 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
How do you code Acute on chronic pain?
Coding Guidelines for Pain338.0, Central pain syndrome.338.11, Acute pain due to trauma.338.12, Acute post-thoracotomy pain.338.18, Other acute postoperative pain.338.19, Other acute pain.338.21, Chronic pain due to trauma.338.22, Chronic post-thoracotomy pain.338.28, Other chronic postoperative pain.More items...
What is I10 diagnosis?
ICD-Code I10 is a billable ICD-10 code used for healthcare diagnosis reimbursement of Essential (Primary) Hypertension.
Can chronic pain be a primary diagnosis?
Only report pain diagnosis codes from the G89 category as the primary diagnosis when: The acute or chronic pain and neoplasm pain provide more detail when used with codes from other categories; or. The reason for the service is for pain control or pain management.
How many codes do you need to use when coding for both acute and chronic phases of a single condition?
Multiple coding for a single condition In addition to the etiology/manifestation convention that requires two codes to fully describe a single condition that affects multiple body systems, there are other single conditions that also require more than one code.
What is considered severe chronic pain?
Your body keeps hurting weeks, months, or even years after the injury. Doctors often define chronic pain as any pain that lasts for 3 to 6 months or more.
What is the ICd 10 code for pain?
The ICD-10-CM Official Guidelines for Coding and Reporting provide extensive notes and instruction for coding pain (category G89). Review these guidelines in full. The following summary identifies key points.#N#When seeking a pain diagnosis, identify as precisely as possible the pain’s location and/or source. If pain is the primary symptom and you know the location, the Alphabetic Index generally will provide all the information you need.#N#Only report pain diagnosis codes from the G89 category as the primary diagnosis when: 1 The acute or chronic pain and neoplasm pain provide more detail when used with codes from other categories; or 2 The reason for the service is for pain control or pain management.
How long does chronic pain last?
Chronic pain may last for months or years, and may persist even after the underlying injury has healed or the underlying condition has been treated. There is no specific timeframe identifying when you can define the pain as chronic. Determine the code assignment based on provider documentation.
What is the meaning of pain?
Pain is a feeling triggered in the nervous system. Pain may be sharp or dull.
How long does pain last?
Once you take care of the problem, pain usually goes away. However, sometimes pain goes on for weeks, months or even years.
What is the pain of the coccyx?
Pain of coccyx greater than 3 months, chronic. Clinical Information. A disorder characterized by the sensation of marked discomfort, distress or agony. An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons.
What is pain in the nervous system?
Intensely discomforting, distressful, or agonizing sensation associated with trauma or disease, with well-defined location, character, and timing. Pain is a feeling triggered in the nervous system. Pain may be sharp or dull. It may come and go, or it may be constant.
What does it mean to feel pain?
Sensation of unpleasant feeling indicating potential or actual damage to some body structure felt all over, or throughout the body. Severe pain of limited duration. The sensation of discomfort, distress, or agony, resulting from the stimulation of specialized nerve endings.
How long does pain last without pain?
Once you take care of the problem, pain usually goes away. However, sometimes pain goes on for weeks, months or even years. This is called chronic pain.
What is a disorder characterized by the sensation of marked discomfort, distress or agony?
An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Causing physical or psychological misery, pain or distress. Intensely discomforting, distressful, or agonizing sensation associated with trauma or disease, ...

Popular Posts:
- 1. icd 9 code for encephalopathy
- 2. what is the icd 10 code for hypercapnia
- 3. icd 10 code for enlarged testes
- 4. icd 10 cm code for bilateral hearing loss
- 5. icd 10 code for tick bite
- 6. icd 10 code for pleurx catheter drainage
- 7. icd 10 dx code for small cell carcinoma lung with brain mets
- 8. icd 9 code for forearm rash
- 9. icd 10 code for 15 weeks pregnant
- 10. icd 10 code for pruitits