What is the ICD 10 code for lumbar degeneration?
Other intervertebral disc degeneration, lumbar region. M51.36 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
What is the ICD 10 code for pyogenic discitis of lumbar spine?
Pyogenic disc inflammation of lumbar spine; Pyogenic discitis of lumbar spine; Pyogenic infection of lumbar intervertebral disc ICD-10-CM Diagnosis Code M51.06 [convert to ICD-9-CM] Intervertebral disc disorders with myelopathy, lumbar region
What is the ICD 10 code for lumbar spinal stenosis?
2018/2019 ICD-10-CM Diagnosis Code M48.06. Spinal stenosis, lumbar region. M48.06 should not be used for reimbursement purposes as there are multiple codes below it that contain a greater level of detail.
What is the correct ICD-10 code for disc disorders?
Selecting the correct ICD-10 code for disc disorders can take a little bit of research. There are many options found in the M50 and M51 categories, which are: M51- Thoracic, Thoracolumbar, and Lumbosacral Intervertebral Disc Disorders The fifth character provides detail about the anatomical location within the spinal region.
What is the ICD 10 code for DDD lumbar?
ICD-10-CM Code for Other intervertebral disc degeneration, lumbar region M51. 36.
How do you code degenerative disc disease?
Codes in subcategory M51. 3, Other thoracic, thoracolumbar and lumbosacral intervertebral disc degeneration, are specific to vertebral regions. ... To read the full article, sign in and subscribe to AHA Coding Clinic® for ICD-10-CM and ICD-10-PCS .
What is the ICD 10 code for degenerative changes?
According to Coding Clinic: “Assign code M16. 0—Bilateral primary osteoarthritis of hip for degenerative changes of hips”. Coding Clinic's rationale is, “ICD-10- CM's Alphabetic Index under “Degeneration, joint disease” instructs “see Osteoarthritis.”
What does code M51 36 mean?
36 Other intervertebral disc degeneration, lumbar region.
What is the ICD-10-CM code for degenerative disc disease?
Other intervertebral disc degeneration, lumbar region M51. 36 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM M51. 36 became effective on October 1, 2021.
Is DDD the same as osteoarthritis?
Degenerative joint disease is just another name for osteoarthritis, which is the most common type of arthritis – and it occurs when the components of a joint wear down. So whether we call it degenerative joint disease, osteoarthritis, or arthritis, we're really talking about the same condition.
What is the ICD-10 code for chronic back pain?
ICD-10 Code M54. 5 for Chronic Low Back Pain | CareCloud.
What is the ICD-10 code for degenerative arthritis?
Unspecified osteoarthritis, unspecified site The 2022 edition of ICD-10-CM M19. 90 became effective on October 1, 2021. This is the American ICD-10-CM version of M19. 90 - other international versions of ICD-10 M19.
What is the ICD-10 code for back pain?
ICD-10 code M54. 5, low back pain, effective October 1, 2021. That means providers cannot use M54. 5 to specify a diagnosis on or after October 1—and existing patients with the M54.
What does lumbar DDD mean?
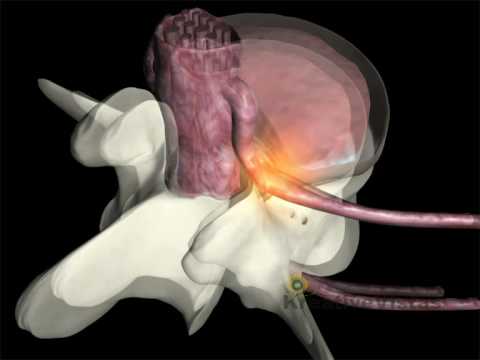
Degenerative disc disease (DDD) affects the discs that separate the spine bones. As you age, the spine begins to show signs of wear and tear as the discs dry out and shrink. These age-related changes can lead to arthritis, disc herniation, or spinal stenosis. Pressure on the spinal cord and nerves may cause pain.
What is degenerative lumbar spine?
Degenerative disc disease in the lumbar spine, or lower back, refers to a syndrome in which age-related wear and tear on a spinal disc causes low back pain. Lumbar Degenerative Disc Disease Video. When damaged discs in the lumbar spine cause symptoms of pain, it is called lumbar degenerative disc disease.
What diagnosis is M51 26?
M51. 26 Other intervertebral disc displacement, lumbar region - ICD-10-CM Diagnosis Codes.
Is degenerative disc disease and degenerative joint disease the same thing?
Degenerative disc disease or DDD can be the cause of many different symptoms resulting in localized pain or pain that radiates down the leg. Degenerative joint disease or DJD is very different, but can have overlapping symptoms with DDD.
What is the ICD-10 code for chronic back pain?
ICD-10 Code M54. 5 for Chronic Low Back Pain | CareCloud.
Is degenerative disc disease a joint disease?
Degenerative Joint Disease is most commonly know as Osteoarthritis. Similar to Degenerative Disc Disease, with Degenerative Joint Disease, the 'cushion' of cartilage between the joints beings to deteriorate. The joints most commonly affected by DJD are the knees, followed by the hips, hands and spine.
Is Spondylosis the same as DDD?
Degenerative Disc Disease (DDD), also known as Spondylosis, is a condition that usually occurs due to aging. As the term implies, it is the progressive deterioration of the discs between the vertebral bodies.
What is the T12-L1 code?
Though it is not specifically mentioned, “thoracolumbar” likely only includes T12-L1, and “lumbosacral” probably only refers to the L5-S1 interspace. There is a strange rule for cervical disc disorders indicating that you should code to the most superior level of the disorder.
What is the difference between radiculopathy and myelopathy?
Myelopathy means that there is some sort of neurologic deficit to the spinal cord, whereas radiculopathy means that there is a deficit to nerve roots. Don’t code radiculitis (M54.1-) separately if you use thefourth character of “1” with radiculopathy for the disc disorders (M50.1- or M51.1-). It is already included in the code.
Is sciatica a code for lumbar radiculopathy?
It is already included in the code. Likewise, don’t code sciatica (M54.3-) if you code for lumbar disc with radiculopathy. It would be redundant. On a side note, lumbar radiculopathy (M54.16) might be used if pain is not yet known to be due a disc, but it radiates from the lumbar spine.

Popular Posts:
- 1. icd 10 code for gerd with dysphagia
- 2. icd 10 code for cardio hyn
- 3. icd 10 code for well child exam
- 4. icd-10 code for callus
- 5. icd 10 code for left ankle pain unspecified
- 6. icd 10 code for ibs unspecified
- 7. icd 10 code for bullae left foot
- 8. icd 10 code for history of allergy to pollen
- 9. icd 10 exernal cause code for blunt trauma
- 10. icd 10 code for ac joint arthropathy