What blood test is used to confirm a HIV diagnosis?
- A nucleic acid test (NAT) can usually tell you if you have HIV infection 10 to 33 days after an exposure.
- An antigen/antibody test performed by a laboratory on blood from a vein can usually detect HIV infection 18 to 45 days after an exposure. ...
- Antibody tests can take 23 to 90 days to detect HIV infection after an exposure. ...
Is HIV test conclusive at 14 weeks?
Yes, conclusive: These tests are conclusive any time 6 weeks or more after the last possible exposure. Don't have any more tests unless and until you may be reexposed.
Should I have a HIV test?
The only way to know for sure whether you have HIV is to get tested. CDC recommends that everyone between the ages of 13 and 64 get tested for HIV at least once as part of routine health care. Knowing your HIV status gives you powerful information to help you take steps to keep you and your partner (s) healthy.
Does a VDRL test detect HIV infection?
Not really, it is not recommended to test the HIV infections. The venereal disease research laboratory (VDRL) test is designed to assess whether or not you have syphilis, a sexually transmitted infection (STI). Syphilis is caused by the bacteria Treponema pallidum. The bacteria infects by penetrating into the lining of the mouth or genital area.

What is the code for inconclusive HIV test?
Code 795.8 was intended for inconclusive HIV test results, whereas code 044.9 was intended for asymptomatic HIV infection (or a statement of "HIV positive").
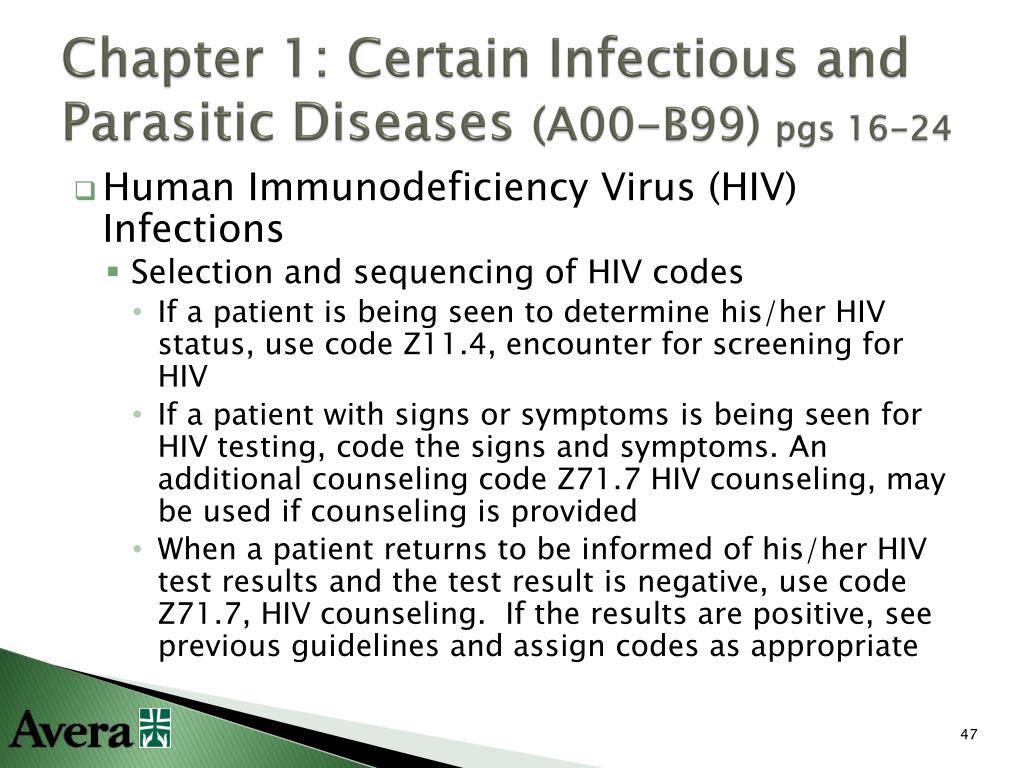
What ICD-10 code covers HIV testing?
Z11. 4 Encounter for screening for human immunodeficiency virus (HIV).
What is the ICD-10-CM codes for HIV positive without any other symptoms?
Answer: Following ICD-10 guidelines, a patient with HIV status without symptoms is coded with Z21, positive HIV status. Some doctors and non-physician practitioners would prefer to use B20. According to ICD-10, B20 is used when the patient has confirmed AIDS.
How do you code HIV test?
Test product. 86701 with modifier 92 for the antibody HIV-1. test.or. 86703 with modifier 92 for the antibody HIV-1. and HIV-2 single assay.or. 87390 with modifier 92 for the infectious agent. antigen detection by enzyme immunoassay.
When do you code B20 and Z21?
Once a patient is coded to B20, they will always have B20 coded on their record; they will never go back to being coded using the asymptomatic code Z21. Code Z21 is used for patients who are asymptomatic, meaning they are HIV positive but have never had an HIV-related condition.
What does the code Z11 4 mean?
The description for diagnosis code Z11. 4 is “Encounter for screening for human immunodeficiency virus [HIV].
What is the sequence for HIV?
Sequencing. The proper sequencing for HIV depends on the reason for the admission or encounter. When a patient is admitted for an HIV-related condition, sequence B20 Human immunodeficiency virus [HIV] disease first, followed by additional diagnosis codes for all reported HIV-related conditions. Conditions always considered HIV-related include ...
What condition must be confirmed to select the code?
In the inpatient setting, HIV is the only condition that must be confirmed to select the code. All other conditions documented as “probable,” suspected,” likely,” “questionable,” “probable,” or “still to rule out” are coded as if they exist in the inpatient setting. Dx. Sequencing. The proper sequencing for HIV depends on the reason for ...
Is HIV a diagnosis?
HIV infection/illness is coded as a diagnosis only for confirmed cases. Confirmation does not require documentation of a positive blood test or culture for HIV; the physician’s diagnostic statement that the patient is HIV positive or has an HIV-related illness is sufficient. In the inpatient setting, HIV is the only condition ...
What is postpartum HIV?
Clinical Information. Development of neutralizing antibodies in individuals who have been exposed to the human immunodeficiency virus (hiv/htlv-iii/lav). Infected with the human immunodeficiency virus (hiv), the cause of acquired immunodeficiency syndrome (aids).
What does "type 1 excludes note" mean?
It means "not coded here". A type 1 excludes note indicates that the code excluded should never be used at the same time as Z21. A type 1 excludes note is for used for when two conditions cannot occur together, such as a congenital form versus an acquired form of the same condition. acquired immunodeficiency syndrome (.
What does the title of a manifestation code mean?
In most cases the manifestation codes will have in the code title, "in diseases classified elsewhere.". Codes with this title are a component of the etiology/manifestation convention. The code title indicates that it is a manifestation code.
What is the late phase of HIV?
One or more indicator diseases, depending on laboratory evidence of hiv infection (cdc); late phase of hiv infection characterized by marked suppression of immune function resulting in opportunistic infections, neoplasms, and other systemic symptoms (niaid). rheumatoid arthritis ( M05.-)
What are the most common infections in patients with aids?
Patients with aids are especially susceptible to opportunistic infections (usually pneumocystis carinii pneumonia, cytomegalovirus (cmv) infections, tuberculosis, candida infections, and cryptococcosis), and the development of malignant neoplasms (usually non-hodgkin's lymphoma and kaposi's sarcoma).
What is immunodeficiency syndrome?
Clinical Information. A disease caused by human immunodeficiency virus (hiv). People with acquired immunodeficiency syndrome are at an increased risk for developing certain cancers and for infections that usually occur only in individuals with a weak immune system.
What is CD4 positive?
An acquired defect of cellular immunity associated with infection by the human immunodeficiency virus (hiv), a cd4-positive t-lymphocyte count under 200 cells/microliter or less than 14% of total lymphocytes, and increased susceptibility to opportunistic infections and malignant neoplasms.
What is Z16.- code?
code to identify resistance to antimicrobial drugs ( Z16.-) A disease caused by human immunodeficiency virus (hiv). People with acquired immunodeficiency syndrome are at an increased risk for developing certain cancers and for infections that usually occur only in individuals with a weak immune system.
What is a type 1 exclude note?
A type 1 excludes note indicates that the code excluded should never be used at the same time as B20. A type 1 excludes note is for used for when two conditions cannot occur together, such as a congenital form versus an acquired form of the same condition.
What does the title of a manifestation code mean?
In most cases the manifestation codes will have in the code title, "in diseases classified elsewhere.". Codes with this title are a component of the etiology/manifestation convention. The code title indicates that it is a manifestation code.
Popular Posts:
- 1. icd 10 code for fell out of bed
- 2. icd-10 code for impella device
- 3. icd 10 code for bipolar d/o
- 4. icd-10 code for delayed union right humerus shaft fracture
- 5. icd 9 code for history of mva
- 6. icd 10 code for hidradenitis of thighs
- 7. icd 10 code for fracture of thoracic spine
- 8. icd-10 code for chronic renal transplant insufficiency
- 9. icd 10 code for right hand laceration with foreign body
- 10. icd 10 code for intentional diphenhydramine overdose