What is the ICD 10 code for diagnosis Q90?
Q90.2 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2018/2019 edition of ICD-10-CM Q90.2 became effective on October 1, 2018. This is the American ICD-10-CM version of Q90.2 - other international versions of ICD-10 Q90.2 may differ.
What is the ICD 10 code for trisomy 10?
ICD-10-CM Diagnosis Code Q92.9. Trisomy and partial trisomy of autosomes, unspecified. 2016 2017 2018 2019 2020 2021 Billable/Specific Code POA Exempt. 21 Q90.9. ICD-10-CM Diagnosis Code Q90.9. Down syndrome, unspecified. 2016 2017 2018 2019 2020 2021 Billable/Specific Code POA Exempt.
What is the latest version of ICD 10 for adults?
The 2022 edition of ICD-10-CM R62.7 became effective on October 1, 2021. This is the American ICD-10-CM version of R62.7 - other international versions of ICD-10 R62.7 may differ. R62.7 is applicable to adult patients aged 15 - 124 years inclusive.
What is the ICD 10 code for fracture of T11 T12?
Fracture of T11-T12 vertebra. S22.08 should not be used for reimbursement purposes as there are multiple codes below it that contain a greater level of detail. The 2019 edition of ICD-10-CM S22.08 became effective on October 1, 2018. This is the American ICD-10-CM version of S22.08 - other international versions of ICD-10 S22.08 may differ.
What is DRG #640-641?
What is the ICD code for failure to thrive?
What is billable code?
What does "type 1 excludes" mean?
What is inclusion term?
About this website

What is ICD-10 code for neonatal weight loss?
As there is no specific code in the perinatal chapter for this code the only code option is R63. 4 Abnormal weight loss. If the condition >10% loss of birth weight is documented and intervention is undertaken then assign R63. 4 Abnormal weight loss.
What is diagnosis Z71 9?
ICD-10 code Z71. 9 for Counseling, unspecified is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
What is diagnosis code N64 4?
ICD-10 code N64. 4 for Mastodynia is a medical classification as listed by WHO under the range - Diseases of the genitourinary system .
What is ICD-10 code W19?
Unspecified fallICD-10-CM Code for Unspecified fall, initial encounter W19.
What is diagnosis code Z71 3?
Dietary counseling and surveillanceICD-10 code Z71. 3 for Dietary counseling and surveillance is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
When should you use the code v71 09?
09 for Observation of other suspected mental condition is a medical classification as listed by WHO under the range -PERSONS WITHOUT REPORTED DIAGNOSIS ENCOUNTERED DURING EXAMINATION AND INVESTIGATION.
What does code Z12 31 mean?
For example, Z12. 31 (Encounter for screening mammogram for malignant neoplasm of breast) is the correct code to use when you are ordering a routine mammogram for a patient. However, coders are coming across many routine mammogram orders that use Z12.
What is code Z12 39?
ICD-10 code Z12. 39 for Encounter for other screening for malignant neoplasm of breast is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
What is ICD-10 code N63?
2022 ICD-10-CM Diagnosis Code N63: Unspecified lump in breast.
How do you code a fall?
With ICD-10, you have R29. 6 (Repeated falls). According to the ICD-10 guidelines you would use R29. 6 when a patient has recently fallen and the reason for the fall is being investigated.
What is the diagnosis code for psychotherapy?
Code 90785 may be reported with codes for diagnostic evaluation (90791), psychotherapy (90832, 90834, 90837) and group psychotherapy (90853).
What is the CPT code for counseling?
90832 – Psychotherapy 30 minutes. 90834 – Psychotherapy 45 minutes. 90837 – Psychotherapy 60 minutes.
What is the ICD-10 code for family counseling?
Procreative counseling and advice using natural family planning. Z31. 61 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
What is a category code?
Category codes are user defined codes to which you can assign a title and a value. The title appears on the appropriate screen next to the field in which you type the code.
What is DRG #640-641?
DRG Group #640-641 - Misc disorders of nutrition, metabolism, fluids or electrolytes with MCC.
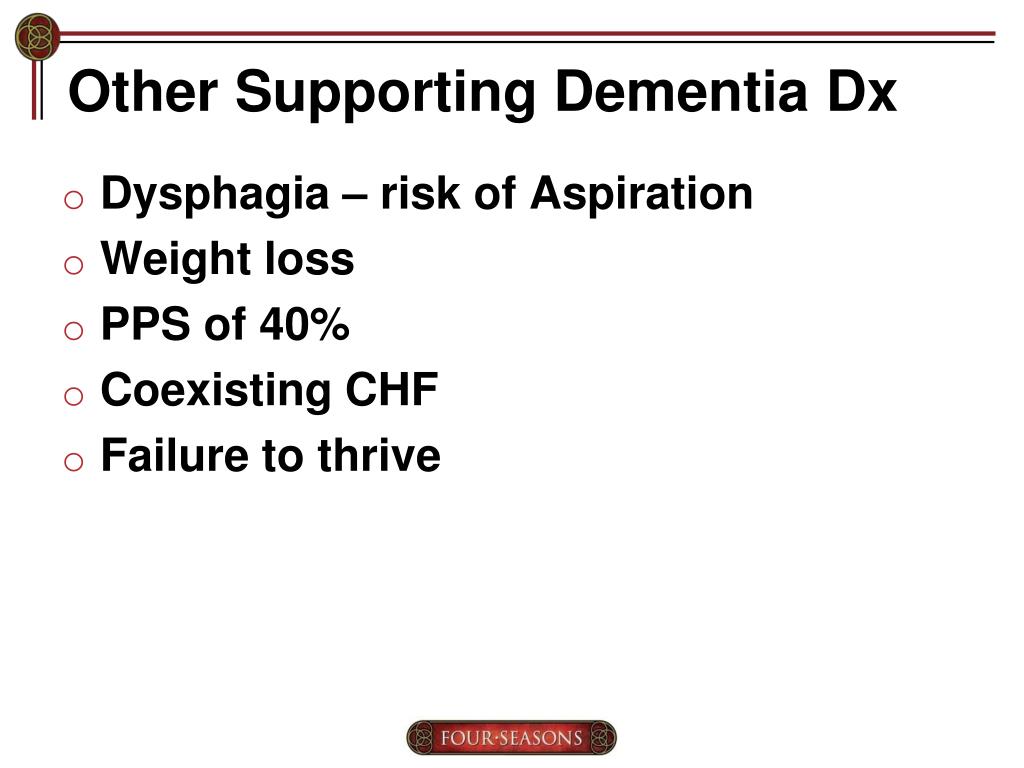
What is the ICD code for failure to thrive?
R62.51 is a billable ICD code used to specify a diagnosis of failure to thrive (child). A 'billable code' is detailed enough to be used to specify a medical diagnosis.
What is billable code?
Billable codes are sufficient justification for admission to an acute care hospital when used a principal diagnosis.
What does "type 1 excludes" mean?
Type-1 Excludes mean the conditions excluded are mutually exclusive and should never be coded together. Excludes 1 means "do not code here."
What is inclusion term?
Inclusion Terms are a list of concepts for which a specific code is used. The list of Inclusion Terms is useful for determining the correct code in some cases, but the list is not necessarily exhaustive.
What is the ICd 10 code for adult failure to thrive?
R62.7 is a valid billable ICD-10 diagnosis code for Adult failure to thrive . It is found in the 2021 version of the ICD-10 Clinical Modification (CM) and can be used in all HIPAA-covered transactions from Oct 01, 2020 - Sep 30, 2021 .
What does "Excludes 2" mean?
A type 2 Excludes note represents 'Not included here'. An Excludes2 note indicates that the condition excluded is not part of the condition it is excluded from but a patient may have both conditions at the same time. When an Excludes2 note appears under a code it is acceptable to use both the code and the excluded code together.
What does NEC not elsewhere mean?
NEC Not elsewhere classifiable#N#This abbreviation in the Tabular List represents “other specified”. When a specific code is not available for a condition, the Tabular List includes an NEC entry under a code to identify the code as the “other specified” code.
What is a type 1 exclude note?
A type 1 Excludes note is a pure excludes. It means 'NOT CODED HERE!' An Excludes1 note indicates that the code excluded should never be used at the same time as the code above the Excludes1 note. An Excludes1 is used when two conditions cannot occur together, such as a congenital form versus an acquired form of the same condition.
What is a list of terms?
List of terms is included under some codes. These terms are the conditions for which that code is to be used. The terms may be synonyms of the code title, or, in the case of “other specified” codes, the terms are a list of the various conditions assigned to that code.
When an excludes2 note appears under a code, is it acceptable to use both the code and the excluded code?
When an Excludes2 note appears under a code it is acceptable to use both the code and the excluded code together. A “code also” note instructs that two codes may be required to fully describe a condition, but this note does not provide sequencing direction. The sequencing depends on the circumstances of the encounter.
Do you include decimal points in ICD-10?
DO NOT include the decimal point when electronically filing claims as it may be rejected. Some clearinghouses may remove it for you but to avoid having a rejected claim due to an invalid ICD-10 code, do not include the decimal point when submitting claims electronically. See also: Failure, failed.
What is the secondary code for Chapter 20?
Use secondary code (s) from Chapter 20, External causes of morbidity, to indicate cause of injury. Codes within the T section that include the external cause do not require an additional external cause code. code to identify any retained foreign body, if applicable ( Z18.-)
Can you use S22.08 for reimbursement?
S22.08 should not be used for reimbursement purposes as there are multiple codes below it that contain a greater level of detail.
What is CMS in healthcare?
The Centers for Medicare & Medicaid Services (CMS), the federal agency responsible for administration of the Medicare, Medicaid and the State Children's Health Insurance Programs, contracts with certain organizations to assist in the administration of the Medicare program. Medicare contractors are required to develop and disseminate Local Coverage Determinations (LCDs). CMS believes that the Internet is an effective method to share LCDs that Medicare contractors develop. While every effort has been made to provide accurate and complete information, CMS does not guarantee that there are no errors in the information displayed on this web site. THE UNITED STATES GOVERNMENT AND ITS EMPLOYEES ARE NOT LIABLE FOR ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION, PRODUCT, OR PROCESSES DISCLOSED HEREIN. Neither the United States Government nor its employees represent that use of such information, product, or processes will not infringe on privately owned rights. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information, product, or process.
What is a local coverage determination?
A Local Coverage Determination (LCD) is a decision made by a Medicare Administrative Contractor (MAC) on whether a particular service or item is reasonable and necessary, and therefore covered by Medicare within the specific jurisdiction that the MAC oversees.
Does CMS have a CDT license?
Organizations who contract with CMS acknowledge that they may have a commercial CDT license with the ADA, and that use of CDT codes as permitted herein for the administration of CMS programs does not extend to any other programs or services the organization may administer and royalties dues for the use of the CDT codes are governed by their commercial license.
What does "you" mean when acting on behalf of an organization?
If you are acting on behalf of an organization, you represent that you are authorized to act on behalf of such organization and that your acceptance of the terms of this agreement creates a legally enforceable obligation of the organization. As used herein, “you” and “your” refer to you and any organization on behalf of which you are acting.
Is CPT a year 2000?
CPT is provided “as is” without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. AMA warrants that due to the nature of CPT, it does not manipulate or process dates, therefore there is no Year 2000 issue with CPT. AMA disclaims responsibility for any errors in CPT that may arise as a result of CPT being used in conjunction with any software and/or hardware system that is not Year 2000 compliant. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon no upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
Can you use CPT in Medicare?
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials of CMS internally within your organization within the United States for the sole use by yourself, employees and agents. Use is limited to use in Medicare, Medicaid or other programs administered by the Centers for Medicare and Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
What is Verdery RB?
Verdery RB. Clinical evaluation of failure to thrive in older people. Clinics in Geriatric Medicine. 1997;13 (4):769-778.
What is DRG #640-641?
DRG Group #640-641 - Misc disorders of nutrition, metabolism, fluids or electrolytes with MCC.
What is the ICD code for failure to thrive?
R62.51 is a billable ICD code used to specify a diagnosis of failure to thrive (child). A 'billable code' is detailed enough to be used to specify a medical diagnosis.
What is billable code?
Billable codes are sufficient justification for admission to an acute care hospital when used a principal diagnosis.
What does "type 1 excludes" mean?
Type-1 Excludes mean the conditions excluded are mutually exclusive and should never be coded together. Excludes 1 means "do not code here."
What is inclusion term?
Inclusion Terms are a list of concepts for which a specific code is used. The list of Inclusion Terms is useful for determining the correct code in some cases, but the list is not necessarily exhaustive.
Popular Posts:
- 1. icd-10 code for mets to the left lung
- 2. icd 10 code for enlarged inferior vena cava
- 3. icd 10 pcs code for pyelonephritis
- 4. icd 10 code for itchy skin rash
- 5. icd-10 code for c&s of vagina
- 6. icd 10 code for atherosclerosis of native arteries of extremities with intermittent claudication
- 7. icd 10 code for recurrent perianal abscess
- 8. icd 10 cm code for: anxiety over parents diagnosis
- 9. icd 9 code for poor prep for colonoscopy
- 10. icd 9 code for anticoagulated state