What is the ICD 10 code for history of parasitic disease?
2018/2019 ICD-10-CM Diagnosis Code Z86.19. Personal history of other infectious and parasitic diseases. Z86.19 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
What is the ICD 10 code for history of infectious disease?
Z86.19 is a billable ICD code used to specify a diagnosis of personal history of other infectious and parasitic diseases. A 'billable code' is detailed enough to be used to specify a medical diagnosis.
What is the ICD 10 code for sexual transmitted infection?
Z11.3 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. Short description: Encntr screen for infections w sexl mode of transmiss; The 2021 edition of ICD-10-CM Z11.3 became effective on October 1, 2020.
What is the ICD 10 code for genital history?
Z87.438 is a billable code used to specify a medical diagnosis of personal history of other diseases of male genital organs. The code is valid for the year 2019 for the submission of HIPAA-covered transactions.
What is the ICD 10 code for Z86 19?
Z86. 19 Personal history of other infectious and parasitic diseases - ICD-10-CM Diagnosis Codes.
What is the ICD 10 code for history of chlamydia?
ICD-10-CM Diagnosis Code A56 A56. 00 Chlamydial infection of lower genitourinary t...
What does diagnosis Z20 2 mean?
ICD-10 code: Z20. 2 Contact with and exposure to infections with a predominantly sexual mode of transmission.
What does diagnosis code Z11 3 mean?
For claims for screening for syphilis in men at increased risk use the following ICD-10-CM diagnosis codes: • Z11.3 - Encounter for screening for infections with a predominantly sexual mode of transmission; and. • any of Z72.
What is the diagnosis for ICD-10 code r50 9?
9: Fever, unspecified.
What is the history of chlamydia?
Chlamydia first became recognized as a specific STI in the 1970s, but it took until 1988 for it to become notifiable. Newly diagnosed cases were reported only routinely in STI statistics from 1990, when there were 34,000 new diagnoses. The number began to rise steeply after 1995, reaching 100,000 in 2003.
What does Z01 419 include?
411, Encounter for gynecological examination (general) (routine) with abnormal findings, or Z01. 419, Encounter for gynecological examination (general) (routine) without abnormal findings, may be used as the ICD-10-CM diagnosis code for the annual exam performed by an obstetrician–gynecologist.
What is the CPT code for STD screening?
This policy describes reimbursement for Infectious agent detection by nucleic acid (DNA or RNA) assays for the detection of Sexually Transmitted Infections (STI), represented by CPT codes 87491, 87591, 87661, or 87801, and submitted for reimbursement on professional and facility claim forms.
What ICD 10 code covers RPR?
Other specified abnormal immunological findings in serum The 2022 edition of ICD-10-CM R76. 8 became effective on October 1, 2021.
What does chlamydial infection unspecified mean?
The chlamydia cause respiratory infection manifested with fever, malaise, cough, dyspnea, sore throat, photophobia and headaches. Chlamydia is a common sexually transmitted disease caused by bacteria. You get it by having sex or sexual contact with someone who is infected. Both men and women can get it.
What is the ICD-10 code for STD screening?
ICD-10 code Z11. 3 for Encounter for screening for infections with a predominantly sexual mode of transmission is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
What does GC chlamydia mean?
Chlamydia trachomatis (CT) and Neisseria gonorrhoeae (GC) are the two most common bacterial causes of sexually transmitted diseases worldwide. In the United States CT and GC account for about 4 million and 2 million annual cases of genital infection respectively.
What is the ICD-10 code for chlamydia in pregnancy?
What are the appropriate ICD-10 codes for History of chlamydia in pregnancy? O98. 81x Other maternal infectious & parasitic disease complicating pregnancy, xxx trimester + Z86. 19 Personal history of other infectious and parasitic diseases?
When will the ICD-10 Z11.3 be released?
The 2022 edition of ICD-10-CM Z11.3 became effective on October 1, 2021.
What is a Z00-Z99?
Categories Z00-Z99 are provided for occasions when circumstances other than a disease, injury or external cause classifiable to categories A00 -Y89 are recorded as 'diagnoses' or 'problems'. This can arise in two main ways:
What is the ICd 10 code for a mapped ICd 9?
The General Equivalency Mapping (GEM) crosswalk indicates an approximate mapping between the ICD-10 code Z87.438 its ICD-9 equivalent. The approximate mapping means there is not an exact match between the ICD-10 code and the ICD-9 code and the mapped code is not a precise representation of the original code.
What is the Z87.438 code?
Z87.438 is a billable diagnosis code used to specify a medical diagnosis of personal history of other diseases of male genital organs. The code Z87.438 is valid during the fiscal year 2021 from October 01, 2020 through September 30, 2021 for the submission of HIPAA-covered transactions.
What is an unacceptable diagnosis?
Unacceptable principal diagnosis - There are selected codes that describe a circumstance which influences an individual's health status but not a current illness or injury, or codes that are not specific manifestations but may be due to an underlying cause. These codes are considered unacceptable as a principal diagnosis.
What is Medicare code editor?
The Medicare Code Editor (MCE) detects and reports errors in the coding of claims data. The following ICD-10 Code Edits are applicable to this code:
Is Z87.438 a POA?
Z87.438 is exempt from POA reporting - The Present on Admission (POA) indicator is used for diagnosis codes included in claims involving inpatient admissions to general acute care hospitals. POA indicators must be reported to CMS on each claim to facilitate the grouping of diagnoses codes into the proper Diagnostic Related Groups (DRG). CMS publishes a listing of specific diagnosis codes that are exempt from the POA reporting requirement. Review other POA exempt codes here.
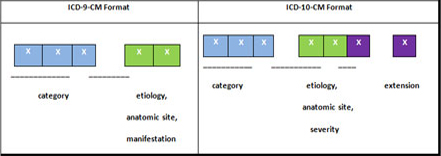
What is the convention of ICd 10?
The conventions for the ICD-10-CM are the general rules for use of the classification independent of the guidelines. These conventions are incorporated within the Alphabetic Index and Tabular List of the ICD-10-CM as instructional notes.
Which code should be sequenced first?
code from subcategory O9A.2, Injury, poisoning and certain other consequences of external causes complicating pregnancy, childbirth, and the puerperium, should be sequenced first, followed by the appropriate injury, poisoning, toxic effect, adverse effect or underdosing code, and then the additional code(s) that specifies the condition caused by the poisoning, toxic effect, adverse effect or underdosing.
What is code assignment?
Code assignment is based on the provider’s documentation of the relationship between the condition and the care or procedure, unless otherwise instructed by the classification. The guideline extends to any complications of care, regardless of the chapter the code is located in. It is important to note that not all conditions that occur during or following medical care or surgery are classified as complications. There must be a cause-and-effect relationship between the care provided and the condition, and an indication in the documentation that it is a complication. Query the provider for clarification, if the complication is not clearly documented.
What does "with" mean in coding?
The word “with” or “in” should be interpreted to mean “associated with” or “due to” when it appears in a code title, the Alphabetic Index (either under a main term or subterm), or an instructional note in the Tabular List. The classification presumes a causal relationship between the two conditions linked by these terms in the Alphabetic Index or Tabular List. These conditions should be coded as related even in the absence of provider documentation explicitly linking them, unless the documentation clearly states the conditions are unrelated or when another guideline exists that specifically requires a documented linkage between two conditions (e.g., sepsis guideline for “acute organ dysfunction that is not clearly associated with the sepsis”).For conditions not specifically linked by these relational terms in the classification or when a guideline requires that a linkage between two conditions be explicitly documented, provider documentation must link the conditions in order to code them as related.
When to use counseling Z codes?
Counseling Z codes are used when a patient or family member receives assistance in the aftermath of an illness or injury, or when support is required in coping with family or social problems.
When assigning a chapter 15 code for sepsis complicating abortion, pregnancy, childbirth, and the?
When assigning a chapter 15 code for sepsis complicating abortion, pregnancy, childbirth, and the puerperium, a code for the specific type of infection should be assigned as an additional diagnosis. If severe sepsis is present, a code from subcategory R65.2, Severe sepsis, and code(s) for associated organ dysfunction(s) should also be assigned as additional diagnoses.
Do not code diagnoses documented as “probable”, “suspected,” “questionable,” “?
Do not code diagnoses documented as “probable”, “suspected,” “questionable,” “rule out,” “compatible with,” “consistent with,” or “working diagnosis” or other similar terms indicating uncertainty. Rather, code the condition(s) to the highest degree of certainty for that encounter/visit, such as symptoms, signs, abnormal test results, or other reason for the visit.
What is the ICD code for parasitic disease?
Z86.19 is a billable ICD code used to specify a diagnosis of personal history of other infectious and parasitic diseases. A 'billable code' is detailed enough to be used to specify a medical diagnosis.
What is billable code?
Billable codes are sufficient justification for admission to an acute care hospital when used a principal diagnosis. The Center for Medicare & Medicaid Services (CMS) requires medical coders to indicate whether or not a condition was present at the time of admission, in order to properly assign MS-DRG codes.
Is a diagnosis present at time of inpatient admission?
Diagnosis was present at time of inpatient admission. Yes. N. Diagnosis was not present at time of inpatient admission. No. U. Documentation insufficient to determine if the condition was present at the time of inpatient admission. No.

Popular Posts:
- 1. icd 10 code for infantile cerebral palsy
- 2. icd 10 code for albuterol
- 3. icd 10 code for low body weight
- 4. icd 9 code for ectropion
- 5. icd 10 code for cervical spine pain with radiculopathy
- 6. icd 10 code for left hand finger pain
- 7. icd 10 code for femoral and actetabuloplasty.
- 8. icd 10 code for tos
- 9. icd 10 code for reversal of colostomy
- 10. icd 10 code for unspecified contractures