What is the purpose of ICD 10 cm?
2016 (effective 10/1/2015): New code (first year of non-draft ICD-10-CM) 2017 (effective 10/1/2016): No change 2018 (effective 10/1/2017): No change 2019 (effective 10/1/2018): No change 2020 (effective 10/1/2019): No change 2021 (effective 10/1/2020): No change 2022 (effective 10/1/2021): No ...
What ICD 10 cm code(s) are reported?
Nov 13, 2020 · ICD 10 Code for HIV (Human Immunodeficiency Virus) is listed below: HIV – B20. Symptomatic HIV – B20. HIV Positive – Z21. Asymptomatic HIV – Z21. HIV Negative – Z71.7. Code only the confirmed cases. ICD 10 code for HIV should be coded only when it’s confirmed from the provider. For example:
What is the ICD 10 diagnosis code for?
Apr 20, 2016 · November 20, 2016. April 20, 2016 by Laureen Jandroep. Q: HIV ICD 10 CM Codes – “On the HIV codes, when do you use the Z code versus the B code? Would you code the patient as being active if they have history of HIV?”. A: When we start looking at the AIDS and HIV codes, we originally received this question that came asking, “When do we ...
What is the CPT code for HIV testing?
12 rows · HIV Screening CPT and ICD -10 Codes TEST PRODUCT PTEST RODUCT Code Rapid Test Modifier ...
How do you code HIV?
Assign code Z21 — Asymptomatic human immunodeficiency virus [HIV] infection status when the patient without any documentation of symptoms is listed as being 'HIV positive', 'known HIV', 'HIV test positive' or similar terminology.Jan 19, 2020
What is ICD-10 code Z21?
Code Z21 is used for patients who are asymptomatic, meaning they are HIV positive but have never had an HIV-related condition.May 14, 2019
What is the ICD-10 code for HIV screening?
Z11. 4 Encounter for screening for human immunodeficiency virus (HIV).Oct 13, 2020
How many stages of HIV are there?
What they explained is that there are really three stages of HIV. There’s the Acute Infection point where the person first gets infected and their body, it’s a virus so it’s replicating constantly. That’s that acute infection timeframe. Usually, they might have some flu-like symptoms.
How many CD4 cells are needed for HIV?
They have not yet had a symptom related to their HIV. When we talk about symptoms related to their HIV, CDC actually defines AIDS, their CD4 cells fall below 200 cells and that’s when it’s progressed to AIDS.
What is clinical latency?
Then, they fall into a period of what we call Clinical Latency. That means that the virus is just there, doing its thing replicating, not making them sick but continuing to spread throughout their bloodstream. It’s reproducing at a lower level than that initial thing, but it’s still considered active infection.
Is a bronchial infection a fungal infection?
Candidiasis of bronchi, trachea, esophagus, lungs, that’s a fungal infection down in there. A patient with AIDS or with HIV has a compromised immune system, they’re not going to be able to fight off these infections as well as a normal healthy patient would.
Is HIV asymptomatic or opportunistic?
Yeah, they thought they had the flu, but it’s not necessarily asymptomatic, it’s not an opportunistic infection. When we start looking through here, the guidelines actually say, “OK, if they’ve not had a symptom of HIV, they’re asymptomatic.”. Usually, the provider is going to call this HIV positive, known HIV, ...
Is HIV a clinically significant condition?
Every insurance company and actually the coding rules, the way that they have always been explained to me, even if you look in the ICD-10 guidelines, HIV is the only condition that is considered to always be clinically significant.
Can you have a history of HIV?
When we first start looking at HIV, the important thing to understand here is that a patient at this point in time cannot have a history of HIV, it’s not possible. We do not yet have a cure for HIV. Once the patient has HIV, they have HIV for life.
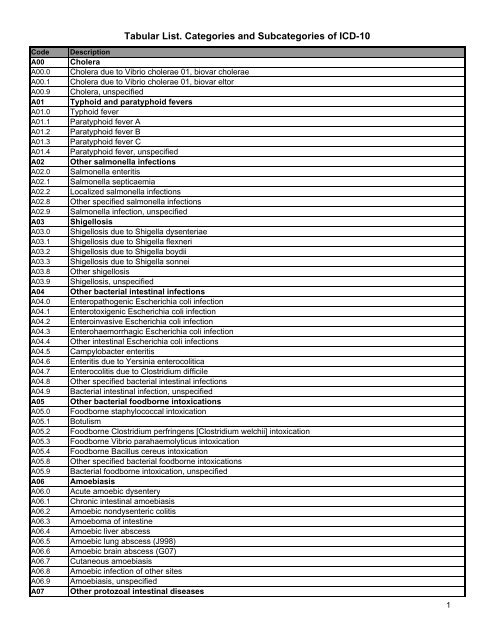
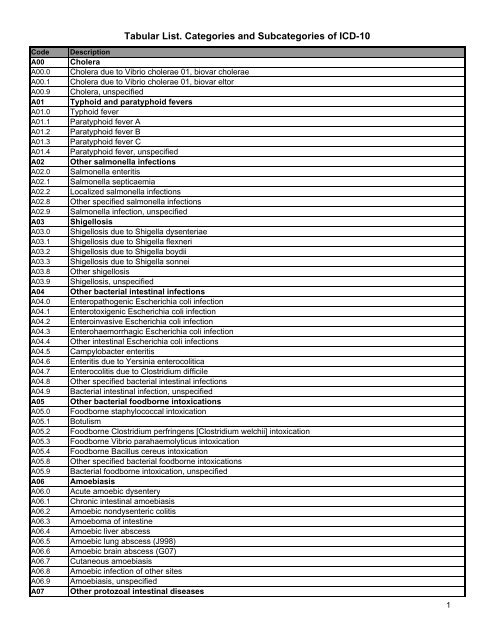
What is the convention of ICd 10?
The conventions for the ICD-10-CM are the general rules for use of the classification independent of the guidelines. These conventions are incorporated within the Alphabetic Index and Tabular List of the ICD-10-CM as instructional notes.
When assigning a chapter 15 code for sepsis complicating abortion, pregnancy, childbirth, and the
When assigning a chapter 15 code for sepsis complicating abortion, pregnancy, childbirth, and the puerperium, a code for the specific type of infection should be assigned as an additional diagnosis. If severe sepsis is present, a code from subcategory R65.2, Severe sepsis, and code(s) for associated organ dysfunction(s) should also be assigned as additional diagnoses.
What is code assignment?
Code assignment is based on the provider’s documentation of the relationship between the condition and the care or procedure, unless otherwise instructed by the classification. The guideline extends to any complications of care, regardless of the chapter the code is located in. It is important to note that not all conditions that occur during or following medical care or surgery are classified as complications. There must be a cause-and-effect relationship between the care provided and the condition, and an indication in the documentation that it is a complication. Query the provider for clarification, if the complication is not clearly documented.
What does "with" mean in coding?
The word “with” or “in” should be interpreted to mean “associated with” or “due to” when it appears in a code title, the Alphabetic Index (either under a main term or subterm), or an instructional note in the Tabular List. The classification presumes a causal relationship between the two conditions linked by these terms in the Alphabetic Index or Tabular List. These conditions should be coded as related even in the absence of provider documentation explicitly linking them, unless the documentation clearly states the conditions are unrelated or when another guideline exists that specifically requires a documented linkage between two conditions (e.g., sepsis guideline for “acute organ dysfunction that is not clearly associated with the sepsis”).For conditions not specifically linked by these relational terms in the classification or when a guideline requires that a linkage between two conditions be explicitly documented, provider documentation must link the conditions in order to code them as related.
When to use counseling Z codes?
Counseling Z codes are used when a patient or family member receives assistance in the aftermath of an illness or injury, or when support is required in coping with family or social problems.
Which code should be sequenced first?
code from subcategory O9A.2, Injury, poisoning and certain other consequences of external causes complicating pregnancy, childbirth, and the puerperium, should be sequenced first, followed by the appropriate injury, poisoning, toxic effect, adverse effect or underdosing code, and then the additional code(s) that specifies the condition caused by the poisoning, toxic effect, adverse effect or underdosing.
Do not code diagnoses documented as “probable”, “suspected,” “questionable,” “
Do not code diagnoses documented as “probable”, “suspected,” “questionable,” “rule out,” “compatible with,” “consistent with,” or “working diagnosis” or other similar terms indicating uncertainty. Rather, code the condition(s) to the highest degree of certainty for that encounter/visit, such as symptoms, signs, abnormal test results, or other reason for the visit.
Popular Posts:
- 1. icd 9 code for prolonged rupture of membranes affecting neworn
- 2. icd 10 code for flame burn
- 3. icd 10 code for severe dysplasia of cervix
- 4. icd 10 code for eye drops dry eyes
- 5. icd 10 code for travel consult
- 6. icd 10 code for failed back syndrome
- 7. true or false? the icd-10 code for obesity is e66.9.
- 8. icd 10 cm code for falling off the gurney
- 9. icd 10 code for left rotator cuff tendonitis
- 10. icd 10 code for personal history of peptifc ulcer dz