What is the diagnosis code for lumbar spine pain?
M54.5 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2021 edition of ICD-10-CM M54.5 became effective on October 1, 2020. This is the American ICD-10-CM version of M54.5 - other international versions of ICD-10 M54.5 may differ.
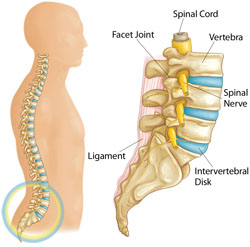
What causes pain in the lumbar area?
Possible Causes and Treatment Options
- Muscle strain. One of the most common causes of radiating pain is from muscle strain. ...
- Pinched nerve. Pinched nerves occur when a nerve is compressed unnaturally by surrounding tissue or bone. ...
- Arthritis. Arthritis is a common condition many individuals begin to experience as they age. ...
- Herniated disc. ...
- Sacroiliac joint dysfunction. ...
What is the ICD 10 code for severe pain?
What is the ICD 10 code for severe pain? Pain, unspecified . R52 is a billable /specific ICD -10- CM code that can be used to indicate a diagnosis for reimbursement purposes.
What is the ICD 10 code for DJD lumbar?
- 2016 (effective 10/1/2015): New code (first year of non-draft ICD-10-CM)
- 2017 (effective 10/1/2016): No change
- 2018 (effective 10/1/2017): Deleted code
- 2018 (effective 10/1/2017): New code
- 2019 (effective 10/1/2018): No change
- 2020 (effective 10/1/2019): No change
- 2021 (effective 10/1/2020): No change
- 2022 (effective 10/1/2021): No change
What is the ICD code for low back pain?
5 - Low back pain is a sample topic from the ICD-10-CM. To view other topics, please log in or purchase a subscription. ICD-10-CM 2022 Coding Guide™ from Unbound Medicine.
What is the ICD-10 code for middle back pain?
ICD-10 code: M54. 6 Pain in thoracic spine | gesund.bund.de.
What is the ICD-10 code for right sided back pain?
Lumbago with sciatica, right side 41 became effective on October 1, 2021. This is the American ICD-10-CM version of M54.
What is the diagnosis code for chronic back pain?
M54. 9 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
What means Dorsalgia?
For starters, dorsalgia is severe back pain, which could be coming from different parts of the spine. Depending on the specific section of the spine where the pain is coming from, there are six types of dorsalgia.
What character in ICD-10-CM coding represents the lumbar region of the spine?
M51. 86 - Other intervertebral disc disorders, lumbar region | ICD-10-CM.
What is the ICD-10 code for bilateral low back pain with sciatica?
4: Lumbago with sciatica.
What is the ICD-10-CM code for sciatica?
3 – Sciatica. ICD-Code M54. 3 is a non-billable ICD-10 code used for healthcare diagnosis reimbursement of Sciatica.
What is the ICD-10 code for lumbar spondylosis?
ICD-10-CM Code for Spondylosis without myelopathy or radiculopathy, lumbar region M47. 816.
What is the ICD-10 code for pain?
ICD-10 code R52 for Pain, unspecified is a medical classification as listed by WHO under the range - Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified .
What is the ICD-10 code for acute on chronic pain?
ICD-10 code G89. 4 for Chronic pain syndrome is a medical classification as listed by WHO under the range - Diseases of the nervous system .
What is the ICd 10 code for pain?
The ICD-10-CM Official Guidelines for Coding and Reporting provide extensive notes and instruction for coding pain (category G89). Review these guidelines in full. The following summary identifies key points.#N#When seeking a pain diagnosis, identify as precisely as possible the pain’s location and/or source. If pain is the primary symptom and you know the location, the Alphabetic Index generally will provide all the information you need.#N#Only report pain diagnosis codes from the G89 category as the primary diagnosis when: 1 The acute or chronic pain and neoplasm pain provide more detail when used with codes from other categories; or 2 The reason for the service is for pain control or pain management.
How long does chronic pain last?
Chronic pain may last for months or years, and may persist even after the underlying injury has healed or the underlying condition has been treated. There is no specific timeframe identifying when you can define the pain as chronic. Determine the code assignment based on provider documentation.
Where is back pain located?
Acute or chronic pain located in the posterior regions of the thorax; lumbosacral region; or the adjacent regions. If you've ever groaned, "oh, my aching back!", you are not alone. Back pain is one of the most common medical problems, affecting 8 out of 10 people at some point during their lives.
How long does back pain last?
Acute back pain comes on suddenly and usually lasts from a few days to a few weeks. Back pain is called chronic if it lasts for more than three months. most back pain goes away on its own, though it may take awhile.
How long does it take for back pain to go away?
If your back pain is severe or doesn't improve after three days, you should call your health care provider. You should also get medical attention if you have back pain following an injury.treatment for back pain depends on what kind of pain you have, and what is causing it.

Popular Posts:
- 1. icd 10 code for pons
- 2. icd 9 code for umbilical hernia repair
- 3. icd 10 code for skipped heart beats
- 4. icd 10 code for left hallux valgus
- 5. icd code for pulmonary embolism
- 6. icd 10 code for nasal congestion in pregnancy
- 7. icd 10 code for left upper lobe ground-glass infiltrate
- 8. icd 10 code for dermoid cyst unspecified
- 9. icd 10 code for cadasil
- 10. icd 10 code for muscle dystonia