For Federal Fiscal Year (FFY) 2019 the International Classification of Diseases 10th Edition, Clinical Modification (ICD-10-CM) expanded code subcategories T81.4, Infection following a procedure, and O86.0, Infection of obstetrical surgical wound, to identify the depth of the post-procedural infection and a separate code to identify post-procedural sepsis.
What is the diagnosis code for post op?
The diagnostic code you use needs to be identical to that used by the surgeon. The date of service should correspond to the date of the surgery. Use the same surgical CPT procedure code used by the surgeon, but add the -55 modifier to signify that you are rendering the postoperative care.
What is the ICD 10 diagnosis code for?
The ICD-10-CM is a catalog of diagnosis codes used by medical professionals for medical coding and reporting in health care settings. The Centers for Medicare and Medicaid Services (CMS) maintain the catalog in the U.S. releasing yearly updates.
What is the diagnosis code for wound infection?
wound infection T81.49 Infection, infected, infective (opportunistic) B99.9 postoperative wound T81.49 surgical site specified NEC T81.49 operation wound T81.49 Sepsis (generalized) (unspecified organism) A41.9 localized - code to specific localized infection in operation wound T81.49
What is the ICD 10 code for infected surgical wound?
- Application site infection
- Infected seroma after surgical procedure
- Infected seroma due to and following procedure
- Infection of tendon repair
- Infectious disorder of tendon
- Meningitis following procedure
- Organ surgical site infection
- Postoperative bacterial meningitis
- Postoperative infection
- Postoperative infection of thyroidectomy wound
What is the ICD-10 code for postoperative wound infection?
4-, a post-procedural wound infection and post-procedural sepsis were assigned to the same ICD-10-CM code T81. 4-, Infection following a procedure with a code for the infection (sepsis, cellulitis, etc.)
What is the ICD-10 code for surgical wound?
ICD-10 Code for Disruption of external operation (surgical) wound, not elsewhere classified, initial encounter- T81. 31XA- Codify by AAPC.
What is the ICD-10 code for C section wound infection?
ICD-10-CM Code for Infection of obstetric surgical wound O86. 0.
How do you code Post procedural sepsis?
Sepsis due to a postprocedural infection: For such cases, the postprocedural infection code should be coded first, such as: T80....2, severe sepsis.If the causal organism is not documented, code A41. ... An additional code should be assigned for the organ dysfunction severe sepsis is causing, such as, N17.More items...•
How do you code a surgical site infection?
Postoperative wound infection is classified to ICD-9-CM code 998.59, Other postoperative infection. Code 998.59 also includes postoperative intra-abdominal abscess, postoperative stitch abscess, postoperative subphrenic abscess, postoperative wound abscess, and postoperative septicemia.
How do you code a wound in ICD-10?
The types of open wounds classified in ICD-10-CM are laceration without foreign body, laceration with foreign body, puncture wound without foreign body, puncture wound with foreign body, open bite, and unspecified open wound. For instance, S81. 812A Laceration without foreign body, right lower leg, initial encounter.
What is disruption of cesarean delivery wound?
Wound disruption was defined as subcutaneous skin dehiscence (from any cause including seroma or hematoma) or fascial dehiscence. Women with wound infections were excluded. Patient demographics, medical co-morbidities, and intrapartum characteristics were evaluated as potential risk factors.
Is cellulitis a surgical site infection?
Most cellulitis occurs in the legs, but it can occur almost anywhere on the body. 2 For the surgery patient, the site of an incision is by far the most common site of infection.
What is the ICD 10 code for infected seroma?
998.51 - Infected postoperative seroma. ICD-10-CM.
What is surgical site infection?
A surgical site infection (SSI) is an infection that occurs after surgery in the part of the body where the surgery took place. Surgical site infections can sometimes be superficial infections involving the skin only.
What is the ICD-10 code for sepsis?
Septicemia – There is NO code for septicemia in ICD-10. Instead, you're directed to a combination 'A' code for sepsis to indicate the underlying infection, such A41. 9 (Sepsis, unspecified organism) for septicemia with no further detail.
When do you code sepsis?
Coding sepsis requires a minimum of two codes: a code for the systemic infection (e.g., 038. xx) and the code 995.91, SIRS due to infectious process without organ dysfunction. If no causal organism is documented within the medical record, query the physician or assign code 038.9, Unspecified septicemia.
What is the code for postoperative fever?
If the physician states only “postoperative fever” and doesn’t identify the source and it is evaluated, monitored, or treated, then assign code 780.62.
How long does postoperative infection last?
However, it most commonly occurs between five and 10 days after surgery. From an ICD-9-CM coding perspective, there is no time limitation regarding the assignment of a complication code.
What is a T86 code?
A preexisting condition or a condition that develops after the transplant is coded as a transplant complication if it affects the function of the transplanted organ. Assign the T86 code first, followed by a code for the condition.
What are the four categories of wound contamination?
The four categories of wound contamination are clean wounds with no gross contamination, lightly contaminated wounds (stomach or biliary surgeries), heavily contaminated wounds (intestinal surgeries), and infected wounds in which infection is obviously present prior to surgical incision. Postoperative Fever. It is normal for a patient ...
How long does it take for a patient to have a low temperature after surgery?
It is normal for a patient to have a low-grade temperature for one to two days after surgery due to the body’s response to a foreign invasion. The following is what is expected following surgery: • a 100˚F temperature for the first two days after surgery; • post-op antibiotics ordered the day of surgery;
Do you have to assign a code for pneumonia?
It is appropriate to assign a code to identify the organism involved, if known. However, do not assign an additional code for the type of pneumonia (eg, Pseudomonas pneumonia).
Can you code T86.1 for CKD?
Therefore, code T86.1- should not be assigned for patients who have CKD in a transplanted organ. This is an exception to the above coding guideline. It would be appropriate to assign code T86.1- for transplant failure, rejection, or another complication that affects the function of the transplanted kidney.
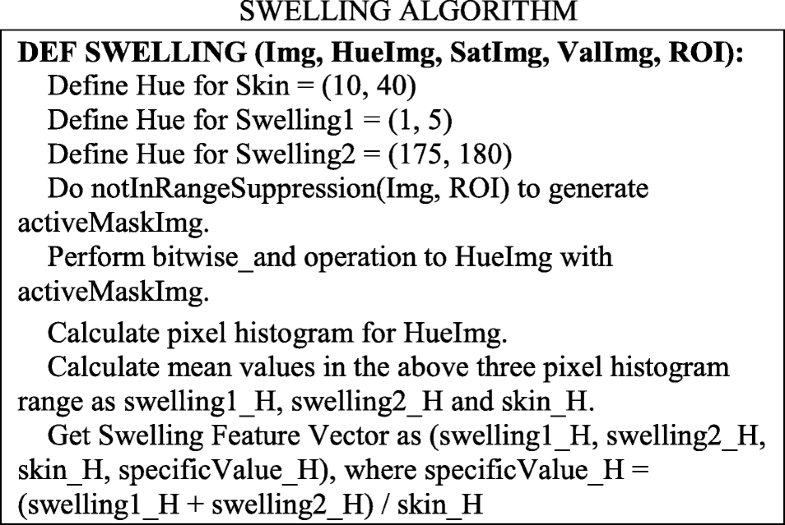
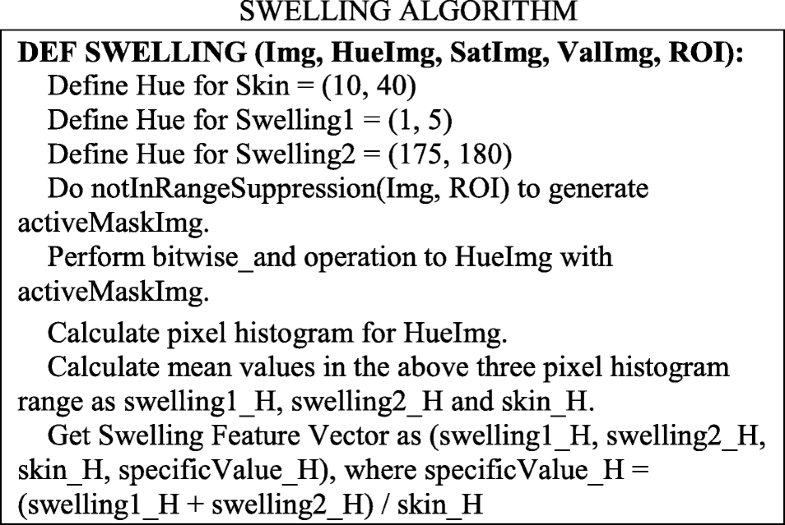
International Classification and Official Guideline Update
For Federal Fiscal Year (FFY) 2019 the International Classification of Diseases 10th Edition, Clinical Modification (ICD-10-CM) expanded code subcategories T81.4, Infection following a procedure, and O86.0, Infection of obstetrical surgical wound, to identify the depth of the post-procedural infection and a separate code to identify post-procedural sepsis.
Addressing Public Health Issues with Coding
SSIs are persistent and preventable healthcare-associated infections. There is increasing demand for evidence-based interventions for the prevention of SSI. Prior to the 2017 update, the last version of the CDC Guideline for Prevention of Surgical Site Infection was published in 1999.
Popular Posts:
- 1. icd code 10 for dehydration
- 2. icd 10 code for medicare depression screening
- 3. icd 10 code for infectious disease right foot
- 4. icd 10 code for b/l cerumen impaction
- 5. icd 10 code for bulging disc
- 6. icd 10 code for isolated systolic hypertension
- 7. icd 10 code for knee joint effusion
- 8. icd 10 code for presence of peg tube
- 9. icd 10 cm code for peg status
- 10. icd-10 dx code for venous stasis wound