What are the symptoms of primary ciliary dyskinesia?
Most babies with primary ciliary dyskinesia experience breathing problems at birth, which suggests that cilia play an important role in clearing fetal fluid from the lungs. Beginning in early childhood, affected individuals develop frequent respiratory tract infections.
When was primary ciliary dyskinesia first described?
The classic symptom combination associated with PCD was first described by A. K. Zivert in 1904, while Kartagener published his first report on the subject in 1933. ^ Coren, M. E; Meeks, M; Morrison, I; Buchdahl, R. M; Bush, A (2002). "Primary ciliary dyskinesia: Age at diagnosis and symptom history".
What is the best treatment for ciliary dyskinesia?
Treatment. Severe fatal respiratory failure can develop; long-term treatment with macrolides such as clarithromycin, erythromycin and azithromycin has been empirically applied for the treatment of primary ciliary dyskinesia in Japan, though controversial due to the effects of the medications.
What is the ICD 10 code for Kartagener's syndrome?
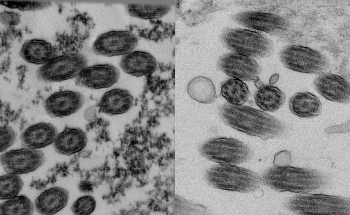
| ICD-10 from 2011 - 2016 ICD Code J98.0 is a non-billable code. To code a diagnosis of this type, you must use one of the two child codes of J98.0 that describes the diagnosis 'diseases of bronchus, not elsewhere classified' in more detail. Normal cilia (A) and cilia representative of Kartagener's syndrome (B).

What is ciliary dyskinesia?
Primary ciliary dyskinesia (PCD) is a rare inherited disorder caused by defects in the structure and/or function of cilia. Cilia are tiny hair-like structures, which are required to move fluids and particles in various parts of the body, including the airways.
What is the diagnosis for ICD-10 code r50 9?
9: Fever, unspecified.
What is the prognosis for primary ciliary dyskinesia?
An early diagnosis and proper treatment also can prevent or delay lung damage. Many people who have PCD have normal lifespans. However, about 25% of people who have the disease may develop respiratory failure, a life-threatening condition. A small number of people who have PCD need lung transplants.
What is the ICD-10 code for right gaze preference?
Other specified disorders of binocular movement The 2022 edition of ICD-10-CM H51. 8 became effective on October 1, 2021.
What is ICD-10 code R51?
ICD-10 code R51 for Headache is a medical classification as listed by WHO under the range - Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified .
What is DX R05?
1 (Acute cough) R05.
Is primary ciliary dyskinesia the same as cystic fibrosis?
But the roots of the two diseases are different: PCD arises from a malfunction of the cilia, the cellular “brooms” that normally sweep mucus out of the respiratory tract. CF patients, in contrast, have trouble transporting salt and water across cell membranes, causing their bodies to produce abnormally sticky mucus.
Is Kartagener syndrome the same as primary ciliary dyskinesia?
Kartagener syndrome is part of the larger group of disorders referred to as primary ciliary dyskinesias. Approximately one half of patients with primary ciliary dyskinesia have situs inversus and, thus, are classified as having Kartagener syndrome.
How is primary ciliary dyskinesia diagnosed?
Diagnosis. Primary ciliary dyskinesia is diagnosed definitively through examination of lung or sinus tissue obtained from a biopsy or through genetic testing. Specific structural defects that are present in these tissues can be detected under an electron microscope.
What is gaze preference?
Gaze preference is an acute inability to produce gaze contralateral to the side of a cerebral (supranuclear) lesion; it is accompanied by a tendency for tonic deviation of the eyes toward the side of the lesion.
What does Disconjugate gaze mean?
Dysconjugate gaze is a failure of the eyes to turn together in the same direction.
What causes gaze preference?
Vertical gaze palsies Upward and downward gaze depends on input from fiber pathways that ascend from the vestibular system through the MLF on both sides to the 3rd and 4th cranial nerve nuclei, the interstitial nucleus of Cajal, and the rostral interstitial nucleus of the MLF.
What is the name of the disease that causes defects in the cilia lining the respiratory tract?
Primary ciliary dyskinesia (PCD), also immotile ciliary syndrome or Kartagener syndrome, is a rare, ciliopathic, autosomal recessive genetic disorder that causes defects in the action of cilia lining the respiratory tract (lower and upper, sinuses, Eustachian tube, middle ear) and fallopian tube, as well as in the flagella of sperm cells.
What is the ICD code for acute care?
Use a child code to capture more detail. ICD Code J98.0 is a non-billable code.
The ICD code J980 is used to code Primary ciliary dyskinesia
Primary ciliary dyskinesia (PCD), also immotile ciliary syndrome or Kartagener syndrome, is a rare, ciliopathic, autosomal recessive genetic disorder that causes defects in the action of cilia lining the respiratory tract (lower and upper, sinuses, Eustachian tube, middle ear) and fallopian tube, as well as in the flagella of sperm cells.
Coding Notes for J98.09 Info for medical coders on how to properly use this ICD-10 code
Inclusion Terms are a list of concepts for which a specific code is used. The list of Inclusion Terms is useful for determining the correct code in some cases, but the list is not necessarily exhaustive.
MS-DRG Mapping
DRG Group #011-013 - Tracheostomy for face, mouth and neck diagnoses with MCC.
ICD-10-CM Alphabetical Index References for 'J98.09 - Other diseases of bronchus, not elsewhere classified'
The ICD-10-CM Alphabetical Index links the below-listed medical terms to the ICD code J98.09. Click on any term below to browse the alphabetical index.
Equivalent ICD-9 Code GENERAL EQUIVALENCE MAPPINGS (GEM)
This is the official approximate match mapping between ICD9 and ICD10, as provided by the General Equivalency mapping crosswalk. This means that while there is no exact mapping between this ICD10 code J98.09 and a single ICD9 code, 519.19 is an approximate match for comparison and conversion purposes.
Summary
Primary ciliary dyskinesia is a disorder characterized by chronic respiratory tract infections, abnormally positioned internal organs, and the inability to have children (infertility). The signs and symptoms of this condition are caused by abnormal cilia and flagella.
Clinical features
List of clinical features of the condition/phenotype displayed from sources such as the Human Phenotype Ontology (HPO) and OMIM. For more information about the disease, please go to the disease information page.
How to treat ciliary dyskinesia?
[4] [5] Treatment is focused on the symptoms. People with PCD may be treated with chest physical therapy and breathing exercises to help remove excess mucous. Other treatments may include inhalants to help with breathing, and antibiotics to help treat and prevent infections. Surgery may be necessary to correct heart defects, and to remove damaged lung tissue. For people with severe lung and airway damage, lung transplant may be an option. Males with infertility may want to consider using donor sperm or intracytoplasmic sperm injection (ICSI) to have children. People with PCD should avoid smoking and exposure to smoke in general. In addition, regular exercise can strengthen the lungs and may improve lung function. [4] [5]
How many people have ciliary dyskinesis?
It is thought that about 1/16,000 – 1/20,000 people have primary ciliary dyskinesis (PCD). The incidence is higher in Norway and Japan. In the United States, it is estimated that about 12-17 thousand people have PCD. [1]
What is a PCD?
Listen. Primary ciliary dyskinesia (PCD) is an inherited disorder which affects the movement of tiny hair-like structures on body cells, known as cili a. Cilia are present on many types of cells, and particularly on those in the respiratory tract. In PCD, the cilia are abnormal, and don’t move correctly. People with this disorder cannot clear the ...
How is PCD diagnosed?
It is diagnosed based on the clinical symptoms. Other diagnostic tests may include ciliary analysis and genetic testing .
What tests are done for PCD?
Other diagnostic tests may include ciliary analysis and genetic testing . Treatment is based on taking care of the symptoms. The long-term outlook for people with PCD depends on the severity of the symptoms. People with frequent lung infections may experience permanent lung damage and require lung transplant.
Is primary ciliary dyskinesia autosomal recessive?
Listen. Most cases of primary ciliary dyskinesia (PCD) are inherited in an autosomal recessive pattern. [1] [2] [3] All individuals inherit two copies of each gene. To have PCD, a person must have a mutation in both copies of the responsible gene in each cell.
Is ciliary dyskinesia life threatening?
The long-term outlook for people with primary ciliary dyskinesia (PCD) is dependent on severity of respiratory symptoms. Generally, PCD is not thought to be life-threatening, but severe lung and airway disease can lead to permanent damage.
What are the consequences of impaired ciliary function?
The main consequence of impaired ciliary function is reduced or absent mucus clearance from the lungs, and susceptibility to chronic recurrent respiratory infections, including sinusitis, bronchitis, pneumonia, and otitis media . Progressive damage to the respiratory system is common, including progressive bronchiectasis beginning in early ...
What is the motility of the cilia?
PCD is a genetically heterogeneous disorder affecting motile cilia which are made up of approximately 250 proteins. Around 90% of individuals with PCD have ultrastructural defects affecting protein (s) in the outer and/or inner dynein arms, which give cilia their motility , with roughly 38% of these defects caused by mutations on two genes, DNAI1 and DNAH5, both of which code for proteins found in the ciliary outer dynein arm.
What is PCD in pulmonary?
Pulmonology. Primary ciliary dyskinesia ( PCD ), is a rare, ciliopathic, autosomal recessive genetic disorder that causes defects in the action of cilia lining the respiratory tract (lower and upper, sinuses, Eustachian tube, middle ear ), fallopian tube, and flagellum of sperm cells. The phrase "immotile ciliary syndrome" is no longer favored as ...
What test is used to diagnose ciliary beat pattern?
Several diagnostic tests for this condition have been proposed. These include nasal nitric oxide levels as a screening test, light microscopy of biopsies for ciliary beat pattern and frequency and electron microscopic examination of dynein arms, as the definite diagnosis method. Genetic testing has also been proposed but this is difficult given that there are multiple genes involved.
What is the role of DNAH5 in PCD?
The role of DNAH5 in heterotaxy syndromes and left-right asymmetry is also under investigation.
When was PCD first described?
The classic symptom combination associated with PCD was first described in 1904 by A. K. Siewert, while Manes Kartagener published his first report on the subject in 1933. The disorder is often now referred to as Siewert's syndrome or Siewert-Kartagener syndrome.
What are the elongated structures that make up the cilia and flagella?
Axonemes are the elongated structures that make up cilia and flagella. Additionally, there may be chemical defects that interfere with ciliary function in the presence of adequate structure. Whatever the underlying cause, dysfunction of the cilia begins during and impacts the embryologic phase of development.
Popular Posts:
- 1. icd 10 code for abnormal lpt
- 2. icd 10 code for family history of kidney cancer
- 3. icd 10 code for oa lumbar
- 4. icd 10 cm code for 85785253
- 5. icd 10 code for degenerative joint disease of the left foot
- 6. icd 10 code for post op fluid collection
- 7. icd 10 code for urethral hypermobility
- 8. icd 10 code for cirrhosis jaundice
- 9. icd-10 code for eema
- 10. what is the icd-10-cm code for chronic lower back pain