What is the ICD 10 code for testicular torsion?
N50 ICD-10-CM Diagnosis Code N50. Other and unspecified disorders of male genital organs 2016 2017 2018 2019 Non-Billable/Non-Specific Code. Type 2 Excludes torsion of testis (N44.0-) Other and unspecified disorders of male genital organs.
What is the ICD 10 code for bilateral testicular cancer?
Magnetic Resonance Imaging (MRI) of Bilateral Testicles ICD-10-CM Diagnosis Code N50.9 [convert to ICD-9-CM] Disorder of male genital organs, unspecified
What is testicular microlithiasis (TM)?
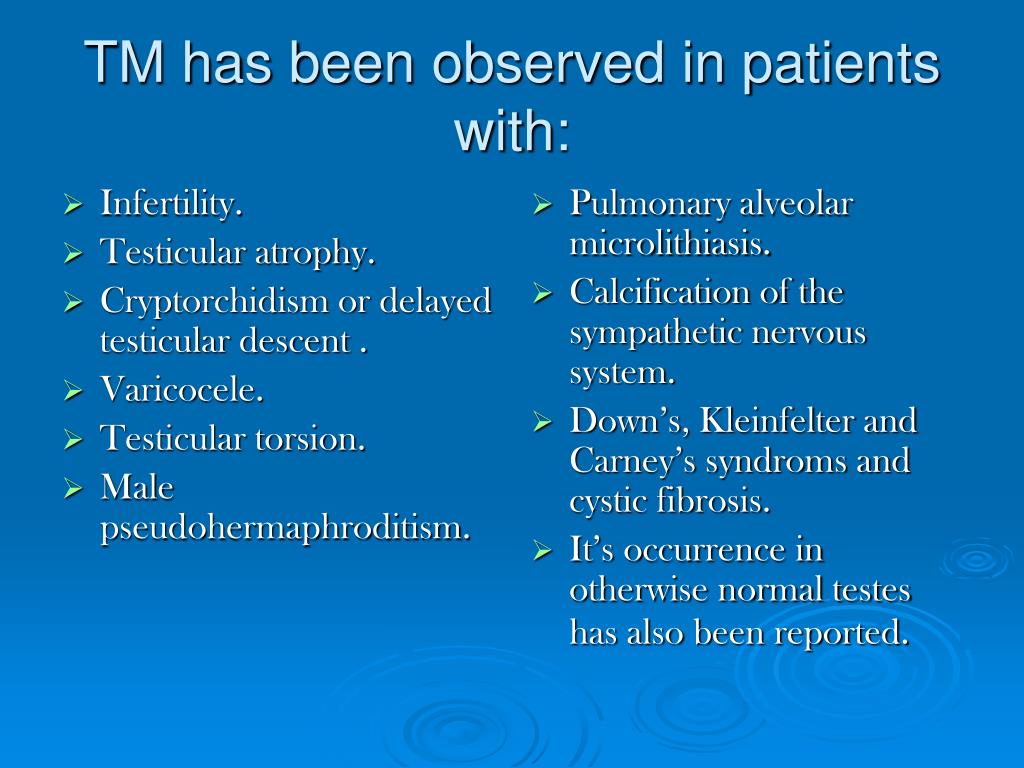
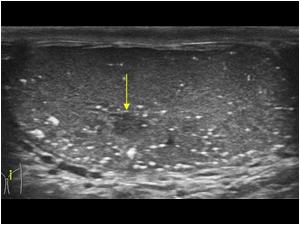
Testicular microlithiasis (TM) is a relatively rare condition detected incidentally during the ultrasound examination of the scrotum.
What is the relationship between bilateral testicular microlithiasis and carcinoma in situ?
Bilateral testicular microlithiasis is indicative of CIS (carcinoma in situ) in subfertile men. De Gouveia Brazao et al. reported that 20% of patients with bilateral testicular microlithiasis were diagnosed with CIS.
What is Microlithiasis?
Gargollo, M.D. Testicular microlithiasis (tes-TIK-yoo-lur my-kroh-lih-THIE-uh-sis) is a condition in which small clusters of calcium form in the testicles. It can be detected on an ultrasound exam of the scrotum. Several studies show a relationship between testicular microlithiasis and testicular cancer.
What is N50 89 diagnosis?
N50. 89 - Other specified disorders of the male genital organs | ICD-10-CM.
What is the ICD-10 code for testicular swelling?
Inflammatory disorders of scrotum The 2022 edition of ICD-10-CM N49. 2 became effective on October 1, 2021.
What is the ICD-10 code for epididymal mass?
Benign neoplasm of unspecified epididymis The 2022 edition of ICD-10-CM D29. 30 became effective on October 1, 2021. This is the American ICD-10-CM version of D29. 30 - other international versions of ICD-10 D29.
What is the ICD-10 code for testicular mass?
Benign neoplasm of unspecified testis D29. 20 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM D29. 20 became effective on October 1, 2021.
What is the ICD-10 code for orchitis?
ICD-10 code N45 for Orchitis and epididymitis is a medical classification as listed by WHO under the range - Diseases of the genitourinary system .
What is the diagnosis for ICD 10 code r50 9?
9: Fever, unspecified.
What is the ICD 10 code for left epididymitis?
ICD-10 code: N45. 9 Orchitis, epididymitis and epididymo-orchitis without abscess.
What does Orchialgia mean?
Introduction. Chronic orchialgia is defined as 3 months of intermittent or constant testicular pain that is significantly bothersome to the patient. It is the cause of about 2.5% to 5% of all urology consultations and currently affects about 100,000 men in the United States each year.
What is the ICD 10 code for epididymal Cyst?
ICD-10-CM Code for Cyst of epididymis N50. 3.
What is the ICD 10 code for Spermatocele?
ICD-10 code N43. 40 for Spermatocele of epididymis, unspecified is a medical classification as listed by WHO under the range - Diseases of the genitourinary system .
What is a testicular mass?
Testicular mass; Scrotal growth. A scrotal mass is a lump or bulge that can be felt in the scrotum. The scrotum is the sac that contains the testicles. The male reproductive system, viewed from a sagittal section. A scrotal mass is a lump or bulge that can be felt in the scrotum.
What are testicular microliths?
Based on the Renshew et al. study, two types of testicular microliths have been described: hematoxylin bodies and lamellated calcifications [8]. Under the optical and electron microscopes, microliths are found to consist of two zones, namely a central calcified zone and multi-layered envelope-stratified collagen fibres, both of which are covered with a thin fibrous capsule of spermatogenic epithelium. Microliths may occupy 30 to 40% of the seminiferous tubules and range in size from 50 to 400 μm. They do not typically affect Leydig cells and the majority of the uninvolved seminiferous tubules often have abnormal spermatogonia and reduced luminal diameters.
What causes TM in spermatocytes?
reported a number of theories proposed in an attempt to explain the origin of TM. Among them were hypotheses variously attributing TM to a range of causes, including liquefaction of protoplasmic dendrites of a spermatocyte, ectopic oocytes in dysgenetic testes, displaced spermatogonia, undifferentiated or desquamated calcified cells, deposition of glycoprotein around the nidus of cell material sloughed into the tubular lumen and abnormal Sertoli cells [9].
Where can microliths be found?
Microliths can be seen in the testis as well as in extra-testicular structures such as the lungs and the central nervous system, with genetic factors also thought to play a role in their development. Mutation in the SLC34A2 gene (4p15) has been found to occur in patients with pulmonary alveolar microliths.
Is there a link between testicular microlithiasis and testicular cancer?
A link between testicular microlithiasis and testicular cancer as well as male infertility has been analyzed. Follow-up is only recommended where risk factors of testicular cancer other than testicular microlithiasis are present.
Is TM associated with seminoma?
The authors suggest that TM may be associated positively with seminomas (p = 0.03) and negatively with embryonal cell carcinomas (p = 0.007). What is more, they reported a link between a higher TM count and a lower initial stage at diagnosis, which suggests that TM may be associated with less aggressive tumors (p = 0.02). No association was found between TM and age, tumor size and the presence of lymphovascular / rete testis invasion (p >0.12, respectively) [18]. The foregoing studies had not found elevated tumor markers in those with incidental TM, hence monitoring serum tumor markers in follow-up is not appropriate [14].
Is testicular microlithiasis a risk factor for testicular tumor?
Subfertility is reported to be a risk factor for a testicular tumor. Bilateral testicular microlithiasis is indicative of CIS (carcinoma in situ) in subfertile men. De Gouveia Brazao et al. reported that 20% of patients with bilateral testicular microlithiasis were diagnosed with CIS. Therefore, the prevalence of CIS in subfertile men with bilateral testicular microlithiasis is significantly higher than in patients without testicular microlithiasis (0.5%) and with unilateral testicular microlithiasis (0%) (p <0.0001) [23]. Thus, men with CIS are at particular risk for invasive testicular germ cell tumor (TGCT). An assessment of testicular microlithiasis is a valuable tool for the early diagnosis of this disease. Approximately 50% of CIS progresses to germ cell tumor within 5 years [24]. Nearly 20% of patients with a previous testicular germ cell tumor have TM in their contralateral testes. Those patients have an increased risk ratio of 8.9 for concurrent CIS compared with patients who do not have TM [25].
Popular Posts:
- 1. 2016 icd 10 code for facial droop
- 2. icd 10 code for shave
- 3. icd 10 code for smoking
- 4. icd 10 code for late effect of intraparenchymal hemorrhage
- 5. icd 10 code for ureteral calculus
- 6. icd 10 diagnosis code for pregnancy with 81025
- 7. icd 10 code for right inguinal mass
- 8. icd 10 code for post c section
- 9. icd 10 code for abnormal results of kidney function studies
- 10. icd-10 code for malignant neoplasm of head and neck