How do you reverse venous insufficiency?
- Wear compression stockings. They ease swelling and improve blood flow.
- Keep your feet elevated above your heart. When you can, do it for 15 minutes every 2 hours and while you sleep.
- Don't stand still for too long. Walk around often.
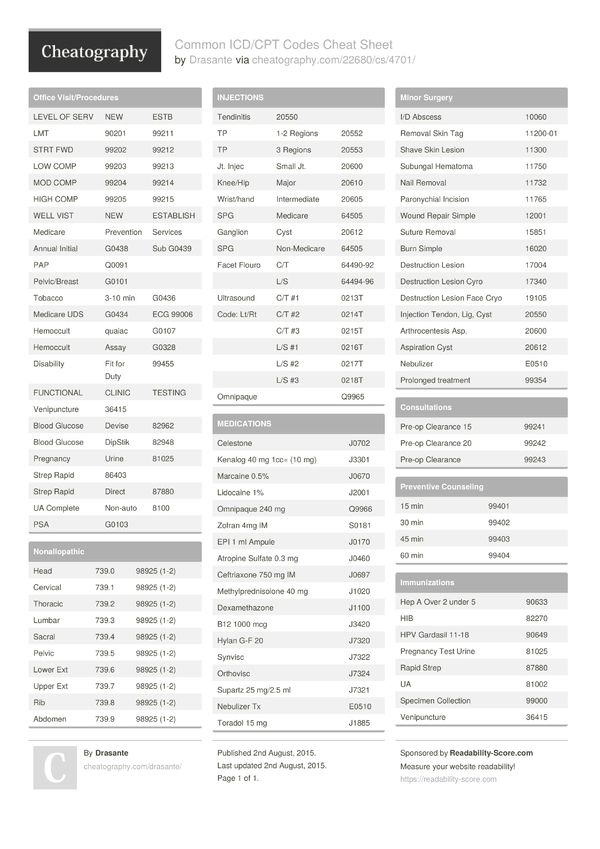
What is the ICD 10 diagnosis code for?
The ICD-10-CM is a catalog of diagnosis codes used by medical professionals for medical coding and reporting in health care settings. The Centers for Medicare and Medicaid Services (CMS) maintain the catalog in the U.S. releasing yearly updates.
How serious is chronic venous insufficiency?
Early symptoms of chronic venous insufficiency, like achy legs, might not seem serious. If left untreated, the condition may progress. Serious complications can arise from untreated chronic venous insufficiency. Poor circulation in the legs can cause ulcers to develop. These ulcers may be painful and slow to heal.
What is the ICD 10 code for poor circulation?
Unspecified disorder of circulatory system
- I99.9 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- The 2022 edition of ICD-10-CM I99.9 became effective on October 1, 2021.
- This is the American ICD-10-CM version of I99.9 - other international versions of ICD-10 I99.9 may differ.
Is venous insufficiency the same as venous hypertension?
Chronic venous hypertension occurs when there's increased pressure inside your veins. The term chronic venous hypertension is a medical term for what is more descriptively called chronic venous insufficiency.
What is the ICD-10 code for varicose veins with venous insufficiency?
Venous insufficiency (chronic) (peripheral) I87. 2 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM I87. 2 became effective on October 1, 2021.
What is the medical term for venous insufficiency?
Chronic venous insufficiency (CVI) is a condition that occurs when the venous wall and/or valves in the leg veins are not working effectively, making it difficult for blood to return to the heart from the legs. CVI causes blood to “pool” or collect in these veins, and this pooling is called stasis.
What is primary venous insufficiency?
Primary chronic venous insufficiency refers to the symptomatic presentation without a precipitating event and is due to congenital defects or changes in venous wall biochemistry. Recent studies suggest that approximately 70% of patients have primary chronic venous insufficiency and 30% have secondary disease.
Is venous insufficiency the same as peripheral vascular disease?
The difference between the two lies in the type of blood vessel that isn't working correctly. PAD affects your arteries, but CVI affects your veins.
What is the ICD-10 code for bilateral lower extremity varicose veins?
ICD-10 code I83. 813 for Varicose veins of bilateral lower extremities with pain is a medical classification as listed by WHO under the range - Diseases of the circulatory system .
What is the difference between primary and secondary venous insufficiency?
Primary venous insufficiency is of uncertain etiology, whereas secondary venous insufficiency is attributed to an acquired condition. The anatomic classification describes the superficial, deep, and perforating venous systems, with multiple venous segments that may be involved.
Is venous insufficiency systemic?
More recent investigations into the cellular and molecular aspects of venous insufficiency have shown that the disease is a complex multifactorial process reflecting both systemic abnormalities of connective tissue synthesis and cellular inflammatory reaction.
What is superficial venous insufficiency?
Superficial venous insufficiency (SVI) of the leg is defined as retrograde flow in the superficial veins of >0.5 seconds in duration. It is caused by a pathophysiological cycle initiated and driven by inflammatory processes that damage the vein walls and its valves.
What is venous insufficiency chronic peripheral?
Chronic venous insufficiency occurs when your leg veins don't allow blood to flow back up to your heart. Normally, the valves in your veins make sure that blood flows toward your heart. But when these valves don't work well, blood can also flow backwards. This can cause blood to collect (pool) in your legs.
What are the stages of venous insufficiency?
We want you to understand the five main stages of chronic venous insufficiency, which include:Stage 1: Spider Veins. Your first sign of trouble may be the development of spider veins. ... Stage 2: Varicose Veins. ... Stage 3: Leg Swelling. ... Stage 4: Skin Discoloration. ... Stage 5: Venous Ulcers.
How do you diagnose venous insufficiency?
Diagnostic TestsDuplex Ultrasound. A duplex ultrasound combines Doppler and conventional ultrasound to produce two-dimensional, moving images of blood vessels in the legs. ... Magnetic Resonance Venogram. ... CT Venogram. ... Venogram.
What is the best treatment for venous insufficiency?
Treatment may include:Improving blood flow in your leg veins. Keeping your legs raised (elevated) can reduce swelling and help increase blood flow. ... Medicines. ... Endovenous laser ablation or radiofrequency ablation (RFA). ... Sclerotherapy. ... Surgery.
What is the most serious complication of venous insufficiency?
Left untreated, these damaged veins can cause serious complications, such as ulcers, bleeding, and a potentially fatal condition called deep vein thrombosis.
Can you reverse chronic venous insufficiency?
First, I want to be clear that there is no way to actually reverse the cause of venous insufficiency, only the symptoms. Damaged valves inside the vein cannot be repaired, but there are plenty of ways to minimize the impact of the reflux they cause. Many of my patients do eventually become symptom-free.
Who is at risk for chronic venous insufficiency?
Women are actually up to three times more likely than men to develop venous disease. This is because changes in hormone levels can weaken the vein walls and affect how well the valves work. In fact, those who are pregnant or have had multiple births are also more at risk due to hormonal changes.
What is the ICd 10 code for venous insufficiency?
I87.2 is a valid billable ICD-10 diagnosis code for Venous insufficiency (chronic) (peripheral) . It is found in the 2021 version of the ICD-10 Clinical Modification (CM) and can be used in all HIPAA-covered transactions from Oct 01, 2020 - Sep 30, 2021 .
Do you include decimal points in ICD-10?
DO NOT include the decimal point when electronically filing claims as it may be rejected. Some clearinghouses may remove it for you but to avoid having a rejected claim due to an invalid ICD-10 code, do not include the decimal point when submitting claims electronically. See also: Dermatitis (eczematous) L30.9.

Popular Posts:
- 1. icd 10 code for status post ventriculoperitoneal shunt
- 2. icd-10-cm code for chronic obstructive asthma
- 3. icd 10 code for dyslipidemia\
- 4. icd 10 code for family history of depression
- 5. icd 10 code for superficial occlusion stenosis femoral artery
- 6. icd 10 code for a1a
- 7. icd 10 code for neuropathic foot ulcer not diabetic wagner grade 3
- 8. icd 9 code for screening for lung cancer
- 9. icd-10-cm code for farmer's lung
- 10. what is the icd 10 code for rinary incontinence