92071: Fitting of contact lens for treatment of ocular surface disease. 92072: Fitting of contact lens for management of keratoconus, initial fitting only. Unfortunately, not every medical insurance carrier will pay for these codes.
What does the CPT code 92071 mean?
Code 92071 Definition. 92071 Fitting of contact lens for treatment of ocular surface disease. This code is used when a prescriptive or nonprescriptive contact lens is fitted for therapeutic purposes to treat a diseased or injured eye. A soft contact lens is placed on the cornea to protect a damaged eye or help heal a corneal ulcer or other damage.
What is a 92072 contact lens?
Definition. 92072 Fitting of contact lens for management of keratoconus; initial fitting. This definition covers the fitting of a prescriptive or nonprescriptive contact lens to treat keratoconus in order to reshape the cornea to correct the patient’s vision.
What is the CPT code for OSD in the eye?
▸ Employ CPT 92071, which is the code for fitting a contact lens for the treatment of OSD. Be sure to indicate the specific eye (RT or LT) because this code is unilateral in nature.
Is the modifier 25 missing from code 92071?
We have appended modifier 25 to code 92071. But they are denying it saying a modifier is missing. Can anyone give me insight to this? I am new to the eye care billing world. Click to expand... 25 is an E&M modifier so it does not belong on the 92071.
Is 92071 considered a procedure?
The Current Procedural Terminology (CPT®) code 92071 as maintained by American Medical Association, is a medical procedural code under the range - Ophthalmological Examination and Evaluation Procedures.
How do I bill CPT 92071?
Assuming your treatment plan includes applying a soft bandage contact lens, you would use 92071 to describe this service. CPT Code 92071 is defined as: “Fitting of contact lens for treatment of ocular surface disease.”
Do you need a modifier for 92071?
92071 (Fitting of Contact Lens for Treatment of Ocular Surface Disease): This code applies to fitting a contact lens to manage ocular surface disease. Right/Left eye can be specified with the appropriate modifier (i.e., 92071-RT).
Is 92071 a bilateral code?
Effective January 1, 2012, there is a new code, 92071 (Fitting of contact lens for treatment of ocular surface disease). Medicare defines this code as bilateral; bill once whether one or both eyes are treated.
Does Medicare pay for 92071?
A. CPT 92071 is defined as a “unilateral” service, so reimbursement is per eye. In 2021, the national Medicare Physician Fee Schedule allowable for 92071 is $37.34 in-office and $32.80 in a facility. This amount is adjusted by local wages indices in each area.
Can you bill for office visit and procedure?
Can you bill an E/M service on the same day as a minor procedure? Sometimes yes, sometimes no. The decision to perform a minor procedure is included in the payment for the procedure, unless a significant and separate E/M is needed, performed and documented.
What is the CPT code for RGP contact lenses?
Use CPT 92310, which is defined as: “Prescription of optical and physical characteristics of and fitting of contact lens, with medical supervision of adaptation; corneal lens, both eyes, except for aphakia.”
When do you use modifier 50?
bilateral proceduresUse modifier 50 to report bilateral procedures performed during the same operative session by the same physician in either separate operative areas (e.g., hands, feet, legs, arms, ears) or in the same operative area (e.g., nose, eyes, breasts).
What is ocular surface disorder?
DEFINITION. Ocular surface disease indicates damage to the surface layers of the eye, namely the cornea and conjunctiva. There are many causes ocular surface disease, but the 2 most common ones are “dry eye syndrome” and “blepharitis”.
How do you bill bandage contact lenses?
Q: How should I bill for a bandage contact lens? The CPT code for this is 92070 (Fitting of contact lens for treatment of disease, including supply of lens).
Does Medicare pay for medically necessary contact lenses?
While Medicare covers some vision services, it doesn't usually pay for eye exams or contact lenses. Some of the vision services original Medicare (parts A and B) may cover include: annual glaucoma test for people at high risk (including those with diabetes or a family history of glaucoma)
How do you code a corneal rust ring?
Since the rust ring is considered foreign to the cornea, the removal is reported either using code 65220 or 65222 as appropriate.
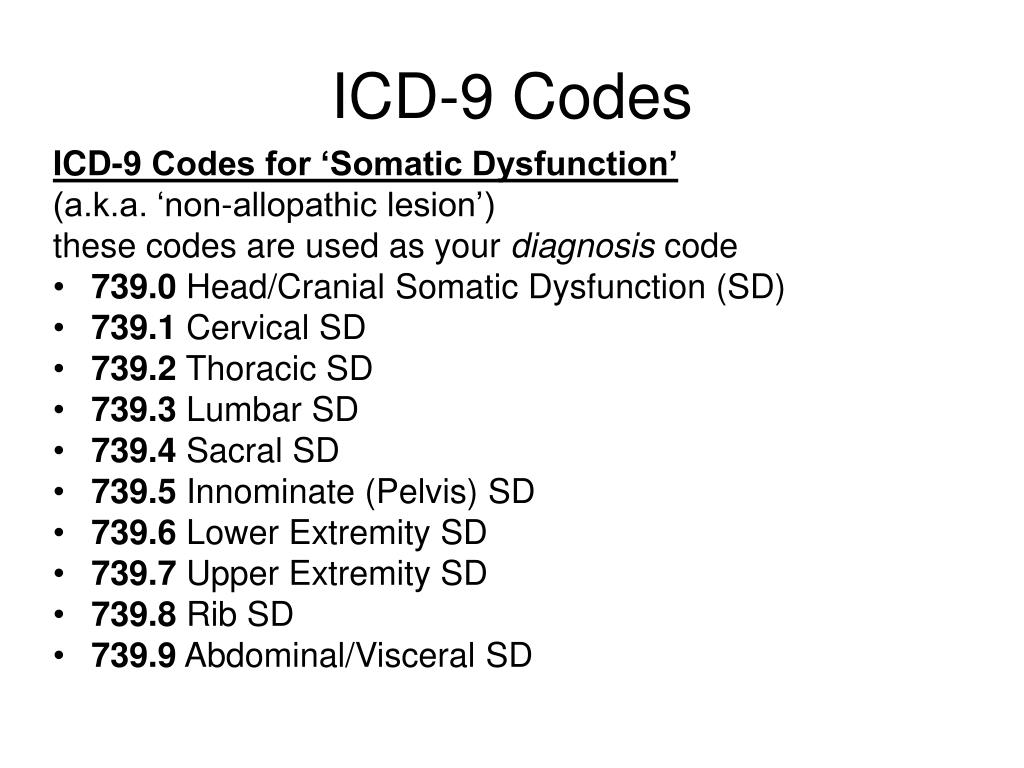
ICD-10 Specifics
ICD-10 has a slew of codes specific to corneal abrasions and sports-related ocular injuries, and it can be a challenge to know them all. If you were to correctly and completely code the patient example above, it would look like this:
Foreign Body Complications
If your encounter involves a foreign body, this changes everything for CPT coding.
How to submit for reimbursement
F or some ocular surface disease (OSD) patients who do not feel relief from symptoms with standard treatments, such as warm compresses, lid scrubs and artificial tears, bandage contact lenses and biological corneal bandages can be used to quell ocular dryness, foreign-body sensation and pain, while safeguarding the cornea from damage.
JASON R. MILLER, O.D., M.B.A., F.A.A.O
F or some ocular surface disease (OSD) patients who do not feel relief from symptoms with standard treatments, such as warm compresses, lid scrubs and artificial tears, bandage contact lenses and biological corneal bandages can be used to quell ocular dryness, foreign-body sensation and pain, while safeguarding the cornea from damage.
FOLLOW THE STEPS
Step 1 The first step for specialty lens billing is to contact a patient’s insurance (vision and/or medical) and obtain a prior authorization for medically necessary contact lens coverage. This may not occur until after you see patients, so often it cannot be done prior to their appointment.
WHAT QUALIFIES AS A MEDICALLY NECESSARY CONTACT LENS?
Each insurance company has its own rules and guidelines on what qualifies for medically necessary contact lenses. Some have a definitive list of patient diagnosis codes that would qualify them for medically necessary lens benefits. Some may also further differentiate diseases into mild, moderate, and severe.
HOW DO I SET UP A FEE SCHEDULE FOR MEDICALLY NECESSARY CONTACT LENSES?
This is a common question that is asked by many providers, and I also had to determine what was fair for my practice. There are a few strategies for determining an appropriate fee schedule. There is no right or wrong method; practitioners should use the one that works best for them.
FINAL THOUGHTS
To maximize efficiency and understanding of billing medically necessary contact lenses, it is advisable to read through your provider manual to know exactly what that specific insurance carrier will cover. Contacting insurance companies and having them walk you through the information can also be useful.
Popular Posts:
- 1. icd-10 code for stage 1 pressure ulcer of the left heel
- 2. icd 10 code for crp screening
- 3. icd 10 code for abnormal t wave
- 4. icd 10 code for lab work
- 5. icd 10 code for pustular vesiciular in oropharynx
- 6. icd 10 code for balance instability
- 7. icd 10 code for lcis
- 8. icd 10 cm code for chest heaviness,
- 9. icd 10 code for low sex drive
- 10. icd 10 code for ulverative colitis