What drugs are used to treat congestive heart failure?
Treatment
- Medications. Doctors usually treat heart failure with a combination of medications. ...
- Surgery or other procedures. Surgery or other procedures to implant cardiac devices may be recommended to treat the underlying problem that led to heart failure.
- Palliative care and end-of-life care. ...
What medications cause congestive heart failure?
Other types of drugs that can bring on heart failure include:
- Antifungal medications
- Cancer medications
- Stimulants
- Antidepressants
- Tumor necrosis factor (TNF) inhibitors
What are symptoms of left heart failure?
These symptoms cause the heart to try to pump harder and cause further damage such as:
- Enlarged Heart
- Rapid Heart Rate
- High Blood Pressure
- Less Blood Flowing to the Arms and the Legs.
What is the ICD 10 code for exacerbation of CHF?
- Code: I50.9.
- Code Name: ICD-10 Code for Heart failure, unspecified.
- Block: Other forms of heart disease (I30-I52)
- Details: Heart failure, unspecified.
- Excludes 2: fluid overload (E87.70)
- Excludes1: neonatal cardiac failure (P29.0)
- Excludes2: cardiac arrest (I46.-)"
- Guidelines: Diseases of the circulatory system (I00-I99)
How do you code Acute on chronic heart failure?
I50. 23 - Acute on chronic systolic (congestive) heart failure | ICD-10-CM.
What is the ICD-10 code for CHF unspecified?
I50.99 – Heart Failure, Unspecified. Code I50. 9 is the diagnosis code used for Heart Failure, Unspecified.
What does Acute on chronic heart failure mean?
Acute heart failure can result from an event such as a viral infection or blockage affecting an artery around the heart. Doctors may call this “de novo” acute heart failure. It may instead result from damage in the heart, which may have developed over time. Doctors may call this “acute on chronic” heart failure.
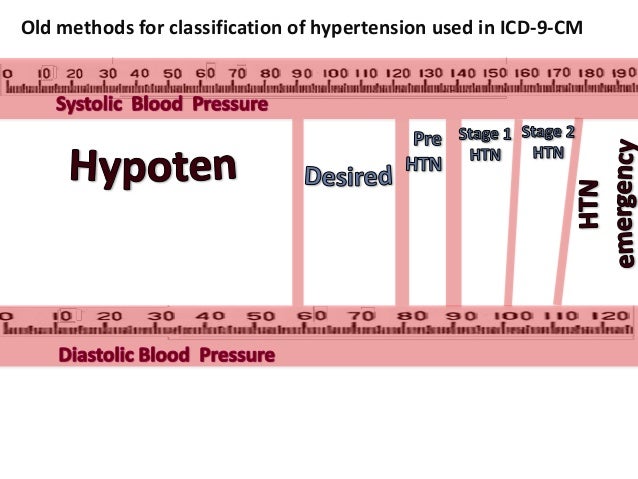
What is the ICD-9 code for congestive heart failure?
Table 1ICD-9-CM diagnosis codeDiagnosisDescriptionHeart failure428.0 Congestive heart failure, unspecified428.1 Left heart failure428.2 Systolic heart failure42 more rows•Mar 29, 2017
What is DX code I10?
ICD-Code I10 is a billable ICD-10 code used for healthcare diagnosis reimbursement of Essential (Primary) Hypertension.
What is the difference between acute and chronic congestive heart failure?
Q: What is the difference between acute and chronic heart failure? A: Chronic heart failure is generally a condition that develops gradually over time, whereas acute heart failure, in most cases, occurs very suddenly and should be considered a medical emergency requiring immediate intervention.
What's the difference between acute heart failure and congestive heart failure?
In short, they are the same, but we thought it would be helpful to provide information on what congestive heart failure is, the types of heart attack someone might have, and how heart failure is diagnosed.
What is the difference between congestive heart failure and chronic heart failure?
Congestive heart failure (CHF) refers to the inadequate functioning of the heart muscle such that fluid builds up in the lungs, abdomen, feet, and arms (hence the term "congestive"). The condition can either be acute (meaning it occurs suddenly, with a sharp rise) or chronic (which means it occurs over the long term).
What does acute on chronic mean?
The term acute on chronic is used in medicine to describe situations when someone with a chronic condition, such as chronic obstructive pulmonary disease, also develops an acute condition, such as pneumonia.
How long can you live with acute heart failure?
For example, the 5-year survival rate for patients with heart failure is about 76%....Table: Survival rates for patients with heart failure.Survival (in years)Survival rate (in percentages)1About 75.9% on average5About 45.5% on average10About 24.5% on averageJul 15, 2021
Is acute heart failure serious?
Acute heart failure is a sudden, life-threatening condition in which the heart is unable to do its job. The heart is still beating, but it cannot deliver enough oxygen to meet the body's needs. This condition requires emergency medical care.
What stage is chronic heart failure?
What are the Stages of CHF?StageSymptomsINo notable symptomsIIPhysical activity may lead to symptoms such as palpitations, shortness of breath, and fatigue.IIIAny physical activity is likely to result in notable symptoms, more severe than Stage II.1 more row•Aug 8, 2019
What is the clinical sign of heart failure?
Clinical symptoms of heart failure include: unusual dyspnea on light exertion, recurrent dyspnea occurring in the supine position, fluid retention or rales, jugular venous distension, pulmonary edema on physical exam, or pulmonary edema on chest x-ray presumed to be cardiac dysfunction.
What is heart failure accompanied by?
Heart failure accompanied by edema, such as swelling of the legs and ankles and congestion in the lungs.
What are the symptoms of a heart failure?
Signs and symptoms include shortness of breath, pitting edema, enlarged tender liver, engorged neck veins, and pulmonary rales.
When will ICD-10-CM I50.9 be released?
The 2022 edition of ICD-10-CM I50.9 became effective on October 1, 2021.
What is the term for a condition in which the heart is unable to pump out enough blood to meet the metabolic?
A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction.
What is the HF code for PMH?
If a provider lists “HF” in the PMH section your institution utilizes, you may pick up I50.9, heart failure, unspecified, but there is no “chronic heart failure, unspecified” code, like there are type-specified HF, acuity-unspecified codes. If they were to document “chronic heart failure,” you just get I50.9.
What percentage of HCCs are not complications or comorbidities?
Chronic conditions can be resource-intensive, so they may have an impact on the population health risk adjustment model when they have none on the inpatient model. Forty percent of HCCs are neither complications or comorbidities (CCs) nor major CCs (MCCs). (For the CMS-HCC model, go online to ...
What is HCC 167?
However, sequelae of major head trauma and skull fractures are also nestled in HCC 167, Major Head Injury.
What is the risk adjustment factor for HCC 106?
Although I73.9, peripheral vascular disease, unspecified lives in HCC 108, if what you really have is a patient with atherosclerosis of a leg with ulceration, you should really be in HCC 106 – which, according to the hierarchy, should yield a risk adjustment factor of 1.461 instead of 0.298. The provider should give the specificity of vessel and the linkage of symptoms or sequelae like claudication, rest pain, ulceration, or gangrene. Be sure to refer to the most up-to-date Disease Hierarchies – 106, Atherosclerosis of the Extremities with Ulceration or Gangrene, supersedes 107, 108, 161, and 189.
Can you code HF?
If a provider doesn’t mention the condition at all, but you note the patient is on meds for heart failure (HF), and prior admissions note HF, you can’t code it, but it should clue you in that the patient may have chronic HF. It needs to be documented in this encounter. You should query.
Is past medical history a coding code?
Providers don’t think of “past medical history” as being “history of,” in the coding sense. The latter, “personal history of,” lands a code in the Z85-87 subcategories, whereas chronic conditions are listed in the system-specific sections.
Is there a disconnect between coders and clinicians regarding the concept of “chronic” conditions?
There is a disconnect among coders and clinicians regarding the concept of “chronic” conditions. All clinicians have interviewed a patient who denies any past medical history, but when confronted with their medication list, they will admit to having high blood pressure and high cholesterol. If controlled, the patients just don’t think of those conditions as being chronic.
Popular Posts:
- 1. icd 10 code for dvt bilateral lower extremities
- 2. icd 10 code for brca screening
- 3. icd 10 cm code for osteitis deformans of skull
- 4. icd-10 code for incisional ventral hernia
- 5. icd 10 code screening for cystic fibrosis
- 6. icd 10 code for pain of left upper extremity
- 7. 2017 icd 10 code for removal desmoid tumor right rectus
- 8. icd-10 code for oa of cervical spine
- 9. icd 10 code for status post artery stents
- 10. icd 10 code for osteophyte spurring thigh