What is the ICD-10 diagnosis code for ADHD?
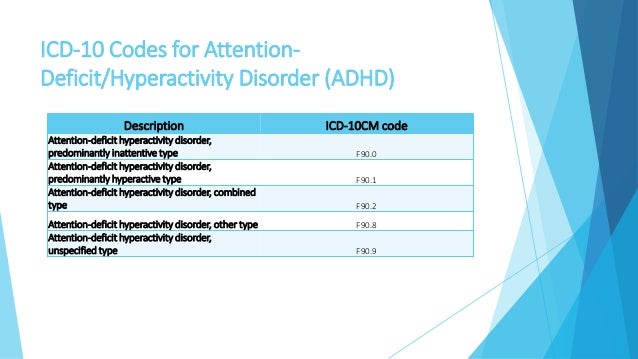
Coding ADHD in ICD-10 ICD-10-CM category F90. - includes ADHD as well as attention deficit syndrome with hyperactivity. It excludes anxiety disorders (F40. - and F41.May 16, 2016
What is ADHD in adults called?
Adult attention-deficit/hyperactivity disorder (ADHD) is a mental health disorder that includes a combination of persistent problems, such as difficulty paying attention, hyperactivity and impulsive behavior.Jun 22, 2019
What is the ICD-10 code for ADHD ADD without hyperactivity?
ICD-10 code: F98. 80 Attention deficit disorder without hyperactivity with onset usually occurring in childhood and adolescence - gesund.bund.de.
What is the ICD 9 code for ADHD?
ICD-9-CM code 314.00 is defined as “attention deficit disorder without mention of hyperactivity.” Thus, the taxonomy of this disorder seems to produce the oxymoronic situation that patients with ADD coded as 314.00 (no hyperactivity) are a subset of 314 (hyperkinetic syndrome) but are commonly referred to as patients ...Sep 7, 2007
Who diagnoses ADHD in adults?
ADHD in adults is often diagnosed by the primary care doctor, a psychiatrist, or a psychologist,. To diagnose ADHD in adults, the doctor will need a history of the adult's behavior as a child.Mar 9, 2021
What's the difference between ADD and ADHD in adults?
ADHD is the official, medical term for the condition — regardless of whether a patient demonstrates symptoms of hyperactivity. ADD is a now-outdated term that is typically used to describe inattentive-type ADHD, which has symptoms including disorganization, lack of focus, and forgetfulness.Jan 7, 2022
Is ADHD and ADD the same?
ADHD is sometimes referred to as ADD (attention-deficit disorder) but ADD is an older term. up until 1987, when the word “hyperactivity” was added to the name. Before that, say in 1980, a child would be diagnosed with ADD, either with or without hyperactivity.
Is ADHD a billable diagnosis?
Attention-deficit hyperactivity disorder, predominantly inattentive type. F90. 0 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
What is the ICD-10 code for ASD?
The ICD-10-CM code for ASD—F84. 0 (autistic disorder)—should be the physician's or psychologist's diagnosis (typically required by payers) of the underlying medical condition, documented in the patient's medical record.May 1, 2019
What is the ICD 11 code for ADHD?
6A05 Attention deficit hyperactivity disorder - ICD-11 MMS.
What is unspecified ADHD?
The unspecified ADHD category is used in situations in which the clinician chooses not to specify the reason that the criteria are not met for the ADHD or for a specific neurodevelopmental disorder and includes presentation in which there is insufficient information to make a more specific diagnosis.
What is ADHD disorder?
ADHD is one of the most common neurodevelopmental disorders of childhood. It is usually first diagnosed in childhood and often lasts into adulthood. Children with ADHD may have trouble paying attention, controlling impulsive behaviors (may act without thinking about what the result will be), or be overly active.
What is ADHD coding?
Attention-Deficit/Hyperactivity Disorder ( ADHD) is a chronic neurobehavioral disorder and often associated with serious areas of impairment and comorbidities over a life span. Physician practice coding professionals are at the forefront to ensure quality ICD-10-CM coded data across a life span for ADHD. In ICD-10-CM, ADHD coding over a life span requires clinical coding expertise across multi-physician specialties including but not limited to psychiatry, pediatrics, internal medicine, and family practice. This article summarizes how complete and accurate ADHD ICD-10-CM coding results in complete and quality coded data for the physician office provider setting.
What are the coexisting conditions of ADHD?
2 Across a life span, some coexisting conditions with ADHD include conduct disorder, depression, and anxiety, which may occur during both childhood and adulthood life stages.
What is a comprehensive evaluation?
A comprehensive evaluation is required to diagnose ADHD and consists of a thorough diagnostic interview, information obtained from independent sources such as family members or teachers, diagnostic symptom checklists, standardized behavior rating scales for ADHD, and other types of clinical assessment testing as defined by the clinician .
Why was ADHD moved to the neurodevelopmental disorders chapter?
ADHD was moved to the neurodevelopmental disorders chapter to better reflect how brain development correlates with ADHD. Thus, with the introduction of DSM-5, ADHD is no longer classified as a childhood disorder but as a chronic lifelong disorder.
What is the best treatment for ADHD?
Effective treatment examples include long-term medication therapy, academic intervention, and cognitive behavioral therapy. Medication (stimulant and non-stimulant) often provides the first line of treatment for many individuals with ADHD, but not all.
What is the DSM-5?
The American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) provides standardized diagnostic criteria and clinical guidelines for use in the comprehensive evaluation for ADHD.
When was the DSM 5 released?
The DSM-5 edition, released in 2013, incorporated ADHD diagnostic criteria updates, which resulted in more age-appropriate and slightly broadened diagnostic criteria that affects how the disorder is diagnosed in older adolescents and adults. Noteworthy DSM-5 ADHD diagnostic criteria updates in this area include:
What is the ICd 10 code for inattentive type?
F90.0 is a valid billable ICD-10 diagnosis code for Attention-deficit hyperactivity disorder, predominantly inattentive type . It is found in the 2021 version of the ICD-10 Clinical Modification (CM) and can be used in all HIPAA-covered transactions from Oct 01, 2020 - Sep 30, 2021 .
Do you include decimal points in ICD-10?
DO NOT include the decimal point when electronically filing claims as it may be rejected. Some clearinghouses may remove it for you but to avoid having a rejected claim due to an invalid ICD-10 code, do not include the decimal point when submitting claims electronically. See also: Disorder (of) see also Disease.
What are the characteristics of ADHD?
Inattention, hyperactivity and impulsivity are the three key characteristics that define ADHD and the way these features present varies from individual to individual. With effective and timely diagnosis and treatment of children and adolescents, ADHD symptoms can addressed and corrected to achieve optimum outcomes.
What type of ADHD is documented in clinical documentation?
The physician must also document the specific type of ADHD: Predominantly inattentive type, Predominantly hyperactive-impulsive type or Combined type.
What is the DSM 5 for ADHD?
The DSM-5 list classifies ADHD in three presentations – Predominantly Inattentive, Hyperactive-Impulsive and Combined. Predominantly inattentive – difficulty with organization and paying attention.
What is the diagnosis of ADHD?
Attention deficit hyperactivity disorder (ADHD) is a chronic neurobehavioral disorder that is typically diagnosed in children and is characterized by symptoms such as hyperactivity and impulsivity, and/or inattention. In the majority of cases, symptoms continue into adulthood.
What is the code for ADHD?
If signs and symptoms of ADHD are absent, screening for ADHD can be reported using code Z13.4, encounter for screening for certain developmental disorders in childhood.
What are the coexisting conditions of ADHD?
Common coexisting conditions in children with ADHD include disorders of mood, conduct, learning, motor control, language and communication and anxiety disorders Adults with ADHD may also have personality disorders, bipolar disorder, obsessive-compulsive disorder and substance misuse.
What is the DSM-5?
The Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) provides the clinical criteria and guidelines for diagnosing ADHD. To make a diagnosis, children should have six or more symptoms of the disorder present; adolescents 17 and older and adults should have at least five of the symptoms present.
How many children with ADHD receive psychological services?
Only 40-50 percent of young children with ADHD receive psychological services. Many parents resort immediately to stimulant or non-stimulant medication, which could have detrimental side effects. The CDC provides many resources for parents as well as clinical guidelines for providers.
How long does ADHD last?
The symptoms have lasted longer than six months, and they impair school, work, home life, or relationships in more than one setting. Clinical documentation requirements for ADHD. Clinical documentation must clearly differentiate ADHD from the following conditions: Hyperkinesia. Hyperkinetic syndrome.
What happens if you leave ADHD untreated?
Children with the condition may fall behind in school, have difficulty maintaining friendships, find themselves unable to accomplish basic tasks, or have conflicts with others.
What is a F90 note?
Category F90.- includes a note at the beginning indicating that these codes may be used regardless of the patient’s age. Note that these disorders generally have onset during childhood, but they may continue through a patient’s life. In some cases, patients may not be diagnosed until adulthood.
How many symptoms are there for ADHD?
Combined: These individuals have symptoms of inattention, hyperactivity, and impulsivity. For a clinical diagnosis of ADHD, an individual must exhibit six or more symptoms of one of the types of ADHD and also meet each of the following three criteria: The symptoms caused problems before the age of 7.
What are the three types of ADHD?
It’s important for parents, providers, and teachers to be able to recognize the three types of ADHD: Inattentive: Individuals with this type of ADHD fail to pay close attention to details and make careless mistakes in schoolwork and other activities.
Who is Kim Carr?
Kim Carr brings more than 30 years of health information and clinical documentation improvement management experience and expertise to her role as Director of Clinical Documentation, where she provides oversight for auditing and documentation improvement for HRS clients. Prior to joining HRS, Kim worked as a consultant implementing CDI programs in varied environments such as level-one trauma centers, small community hospitals and all levels in between.#N#Before joining the consultant arena, Kim served as Manager of CDI in an academic level-one trauma center. She was responsible for education and training for physicians and clinical documentation specialists. Over the past 30 years, Kim has held several HIM positions; including HIM Coding Educator, Quality Assurance/Utilization Management Coordinator, DRG Coding Coordinator and Coding Manager. Kim holds a degree in Health Information Management and is a member of AHIMA, THIMA, ACDIS and AAPC.
What is differential diagnosis?
Differential Diagnosis. Mixed disorders are common, and pervasive developmental disorders take precedence when they are present. The major problems in diagnosis lie in differentiation from conduct disorder: when its criteria are met, hyperkinetic disorder is diagnosed with priority over conduct disorder.
Why are hyperkinetic children prone to accidents?
Hyperkinetic children are often reckless and impulsive, prone to accidents, and find themselves in disciplinary trouble because of unthinking (rather than deliberately defiant) breaches of rules.
When hyperkinesis was present in childhood, but has disappeared and been succeeded by another condition, such as answer
When hyperkinesis was present in childhood, but has disappeared and been succeeded by another condition, such as dissocial personality disorder or substance abuse, the current condition rather than the earlier one is coded.
When do hyperkinetic disorders occur?
Hyperkinetic disorders always arise early in development (usually in the first 5 years of life).
Why do kids get hyperactive?
Acute onset of hyperactive behaviour in a child of school age is more probably due to some type of reactive disorder (psychogenic or organic), manic state, schizophrenia, or neurological disease (e.g. rheumatic fever). Excludes: anxiety disorders. mood (affective) disorders.
What is the standard for judgement?
The standard for judgement should be that the activity is excessive in the context of what is expected in the situation and by comparison with other children of the same age and IQ. This behavioural feature is most evident in structured, organized situations that require a high degree of behavioural self-control.
Is hyperkinesis more common in boys than girls?
Nevertheless, current evidence favours the separation of a group in which hyperkinesis is the main problem. Hyperkinetic disorders are several times more frequent in boys than in girls. Associated reading difficulties (and/or other scholastic problems) are common.
Is F98.8 a pediatric code?
In addition, the 2016 book does include the indicator that F98.8 is a pediatric only code; however this has been removed in 2017. Again, I'm guessing it is because the code descriptor for F98.8 states the condition "usually originates in childhood or adolescents," not that the patient is be a child/adolescent.
Can you use F90.0 without documentation?
The F98.8 states onset occurring in childhood not thatbit cannot be used for an adult. You may need to appeal with documentation. But you cannot assign F90.0 without the documentation to support it.
Popular Posts:
- 1. icd 9 code for blindness one eye
- 2. icd 10 code for acute steroid induced cardiac arrhythmia
- 3. icd-10 code for pans
- 4. icd 10 code for left foot ulcer unstageable
- 5. icd 10 code for fall while snowboarding
- 6. icd 10 code for gingivostomatitis
- 7. icd 10 code for family hx of melanoma
- 8. icd 10 code for strain of chest wall
- 9. icd 10 code for injury of right great toe
- 10. what is the icd 10 code for cervical spine nerve root injury