What is the ICD-10 code for Parkinson's dementia?
Disease, Parkinson: You will see Parkinsonism dementia listed with the codes G31. 83 and F02. 80.
What is ICD-10 code for Parkinson's disease?
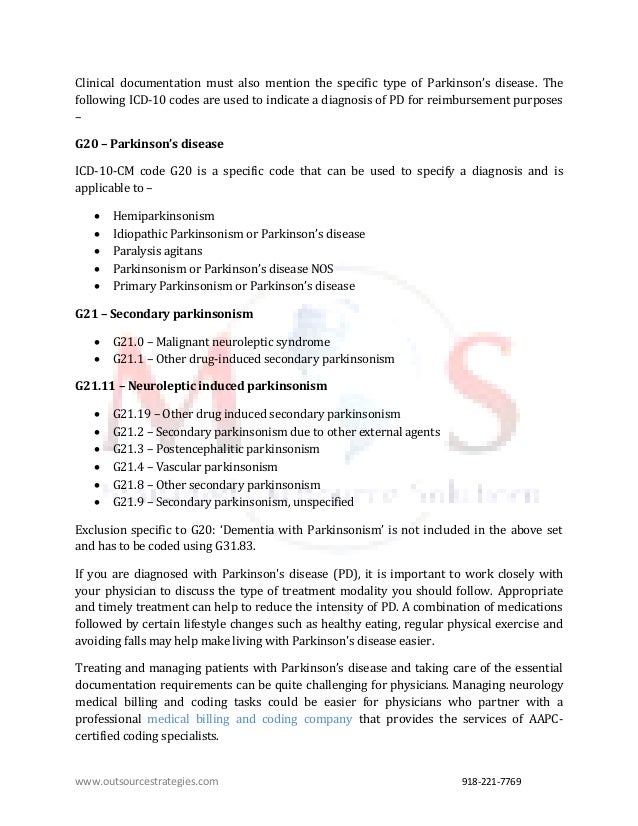
ICD-10 code G20 for Parkinson's disease is a medical classification as listed by WHO under the range - Diseases of the nervous system .
Do you have to code dementia with Parkinson's disease?
ICD-10-CM Coding: You will see Parkinsonism dementia listed and an additional code F02. 80 which appears in brackets and indicates this code would be assigned also but as a secondary. In the tabular code G20 represents PD, and it would be sequenced first, followed by the manifestation(s).
What is the correct code and sequencing for dementia and Parkinson's disease?
Let's Discuss the Correct Coding When coding Parkinson's disease with dementia take a look at the alphabetic index: Parkinsonism (idiopathic) (primary) G20, with dementia G31. 83 [F02. 80]. The brackets mean that the F02.
What is the ICD-10 code for Alzheimer's disease?
ICD-10 code G30. 9 for Alzheimer's disease, unspecified is a medical classification as listed by WHO under the range - Diseases of the nervous system .
What is the ICD-10 code for Alzheimer's dementia?
Alzheimer's disease, unspecified G30. 9 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM G30. 9 became effective on October 1, 2021.
Can a person have both Alzheimer's and Parkinson's?
While it's not common, it's possible to have both diseases at the same time. Alzheimer's disease always causes dementia; Parkinson's disease, a movement disorder, can sometimes cause dementia.
Are Parkinsons and Alzheimers related?
Although Parkinson's and Alzheimer's share some similar symptoms and risk factors, there does not appear to be a link between Parkinson's and Alzheimer's, nor any evidence that one can lead to the other.
Can you have Parkinson's and dementia?
Causes and risk factors Some studies have reported that the average time from onset of Parkinson's to developing dementia is about 10 years. One large study found that about three-quarters of people who live with Parkinson's for more than 10 years will develop dementia.
Do you have to code dementia with Alzheimer's?
Alzheimer's disease and dementia coding: Dementia is an inherent part of the diagnosis of Alzheimer's disease. The physician does not have to give both a diagnosis of Alzheimer's disease and dementia in order to report both codes. Per the ICD-10-CM Alphabetic Index, G30. 9 would be reported first, followed by F02.
Can dementia be used as primary diagnosis?
Unspecified dementia is determined to be a contributory condition to her terminal status, but cannot be listed as a principal diagnosis because it is listed on the 2014 List of Hospice Invalid Principal diagnosis Codes.
Can f01 51 be primary diagnosis?
The dysfunction may be primary, as in diseases, injuries, and insults that affect the brain directly and selectively; or secondary, as in systemic diseases and disorders that attack the brain only as one of the multiple organs or systems of the body that are involved.
What is g20 Parkinson's disease?
A progressive degenerative disorder of the central nervous system characterized by loss of dopamine producing neurons in the substantia nigra and the presence of lewy bodies in the substantia nigra and locus coeruleus.
How is Parkinson's disease?
Parkinson's disease is a brain disorder that causes unintended or uncontrollable movements, such as shaking, stiffness, and difficulty with balance and coordination. Symptoms usually begin gradually and worsen over time. As the disease progresses, people may have difficulty walking and talking.
What is Alzheimer's disease?
A disabling degenerative disease of the nervous system occurring in middle-aged or older persons and characterized by dementia and failure of memory for recent events, followed by total incapacitation and death. Types of the alzheimer syndrome are differentiated by the age of onset and genetic characteristics.
What are the symptoms of Alzheimer's?
A brain disorder that usually starts in late middle age or old age and gets worse over time. Symptoms include loss of memory, confusion, difficulty thinking, and changes in language, behavior, and personality.
What is neurodegenerative disorder?
Neurodegenerative disorder of the cns resulting in progressive loss of memory and intellectual functions; begins in the middle or later years; characterized by brain lesions such as neurofibrillary tangles and neuritic plaques.
What is the most common form of dementia in older people?
A progressive, neurodegenerative disease characterized by loss of function and death of nerve cells in several areas of the brain leading to loss of cognitive function such as memory and language. Alzheimer's disease (ad) is the most common form of dementia among older people.
How does Alzheimer's disease affect people?
Dementia is a brain disorder that seriously affects a person's ability to carry out daily activities . Ad begins slowly. It first involves the parts of the brain that control thought, memory and language. People with ad may have trouble remembering things that happened recently or names of people they know. A related problem, mild cognitive impairment (mci), causes more memory problems than normal for people of the same age. Many, but not all, people with mci will develop ad. In ad, over time, symptoms get worse. People may not recognize family members or have trouble speaking, reading or writing. They may forget how to brush their teeth or comb their hair. Later on, they may become anxious or aggressive, or wander away from home. Eventually, they need total care. This can cause great stress for family members who must care for them. Ad usually begins after age 60. The risk goes up as you get older. Your risk is also higher if a family member has had the disease. No treatment can stop the disease. However, some drugs may help keep symptoms from getting worse for a limited time. nih: national institute on aging
When will the ICD-10 G30.9 be released?
The 2022 edition of ICD-10-CM G30.9 became effective on October 1, 2021.
What are the symptoms of Parkinson's disease?
The early stages of PD include the following signs and symptoms: Slight shaking of a finger, hand, leg, chin, or lip. Stiffness or difficulty walking. Difficulty getting out of a chair.
What is the PD G20 code?
With PD G20 code, you will be coding associated signs and symptoms or those complications not necessarily inherent to the disease. Most of these complications will be found in Chapter 18, as signs and/or symptoms.
What are the symptoms of PD?
PD is associated with the physical symptoms of tremor and/or rigidity. These symptoms may be shown as head bobbing or other sudden involuntary jerking movements and shaking hand (s).
What is the third category of medication for PD?
The third category of drugs prescribed for PD includes medications that help control the non-motor symptoms of the disease ; that is, the symptoms that don't affect movement. For example, people with PD-related depression may be prescribed antidepressants.
What is the second category of PD drugs?
The second category of PD drugs affects other neurotransmitters in the body in order to ease some of the symptoms of the disease. For example, anticholinergic drugs interfere with production or uptake of the neurotransmitter acetylcholine. These can be effective in reducing tremors.
How many people are affected by Parkinson's disease?
As a neurodegenerative disease of the brain, which impacts an individual’s motor function, Parkinson’s Disease (PD) is the most common neurological disorder, affecting approximately one million people in the United Status. It is estimated that approximately 60,000 Americans are diagnosed with PD each year, and this number does not reflect ...
What are the most common drugs for PD?
The first category includes drugs that increase the level of dopamine in the brain. The most common drugs for PD are dopamine pre cursors—substances such as levodopa that cross the blood-brain barrier and are then changed into dopamine.
What is the ICd 10 code?
1 The codes comprising the ICD-10-CM are used to compile statistics, adjudicate coverage, calculate payment, and assess quality of care. 2 Codes are updated annually because inadequate coding can prevent accurate payment for services rendered and limit the evaluation of medical processes and outcomes. 2 We have assessed the need for additional ICD-10-CM codes for Parkinson disease (PD) to better reflect patient care.
What is the ICd 10 code for dystonia?
There is currently an ICD-10-CM code for dystonia (G24) and subcodes for different types of dystonia (G24.0–G24.9), as well as an ICD-10-CM code for drug-induced subacute dyskinesia (G24.01). These are not accurate to specify PD with dyskinesia, however. In PD, dyskinesia results from multiple mechanisms associated with disease progression, including glutamatergic overactivity, serotonin neuronal false transmitter release of dopamine, and loss of striatal buffering capacity. 14,23,24 In contrast, another unrelated movement disorder, tardive dyskinesia, is accurately coded by G24.01, 22 because this is caused by drug-induced dopamine receptor blocking mechanisms. 25
What are the challenges of coding for PD?
Some potential challenges may exist with expanding the ICD-10-CM coding structure for PD. The process of learning and entering new codes might be more time consuming for physicians until they adjust to the new proposed coding system. Under the current coding structure, however, health care providers need to accurately document patients’ symptoms to support the proper code. This could indirectly affect how physicians accurately address and manage PD symptoms, which might also impede physicians’ time. Therefore, including additional codes to specify motor complications associated with PD would be expected to facilitate the process for health care providers to accurately diagnose and code a patient with PD and “OFF” episodes and/or dyskinesia. Furthermore, expanding the ICD-10-CM coding for PD may reduce the time associated with providing clinical notes and additional documentation to justify both adjunctive and on-demand treatments for “OFF” episodes and dyskinesia for prior authorization. Another potential challenge is the possible learning curve associated with revising the coding structure for PD and more time spent on administrative tasks. However, the ICD-10-CM codes are updated on an annual basis and health care providers implement these changes with relative ease. Both potential limitations are expected to be outweighed by the benefits associated with revising the ICD-10-CM codes for PD (Figure 2).
What are the hallmarks of PD?
The pathologic hallmark of PD is the presence of Lewy bodies, which are intracellular inclusions of α-synuclein. 6,7 These α-synuclein protein aggregates are associated with the death of dopamine-producing neurons 4 and have been implicated in the progressive, neurodegenerative process underlying idiopathic PD. 8 Levodopa and other dopaminergic therapies replenish striatal dopamine and provide symptomatic benefit. 9 As neurodegeneration progresses over 3 to 5 years, however, progressive striatal denervation coupled with variable intestinal absorption of levodopa due to gastric dysmotility—reflecting enteric nervous system involvement—causes the emergence of motor complications, including motor fluctuations (ie, “OFF” episodes) and dyskinesia. 10
What is the ICD code for Alzheimer's?
ICD Code G30 is a non-billable code. To code a diagnosis of this type, you must use one of the four child codes of G30 that describes the diagnosis 'alzheimer's disease' in more detail. G30 Alzheimer's disease. NON-BILLABLE. BILLABLE.
What is the ICD code for neurodegeneration?
The ICD code G30 is used to code Neurodegeneration. Neurodegeneration is the umbrella term for the progressive loss of structure or function of neurons, including death of neurons.
What is the ICD code for acute care?
G30 . Non-Billable means the code is not sufficient justification for admission to an acute care hospital when used a principal diagnosis. Use a child code to capture more detail. ICD Code G30 is a non-billable code.
What are the parallels between neurodegenerative disorders?
There are many parallels between different neurodegenerative disorders including atypical protein assemblies as well as induced cell death. Neurodegeneration can be found in many different levels of neuronal circuitry ranging from molecular to systemic. Specialty:
What is the use of additional code?
Use Additional Code. Use Additional Code note means a second code must be used in conjunction with this code. Codes with this note are Etiology codes and must be followed by a Manifestation code or codes. Code to identify: Delirium, if applicable See Code F05.
Agenda
Coding for Alzheimer’s and Parkinson’s disease, stroke, epilepsy, migraines, and pain
Meet the Speaker
Lori-Lynne A. Webb, CPC, CCS-P, CCP, CHDA, CDIP, COBGC, AHIMA-approved ICD-10-CM/PCS trainer, is an E/M and procedure-based coding, compliance, data charge entry, and HIPAA privacy specialist with more than 20 years of experience.
Continuing Education
AAPC This program has the prior approval of AAPC for 1.5 continuing education hours. Granting of prior approval in no way constitutes endorsement by AAPC of the program content or the program sponsor.
Instructions
Webinar system requirements and program materials: To fully benefit from the webinar experience, please note you will need a computer equipped with the following:
Popular Posts:
- 1. icd 10 code for tearful
- 2. icd 9 code for seborrheic area of ear
- 3. icd 10 code for pressulre ulcer stage ii leg
- 4. what is the icd 10 code for myalgia
- 5. icd 10 code for chest pain with inspiration
- 6. icd 10 code for duchenne muscular dystrophy
- 7. icd 10 code for right breast mastectomy
- 8. icd 10 code for decreased rectal sphincter tone
- 9. icd 10 code for non small cell carcinoma of left lung invasion of pulmanary artery
- 10. icd 10 code for yeast infection diaper