What is antithrombin III deficiency?
Antithrombin III deficiency (abbreviated ATIII deficiency) is a deficiency of antithrombin III. It is a rare hereditary disorder that generally comes to light when a patient suffers recurrent venous thrombosis and pulmonary embolism, and repetitive intrauterine fetal death (IUFD).
What are the possible complications of antithrombin deficiency?
Antithrombin deficiency may result in serious venous thrombosis and heparin resistance. Please visit our Clinical Education Center to stay informed on any future publications, webinars, or other education opportunities.
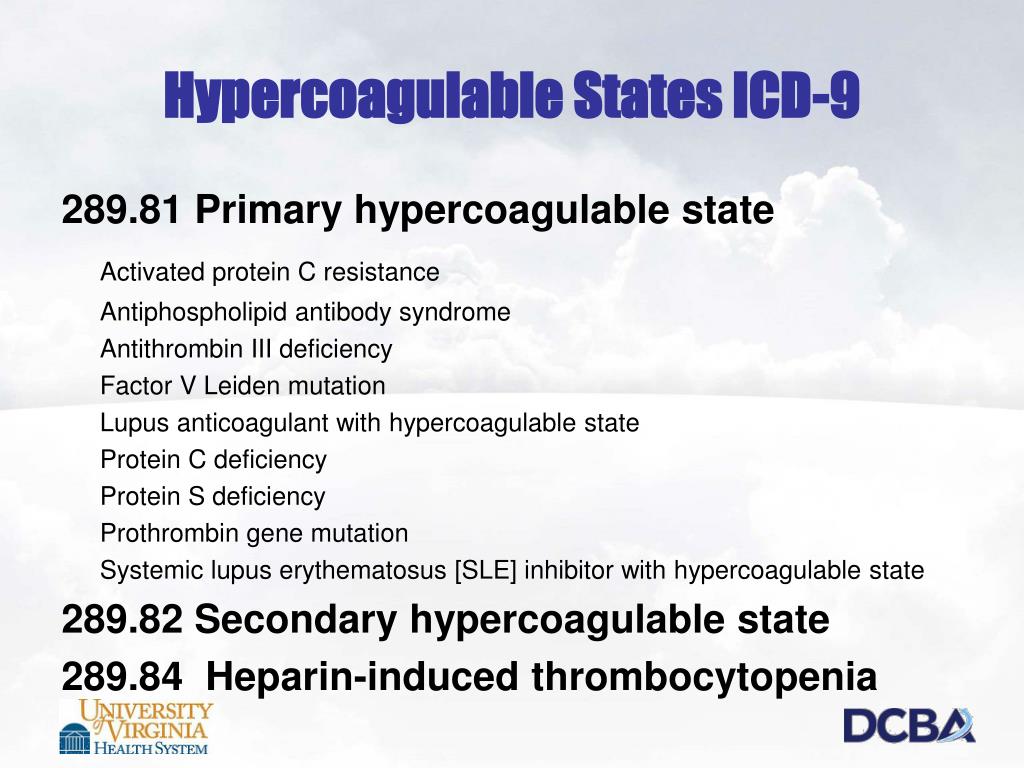
What is the ICD 10 code for primary thrombophilia?
Other primary thrombophilia. D68.59 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2020 edition of ICD-10-CM D68.59 became effective on October 1, 2019. This is the American ICD-10-CM version of D68.59 - other international versions of ICD-10 D68.59 may differ.
What is the ICD 10 code for thrombocytopenia?
This is the American ICD-10-CM version of D68.59 - other international versions of ICD-10 D68.59 may differ. A disorder of hemostasis in which there is a tendency for the occurrence of thrombosis. A rare disorder characterized by the presence of low levels of antithrombin iii which prohibits the formation of blood clots.

What is the ICD-10 code for antithrombin III?
The 2022 edition of ICD-10-CM D68. 59 became effective on October 1, 2021. This is the American ICD-10-CM version of D68.
What does low antithrombin III mean?
Antithrombin deficiency (or antithrombin III deficiency) is a blood clotting disorder that makes you more likely to get abnormal blood clots. People with this problem are at a high risk for deep vein thrombosis (a blood clot in any deep vein of the body) and pulmonary embolism (a clot that ends up in your lungs).
What is ICD-10 code for factor VII deficiency?
D68. 2 - Hereditary deficiency of other clotting factors. ICD-10-CM.
What ICD-10 code will cover factor v leiden mutation?
Factor v leiden mutation (r506q) is the most common cause of apc resistance. An abnormality that refers to mutation of factor v leiden, which is a variant of human factor v. It results in thrombophilia, deep vein thrombosis, and a slightly increased risk of miscarriage.
What is antithrombin deficiency?
Deficiency of antithrombin (AT; antithrombin III) can be inherited or acquired; it is defined as an AT activity level that is consistently less than 80 percent of normal (or the lower limit of the assay's reference range). In some patients, AT deficiency can be associated with an increased risk of thromboembolism.
Is antithrombin and antithrombin III the same?
It blocks our blood clotting mechanism by inactivating the major clotting protein “thrombin.” It is, therefore, called “anti-thrombin.” While antithrombin III was the original name given to this protein, the correct name now is just antithrombin, with the “III” dropped.
What is the ICD-10 code for Factor V?
Hereditary deficiency of other clotting factors The 2022 edition of ICD-10-CM D68. 2 became effective on October 1, 2021. This is the American ICD-10-CM version of D68.
What does it mean when Factor 8 is high?
If your levels of factor VIII are too high, you are likely at a higher risk for thrombosis, which is blood clot formation in your blood vessels. In this case, your doctor may perform additional tests or prescribe anticoagulant therapy.
What is acquired coagulation deficiency?
Acquired factor VIII deficiency is a bleeding disorder that requires prompt diagnosis and management to avert severe, life-threatening bleeding and death. Despite knowledge of this disorder of coagulation for several decades, relatively little is still known about this disease because of its rare incidence.
What ICD-10 covers PT PTT?
NCD - Partial ThromboplastinTime (PTT) (190.16)
What is factor V Leiden heterozygous?
Heterozygous means that the 2 copies of a gene are different. In your case, one of your Factor V gene codes is for normal clotting Factor V and the other Factor V gene code is for Factor V Leiden. There is more risk of a blood clot if both gene codes are for Factor V Leiden (ie in the homozygous state).
What diagnosis covers CPT 85610?
A: When physicians use a prothrombin time test (reported with CPT code 85610) to monitor patients on anticoagulant drugs, Medicare pays the entity that performed the test. Its payment for the test is based on the geographically specific laboratory test fee schedule.
The ICD code D688 is used to code Antithrombin III deficiency
Antithrombin III deficiency (abbreviated ATIII deficiency) is a deficiency of antithrombin III. It is a rare hereditary disorder that generally comes to light when a patient suffers recurrent venous thrombosis and pulmonary embolism, and repetitive intrauterine fetal death (IUFD).
Coding Notes for D68.8 Info for medical coders on how to properly use this ICD-10 code
Type-1 Excludes mean the conditions excluded are mutually exclusive and should never be coded together. Excludes 1 means "do not code here."
ICD-10-CM Alphabetical Index References for 'D68.8 - Other specified coagulation defects'
The ICD-10-CM Alphabetical Index links the below-listed medical terms to the ICD code D68.8. Click on any term below to browse the alphabetical index.
Equivalent ICD-9 Code GENERAL EQUIVALENCE MAPPINGS (GEM)
This is the official approximate match mapping between ICD9 and ICD10, as provided by the General Equivalency mapping crosswalk. This means that while there is no exact mapping between this ICD10 code D68.8 and a single ICD9 code, 286.9 is an approximate match for comparison and conversion purposes.
What is the role of antithrombin in hemostasis?
In this way, AT serves an important role in controlling coagulation by limiting the extent of thrombus formation. AT inhibits several steps of the coagulation cascade by binding to the catalytic sites of thrombin (factor IIa) and factors IXa, Xa, XIa, and XIIa. The complexes of AT with these thrombogenic serine proteinases are then rapidly cleared from the plasma. The binding of AT to these coagulation factors is slow in the absence of heparin. Heparin sulfate from endothelial cells or exogenously administered heparin binds to a specific site on the AT molecule. This produces a conformational change in the structure of AT, enhancing its binding to the activated coagulation factors by 1000-fold. 8 Congenital defects in both the heparin binding site and the proteinase binding site of AT can cause functional deficiencies in AT activity.
What causes low AT levels?
AT deficiency can be found in patients with severe hepatic disorders (hepatitis, cirrhosis, etc) due to diminished synthesis and nephrotic syndrome due to urinary protein loss. Malignancy and inflammatory bowel disease can also produce diminished AT levels. 9 Drug therapy with L-asparaginase or fluorouracil can also reduce AT levels.
Can thrombosis be caused by surgery?
In the majority of cases, thrombosis can be linked to trauma , surgery, pregnancy, oral contraceptive use, or other risk factors; however, thrombosis occurs spontaneously with no precipitating events or other known risk factors in about 33% of cases. 8.
Clinical Significance
Antithrombin III Activity and Antigen - This assay is used to assess the availability of antithrombin, a potent, naturally occurring anticoagulant, by measuring total protein (antigen) and activity. Antithrombin deficiency may result in serious venous thrombosis and heparin resistance.
Test Resources
Please visit our Clinical Education Center to stay informed on any future publications, webinars, or other education opportunities.
Test Details
Patient should abstain from anabolic steroids, Gemfibrozil, Warfarin (Coumadin®), heparin therapy, asparaginase, estrogens, gestodene and oral contraceptives optimally for 3 days prior to specimen collection. Overnight fasting is preferred.
Popular Posts:
- 1. icd-10-cm code for blighted ovum
- 2. icd 10 external cause code for repetitve fracture
- 3. icd 10 code for personal history of unterine cancer
- 4. icd 10 code for personal history of brain aneurysm
- 5. icd 10 code for ocular hypertension bilateral
- 6. icd 10 code for fracture of distal end of right tibia
- 7. icd 10 code for hiv disease
- 8. icd 10 cm code for p 82.90
- 9. icd 10 code for catarct
- 10. icd 10 code for stone in cystic or bile duct