What is the diagnostic code for anxiety?
Oct 01, 2021 · Encounter for screening examination for other mental health and behavioral disorders 2019 (effective 10/1/2018): New code 2020 (effective 10/1/2019): No change 2021 (effective 10/1/2020): No change 2022 (effective 10/1/2021): No change
What is the ICD 10 code for early onset dementia?
Oct 01, 2021 · Encounter for screening for depression Z13.31 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM Z13.31 became effective on October 1, 2021. This is the American ICD-10-CM …
What is the ICD 10 diagnosis code for?
anxiety coding fact sheet for primary care clinicians 96102 Psychological testing (includes psychodiagnostic assessment of emotionality, intellectual abilities,
What does ICD 10 do you use for EKG screening?
ICD-10 code Z13.39, “Encounter for screening examination for other mental health and behavioral disorders,” can be reported with CPT code 96127 when anxiety assessments are given to ...
What is the ICD-10 code for screening?
What is the difference between 96127 and 96160?
What is the ICD-10 code for psychological assessment?
What is the ICD-10 code for anxiety about health?
When do you use CPT code 96160?
Is 99420 a valid CPT code?
What is the ICD-10 code for depression screening?
What is R41 89?
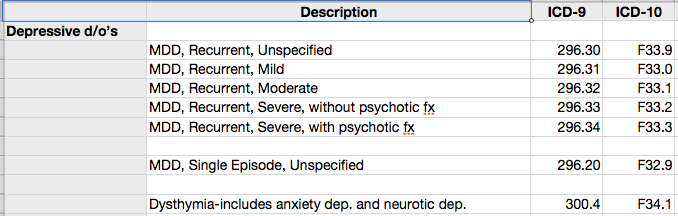
What is the ICD-10 code for depression?
As stated above, F32. 9 describes major depressive disorder, single episode, unspecified.Jun 4, 2021
What is the diagnosis for anxiety?
What is the ICD-10 code for mild anxiety?
What is the DSM code for anxiety?
How does coding and billing help in the medical home?
Coding and billing for screening performed in the medical home can help cover the costs of the work done and the instruments used to monitor for developmental delays, maternal depression, risky substance use, suicidality, or mental health disorders. Screening reimbursement is complicated because state and private insurers may differ on how many screens may be reimbursed during 1 visit or in 1 year. Some payers contract with participating providers to bundle developmental or mental health screening with preventive care, or they may direct their providers to bill differently from the American Medical Association's CPT guidelines. Detailed coding and billing, even if it does not get paid by Medicaid or the insurer, is useful to track work value (RVU).
What is the difference between modifier 25 and modifier 59?
There is no need to use Modifier 25 for routine screening in a well-child visit. Modifier 59 indicates a distinct procedural service (non-E/M service).
Why is accurate coding important?
Accurate, detailed coding, even for items not currently reimbursable, helps reflect the actual clinical effort and identify codes that may need to be reimbursable in the future to optimize care for children with special health care needs.
What is modifier 25?
Modifier 25 appends one service with a second, separately identifiable E/M service. Modifier 25 states that the procedure performed should be considered separate from the visit. There is no need to use Modifier 25 for routine screening in a well-child visit.
What is a CRAFFT 2.1?
During a well-child visit for an established 17-year-old, the patient completes a PHQ-9 and a CRAFFT 2.1, both of which are normal. The adolescent reports feeling anxious in crowds and talking in front of the class at school. In addition to the routine depression and risky substance use screeners completed at check-in, the patient also completes a SCARED Version for Child (anxiety screen), which is abnormal. The provider briefly discusses the results with the patient and then recommends a follow-up visit focused on anxiety.
What is an 18-month-old child's E/M?
An established 18-month-old patient presents for an E/M visit for an ear infection requiring treatment. During the visit, the provider realizes that the 18-month-old child missed his last well-child check and administers a developmental screen and an autism screen. The clinician reviews the results with the family.
What happens during an 18 month visit?
During an 18-month, well-child visit, the parent completes an autism screen and a developmental screen. The clinician reviews the results of both screens with the family and documents them appropriately in the visit note. The child also has an ear infection requiring treatment.
What is a screening test?
Also called: Screening tests. Screenings are tests that look for diseases before you have symptoms. Screening tests can find diseases early, when they're easier to treat. You can get some screenings in your doctor's office. Others need special equipment, so you may need to go to a different office or clinic.
What is the Z13.39 code?
Z13.39 is a billable diagnosis code used to specify a medical diagnosis of encounter for screening examination for other mental health and behavioral disorders. The code Z13.39 is valid during the fiscal year 2021 from October 01, 2020 through September 30, 2021 for the submission of HIPAA-covered transactions. The code is exempt from present on admission (POA) reporting for inpatient admissions to general acute care hospitals.#N#The code Z13.39 describes a circumstance which influences the patient's health status but not a current illness or injury. The code is unacceptable as a principal diagnosis.
Is Z13.39 a POA?
Z13.39 is exempt from POA reporting - The Present on Admission (POA) indicator is used for diagnosis codes included in claims involving inpatient admissions to general acute care hospitals. POA indicators must be reported to CMS on each claim to facilitate the grouping of diagnoses codes into the proper Diagnostic Related Groups (DRG). CMS publishes a listing of specific diagnosis codes that are exempt from the POA reporting requirement. Review other POA exempt codes here.
How does mental health affect people?
Mental health includes our emotional, psychological, and social well-being. It affects how we think, feel, and act as we cope with life. It also helps determine how we handle stress, relate to others, and make choices. Mental health is important at every stage of life, from childhood and adolescence through adulthood.
What is a screening test?
Also called: Screening tests. Screenings are tests that look for diseases before you have symptoms. Screening tests can find diseases early, when they're easier to treat. You can get some screenings in your doctor's office. Others need special equipment, so you may need to go to a different office or clinic.
What is the medical term for depression?
Depression. Also called: Clinical depression, Dysthymic disorder, Major depressive disorder, Unipolar depression. Depression is a serious medical illness. It's more than just a feeling of being sad or "blue" for a few days.
What is the Z13.31 code?
Z13.31 is a billable diagnosis code used to specify a medical diagnosis of encounter for screening for depression. The code Z13.31 is valid during the fiscal year 2021 from October 01, 2020 through September 30, 2021 for the submission of HIPAA-covered transactions. The code is exempt from present on admission (POA) reporting for inpatient admissions to general acute care hospitals.#N#The code Z13.31 describes a circumstance which influences the patient's health status but not a current illness or injury. The code is unacceptable as a principal diagnosis.
What is the tabular list of diseases and injuries?
The Tabular List of Diseases and Injuries is a list of ICD-10 codes, organized "head to toe" into chapters and sections with coding notes and guidance for inclusions, exclusions, descriptions and more. The following references are applicable to the code Z13.31:
Is Z13.31 a POA?
Z13.31 is exempt from POA reporting - The Present on Admission (POA) indicator is used for diagnosis codes included in claims involving inpatient admissions to general acute care hospitals. POA indicators must be reported to CMS on each claim to facilitate the grouping of diagnoses codes into the proper Diagnostic Related Groups (DRG). CMS publishes a listing of specific diagnosis codes that are exempt from the POA reporting requirement. Review other POA exempt codes here.
What is depression medical?
Depression. Also called: Clinical depression, Dysthymic disorder, Major depressive disorder, Unipolar depression. Depression is a serious medical illness. It's more than just a feeling of being sad or "blue" for a few days.
Is depression a medical condition?
Depression is a serious medical illness. It's more than just a feeling of being sad or "blue" for a few days. If you are one of the more than 19 million teens and adults in the United States who have depression, the feelings do not go away. They persist and interfere with your everyday life.

Popular Posts:
- 1. icd 10 code for unintentional overdose
- 2. icd-10 code for supervision of pregnancy with history of miscarriage
- 3. icd 10 code for perianal mass
- 4. icd 10 code for chronic alternating diarrhea with constipation
- 5. icd 10 cm code for dyshidrotic eczema.
- 6. icd 10 code for vental hernia
- 7. icd 10 code for cervical bone spur
- 8. icd 10 code for pain in joints of right hand
- 9. icd 10 code for raynauds
- 10. icd 10 code for lumbar decompression