What is the code for fovea?
Why use a diagnosis code in the absence of an approved therapy?
What is H35.31x3?
What is central geographic atrophy?
What is the code for AMD wet?
What is GA in a patient?
See 3 more
About this website
Coding For Laterality in AMD
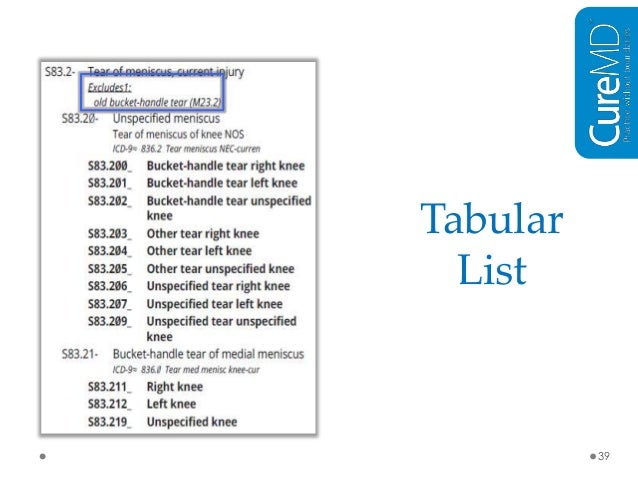
When you use the codes for dry AMD (H35.31xx) and wet AMD (H35.32xx), you must use the sixth character to indicate laterality as follows:1 for the...
Coding For Staging in Dry AMD
The codes for dry AMD—H35.31xx—use the seventh character to indicate staging as follows:H35.31x1 for early dry AMD—a combination of multiple small...
Defining Geographic Atrophy
When is the retina considered atrophic? The Academy Preferred Practice Pattern1 defines GA as follows:The phenotype of central geographic atrophy,...
Coding For Geographic Atrophy
The Academy recommends that when coding, you indicate whether the GA involves the center of the fovea: Code H35.31x4 if it does and H35.31x3 if it...
Coding For Staging in Wet AMD
The codes for wet AMD—H35.32xx—use the sixth character to indicate laterality and the seventh character to indicate staging as follows:H35.32x1 for...
How to Use the ICD-10 Codes for Age-Related Macular Degeneration
62 • SEPTEMBER 2017 Coding for Geographic Atrophy The Academy recommends that when coding, you indicate whether the GA involves the center of the fovea: Code H35.31x4 if it does and H35.31x3 if it
ICD10 codes matching 'Macular Degeneration' - ICD-Codes.com
ICD10 codes matching "Macular Degeneration" Codes: = Billable H35.30 Unspecified macular degeneration; H35.31 Nonexudative age-related macular degeneration; H35.311 Nonexudative age-related macular degeneration, right eye; H35.3110 Nonexudative age-related macular degeneration, right eye, stage unspecified; H35.3111 Nonexudative age-related macular degeneration, right eye, early dry stage
Neovascular ARMD icd 10 | Medical Billing and Coding Forum - AAPC
If this is your first visit, be sure to check out the FAQ & read the forum rules.To view all forums, post or create a new thread, you must be an AAPC Member.If you are a member and have already registered for member area and forum access, you can log in by clicking here.If you've forgotten your username or password use our password reminder tool.
What is the code for fovea?
The Academy recommends that when coding, you indicate whether the GA involves the center of the fovea: Code H35.31x4 if it does and H35.31x3 if it doesn’t, with “x” indicating lateral ity. Improved categorization of GA will help in clinical practice and also will lead to a better understanding of the natural history, comorbidities, and visual prognosis associated with the disease.
Why use a diagnosis code in the absence of an approved therapy?
Why use a diagnosis code in the absence of an approved therapy? Accurate documentation and coding will help researchers and policymakers track the visual impairment and visual function deficits that are associated with the condition. Furthermore, when treatments do become available, you will be ready to code for them.
What is H35.31x3?
H35.31x3 for advanced atrophic dry AMD without subfoveal involvement —geographic atrophy (GA) not involving the center of the fovea.
What is central geographic atrophy?
The phenotype of central geographic atrophy, the advanced form of non-neovascular AMD, will have 1 or more zones of well- demarcated RPE and/or choriocapillaris atrophy. Drusen and other pigmentary abnormalities may surround the atrophic areas.
What is the code for AMD wet?
The codes for wet AMD—H35.32xx—use the sixth character to indicate laterality and the seventh character to indicate staging as follows:
What is GA in a patient?
These patches enlarge and coalesce and may be associated with a dense paracentral scotoma, thereby limiting tasks such as reading. Patients with GA may demonstrate good visual acuity (VA) until late in the course of the disease, when the fovea becomes progressively atrophic, leading to severe visual acuity decline from central blindness and forcing the patient to use noncentral retina and eccentric fixation to read and perform other visual tasks.
What is the ICd code for postmenopausal vaginal atrophic vaginal?
N95.2 is a billable ICD code used to specify a diagnosis of postmenopausal atrophic vaginitis. A 'billable code' is detailed enough to be used to specify a medical diagnosis.
What is atrophic vaginal atrophy?
atrophic vaginitis (also known as vaginal atrophy or urogenital atrophy) is an inflammation of the vagina (and the outer urinary tract) due to the thinning and shrinking of the tissues, as well as decreased lubrication. these symptoms are due to a lack of the reproductive hormone estrogen. Specialty:
What is DRG #742-743?
DRG Group #742-743 - Uterine and adnexa procedure for non-malignancy without CC or MCC.
ICD-10 Codes for Cerebrovascular Accident (CVA)
Cerebrovascular accident (also known as CVA) is the medical term for a stroke. A stroke occurs when the blood supply to part of your brain is interrupted or reduced, preventing brain tissue from getting oxygen and nutrients. Brain cells begin to die in minutes.
Symptoms of CVA
The quicker you can get a diagnosis and treatment for a stroke, the better your prognosis will be. For this reason, it’s important to understand and recognize the symptoms of a stroke.
Treatment for CVA
Emergency treatment for stroke depends on whether you’re having an ischemic stroke or a stroke that involves bleeding into the brain. To treat an ischemic stroke, doctors must quickly restore blood flow to your brain.
What is the code for fovea?
The Academy recommends that when coding, you indicate whether the GA involves the center of the fovea: Code H35.31x4 if it does and H35.31x3 if it doesn’t, with “x” indicating lateral ity. Improved categorization of GA will help in clinical practice and also will lead to a better understanding of the natural history, comorbidities, and visual prognosis associated with the disease.
Why use a diagnosis code in the absence of an approved therapy?
Why use a diagnosis code in the absence of an approved therapy? Accurate documentation and coding will help researchers and policymakers track the visual impairment and visual function deficits that are associated with the condition. Furthermore, when treatments do become available, you will be ready to code for them.
What is H35.31x3?
H35.31x3 for advanced atrophic dry AMD without subfoveal involvement —geographic atrophy (GA) not involving the center of the fovea.
What is central geographic atrophy?
The phenotype of central geographic atrophy, the advanced form of non-neovascular AMD, will have 1 or more zones of well- demarcated RPE and/or choriocapillaris atrophy. Drusen and other pigmentary abnormalities may surround the atrophic areas.
What is the code for AMD wet?
The codes for wet AMD—H35.32xx—use the sixth character to indicate laterality and the seventh character to indicate staging as follows:
What is GA in a patient?
These patches enlarge and coalesce and may be associated with a dense paracentral scotoma, thereby limiting tasks such as reading. Patients with GA may demonstrate good visual acuity (VA) until late in the course of the disease, when the fovea becomes progressively atrophic, leading to severe visual acuity decline from central blindness and forcing the patient to use noncentral retina and eccentric fixation to read and perform other visual tasks.
Popular Posts:
- 1. icd 10 code for chronic embolism axillary
- 2. icd 10 code for generalized back pain
- 3. icd-10-cm code for pyelonephritis
- 4. icd 10 code for right upper lobe infiltrate
- 5. icd 10 cm code for history of diabetes
- 6. icd 10 code for asthma exacerbarion with copd
- 7. icd 10 code for transitional care following surgery
- 8. icd 10 code for traumatic hemothorax on left
- 9. icd 10 code for metatarsalgia right foot
- 10. icd 10 code for distress