What is bilateral foot condition?
- You experience tenderness
- There is marked inward displacement and pronation (inward rolling of the foot)
- Orthopedic shoes and inserts do not provide relief or reduce the symptoms
- Your Achilles tendon spasms when it is touched
What is debridement of foot ulcer?
Preparation may include:
- physical exam
- measurement of wound
- pain medication (mechanical debridement)
- local or general anesthesia (sharp debridement)
What is bilateral foot?
Bilateral club foot is when both feet turn inward and downward. It is a condition that is present at birth (congenital). Common symptoms reported by people with bilateral club foot
What is the best treatment for a diabetic foot ulcer?
There are several key factors in the appropriate treatment of a diabetic foot ulcer:
- Prevention of infection
- Taking the pressure off the area, called “off-loading”
- Removing dead skin and tissue, called “debridement”
- Applying medication or dressings to the ulcer
- Managing blood glucose and other health problems
What is the ICD-10 diagnosis code for right foot ulcer?
519 for Non-pressure chronic ulcer of other part of right foot with unspecified severity is a medical classification as listed by WHO under the range - Diseases of the skin and subcutaneous tissue .
What is the ICD-10 code for unspecified foot ulcer?
ICD-10-CM Code for Non-pressure chronic ulcer of other part of unspecified foot with unspecified severity L97. 509.
How do you code a foot ulcer?
Of these options, the most commonly used codes for diabetic foot ulcers are E10. 621 (Type 1 diabetes mellitus with foot ulcer) and E11. 621 (Type 2 diabetes mellitus with foot ulcer).
What is the ICD-10 for diabetic foot ulcer?
ICD-10 code E11. 621 for Type 2 diabetes mellitus with foot ulcer is a medical classification as listed by WHO under the range - Endocrine, nutritional and metabolic diseases .
What is the ICD 10 code for left foot ulcer?
ICD-10-CM Code for Non-pressure chronic ulcer of other part of left foot with unspecified severity L97. 529.
What is the ICD 10 code for foot care?
Routine foot care, removal and/or trimming of corns, calluses and/or nails, and preventive maintenance in specific medical conditions (procedure code S0390), is considered a non-covered service.
Whats the difference between a pressure ulcer and a diabetic ulcer?
While diabetic patients can get pressure ulcers due to abuse or neglect in a nursing home, diabetic ulcers may appear in areas that are not typically subject to extended pressure—such as the bottoms of the feet when a resident has been lying down. In these cases, a diagnosis of a diabetic ulcer is more apt.
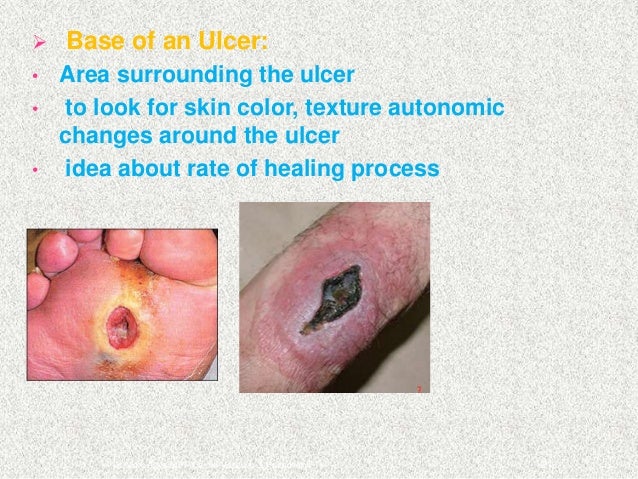
What is an ulcer on the foot?
Foot ulcers are open sores or lesions that will not heal or that return over a long period of time. These sores result from the breakdown of the skin and tissues of the feet and ankles and can get infected. Symptoms of foot ulcers can include swelling, burning, and pain.
When coding a pressure ulcer what must be coded?
“Two codes are needed to completely describe a pressure ulcer: A code from subcategory 707.0, Pressure ulcer, to identify the site of the pressure ulcer and a code from subcategory 707.2, Pressure ulcer stages.
What is the ICD 10 code for diabetic foot ulcer left foot?
529: Non-pressure chronic ulcer of other part of left foot with unspecified severity.
What is the ICD 10 code for diabetic foot infection?
Type 2 diabetes mellitus with foot ulcer E11. 621 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
What is ICD 10 code for diabetic wound infection?
Type 2 diabetes mellitus with other skin ulcer The 2022 edition of ICD-10-CM E11. 622 became effective on October 1, 2021.
What is a L97.91 ulcer?
L97.91 -Non-pressure chronic ulcer of unspecified part of right lower leg. L97.92 – Non-pressure chronic ulcer of unspecified part of left lower leg. According to the American Podiatric Medical Association, about 14 to 24 percent of Americans with diabetic foot ulcers have amputations.
What are the risk factors for ulcers?
The most common risk factors for ulcer formation include – diabetic neuropathy, structural foot deformity, kidney disease, obesity and peripheral arterial occlusive disease. The condition can be effectively prevented if the underlying conditions causing it are diagnosed early and treated correctly.
What is a diabetic foot ulcer?
Regarded as the most common reason for hospital stays among people with diabetes, a diabetic foot ulcer (DFU) is an open sore caused by neuropathic (nerve) and vascular (blood vessel) complications of the disease. Typically located on the plantar surface, or bottom/top of toes, pad of foot, or heel of foot, these complex, ...
What is the best way to offload wounds on the forefoot?
Half shoes, therapeutic shoes, custom insoles, and the use of felted foam are other alternative methods to off-load wounds located on the forefoot. Dressings– Wounds and ulcers heal faster and have a lower risk of infection if they are kept covered and moist, using dressings and topically-applied medications.
How are cannabinoids separated?
Cannabinoids are separated from hemp using supercritical CO2 extraction. Thanks to modern-day innovation, the resulting solution is tidy, devoid of unneeded waxes and heavy metals, naturally present in the plant, and the sucked liquid has a common, oily consistency.
Why is it important to remove dead skin?
This procedure is important because dead skin hampers the development of healthy new tissues, and also makes the affected area more vulnerable to infections. Removal of the dead skin will promote quick and easy healing. Debridement will be done surgically, enzymatically, biologically, or through autolysis.
How many amputations are there for diabetics?
The risk of foot ulceration and limb amputations increases with age and duration of diabetes. In the United States, about 82,000 amputations are performed each year on persons with diabetes; half of those ages 65 years or older. Treatment for diabetic foot ulcers varies depending on their causes.
What percentage of diabetics have neuropathy?
After 10 years, ~90 percent of Type 1 and Type 2 diabetics have some degree of neuropathy, most commonly affecting the feet and legs, and 90 percent of diabetic foot ulcers have diabetic neuropathy as a contributing factor. If the diabetic doesn’t recognize discomfort due to nerve impairment, they may not adjust their shoes ...
What causes diabetic foot ulcers?
A “diabetic foot ulcer,” which is caused exclusively by hyperglycemia, in the absence of neuropathy or ischemia, is a rarity. That term almost always refers to an ulcer on the foot of a diabetic that derives from neuro/ischemic etiology, as opposed to being strictly and principally due to pressure injury.
What happens when blood sugar is low?
Poorly controlled blood sugars weaken the small blood vessel walls and predispose patients to arteriosclerosis. This impairs the circulation and causes ischemia of the soft tissues, especially of the lower extremities. Many diabetics have both diabetic peripheral neuropathy and angiopathy.
Why do diabetics get ulcers?
The American Podiatric Medical Association adds that “ (diabetic foot) ulcers form due to a combination of factors , such as lack of feeling in the foot, poor circulation, foot deformities, irritation (such as friction or pressure), and trauma, as well as duration of diabetes .”. They go on to note that “vascular disease can complicate a foot ulcer, ...
What is the L89 code for a pressure ulcer?
Pressure injuries with skin breakdown are considered pressure ulcers. An additional L89 code specifies the stage (depth of tissue injury) and the anatomical site. Pressure ulcers form in sites that experience shear or pressure, typically in tissue overlying bony prominences such as elbows, the sacrum, hips, or heels.
Why are pressure ulcers considered a patient safety indicator?
Pressure ulcers are deemed patient safety indicators and hospital acquired conditions because a concerted program for prevention and treatment can prevent them and protect our patients from iatrogenic harm. The diagnosis of a “pressure ulcer” may trigger prevalence and incident reporting.
What is the most common site of ulceration?
The plantar surface is the most common site of ulceration, especially at areas of bony prominence.”.
What is a venous ulcer?
Venous ulcers (venous insufficiency ulceration, stasis ulcers, stasis dermatitis, varicose ulcers, or ulcus cruris) are wounds that are thought to occur due to improper functioning of venous valves, usually of the leg s (hence leg ulcers).:846 . They are the major occurrence of chronic wounds, occurring in 70% to 90% of leg ulcer cases.
Where do ulcers on the right leg occur?
Venous ulcers develop mostly along the medial distal leg, and can be very painful. Venous ulcer on the back of the right leg.
Terminology
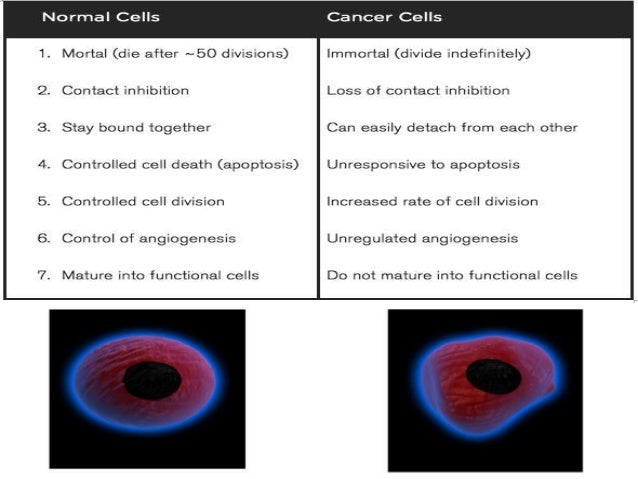
Diagnosis
- There are medical diagnoses that predispose patients to develop secondary conditions. Diabetes mellitus is a pervasive endocrinopathy whereby hyperglycemia affects every organ and system in the body, including the nerves and blood vessels. It makes a patient more prone to infection and poor healing. Diabetics are prone to foot ulcers, often with contributions from neuropathic, ische…
Clinical significance
- Diabetics also often have diseases of both large and small arteries. Poorly controlled blood sugars weaken the small blood vessel walls and predispose patients to arteriosclerosis. This impairs the circulation and causes ischemia of the soft tissues, especially of the lower extremities.
Causes
- Heel ulcers, however, are usually a consequence of a pressure injury, although it is also possible to have another mechanism cause a non-pressure injury involving the heel. Diabetes may accelerate or complicate the injury. The American Podiatric Medical Association adds that (diabetic foot) ulcers form due to a combination of factors, such as lack of feeling in the foot, po…
Signs and symptoms
- Neuropathy results in malum perforans pedis (a.k.a. bad perforating foot) ulcers. These are painless, non-necrotic, circular lesions circumscribed by hyperkeratosis. They often overlie a metatarsal head. Ischemic wounds manifest local signs of ischemia such as thin, shiny, hairless skin with pallor and coldness. These are often found at areas of friction and may be painful.
Epidemiology
- The American Orthopaedic Foot & Ankle Society states that ulceration is an extremely common complication in diabetic patients (up to 12 percent of the population). The plantar surface is the most common site of ulceration, especially at areas of bony prominence. The Society also points out that the presence of neuropathy is the key factor in development of diabetic ulceration.
Society and culture
- In the podiatric literature, NPUAP is often referenced as having given guidance to use diabetic foot ulcer for any ulcer on the foot of a diabetic, even if arterial disease and/or pressure played a role in its development. I think this is simplistic and derived from literature not aimed at physicians/APPs. It is common in the literature to see the term diabetic foot ulcer used for all-co…
Treatment
- Ultimately, the clinical concern is to treat the lesion appropriately, regardless of the name attached to it. The treatment for both pressure ulcers and diabetic foot ulcers includes offloading (i.e., pressure mitigation, often by means of padding, shoe modifications, contact casts, boots, or non-weight-bearing strategies). Any non-healing wound should be assessed for neuropathy and …
Popular Posts:
- 1. icd 10 code for left eye glaucoma post surgery
- 2. icd pcs code for amniotomy
- 3. icd 10 code for cyst on scalp
- 4. icd 10 code for hyperglycemic hyperosmolar state
- 5. icd-11 code for diabetes mellitus
- 6. icd 10 code for film copies
- 7. icd 10 cm code for enlarged abdominal growth
- 8. icd 10 code for fibrocystic disease of right breast
- 9. icd 10 dx code for creatine kinase
- 10. icd 10 code for diabetic mycotic nails