What are the new ICD 10 codes?
The new codes are for describing the infusion of tixagevimab and cilgavimab monoclonal antibody (code XW023X7), and the infusion of other new technology monoclonal antibody (code XW023Y7).
What is difference between ICD9 and ICD10?
- Similar to the diagnosis code set, the alpha characters in ICD 10 code sets are not case-sensitive.
- The letters “O” and “I” are not in the code set. ...
- The 7 characters in the procedure code set help in providing very precise details. ...
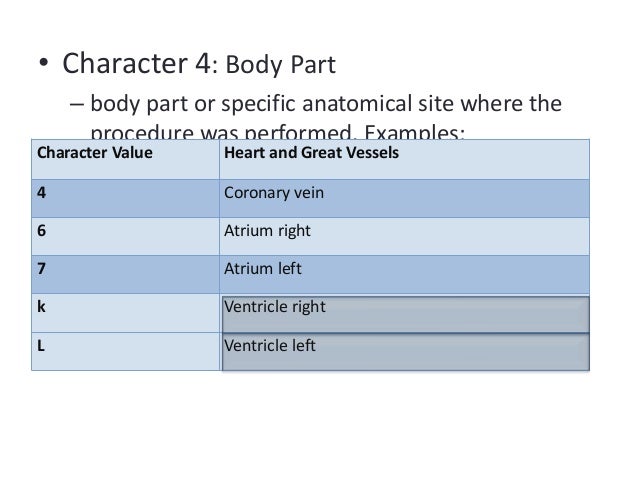
- The fourth character identifies the part of the body. ...
What does ICD 10 mean?
ICD-10 is the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD), a medical classification list by the World Health Organization (WHO). It contains codes for diseases, signs and symptoms, abnormal findings, complaints, social circumstances, and external causes of injury or diseases.
Where can one find ICD 10 diagnosis codes?
Search the full ICD-10 catalog by:
- Code
- Code Descriptions
- Clinical Terms or Synonyms
What is the ICD-10 code for ICD placement?
Z95.810Z95. 810 - Presence of automatic (implantable) cardiac defibrillator. ICD-10-CM.
What is ICD-10 code for implantable cardioverter defibrillator?
Encounter for adjustment and management of automatic implantable cardiac defibrillator. Z45. 02 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM Z45.
What is the ICD-10-CM code for pacemaker?
Z95.0ICD-10 code Z95. 0 for Presence of cardiac pacemaker is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
What is the ICD-10 code for presence of dual chamber pacemaker?
Z95.0Z95. 0 - Presence of cardiac pacemaker. ICD-10-CM.
What is the ICD 10 code for defibrillator shock?
Shock, not elsewhere classified ICD-10-CM R57. 0 is grouped within Diagnostic Related Group(s) (MS-DRG v39.0): 222 Cardiac defibrillator implant with cardiac catheterization with ami, hf or shock with mcc.
What is the ICD 10 code for nonischemic cardiomyopathy?
0 - Dilated cardiomyopathy is a sample topic from the ICD-10-CM. To view other topics, please log in or purchase a subscription. ICD-10-CM 2022 Coding Guide™ from Unbound Medicine.
What is the ICD-10 code for cardiac arrhythmia?
ICD-10 code I49. 9 for Cardiac arrhythmia, unspecified is a medical classification as listed by WHO under the range - Diseases of the circulatory system .
What is the ICD 10 code for pacemaker placement?
0JH606ZInsertion of Pacemaker, Dual Chamber into Chest Subcutaneous Tissue and Fascia, Open Approach. ICD-10-PCS 0JH606Z is a specific/billable code that can be used to indicate a procedure.
What is a biventricular pacemaker?
Biventricular Pacemaker and ICD (Biventricular ICD) You have a condition called heart failure. It is also known as congestive heart failure (CHF). This condition causes symptoms such as getting tired very quickly and being short of breath. To help treat these symptoms, your healthcare provider is recommending a biventricular pacemaker ...
What does the ICD part of a heart monitor do?
The ICD part of the device detects dangerously fast heart rhythms and stops them. If the device detects an abnormally fast heartbeat that can cause cardiac arrest, it will send a "shock" to the heart. The shock stops this dangerous heart rhythm and restores a normal heartbeat.
What are the 4 chambers of the heart?
The heart is made up of 4 sections (chambers) that pump to move blood through the heart. The top 2 chambers are the left atrium and right atrium. These are filling chambers of the heart. The bottom chambers are the left ventricle and right ventricle. These are the pumping chambers of the heart. The heart has an electrical system. This system sends signals that make the atria and ventricles work together. This causes the heart to beat and move blood through the heart and lungs and out to the body.
What is bundle branch block?
A bundle branch block can throw off the timing of the heart's contraction. This can make the heart's squeezing contraction even weaker. A biventricular pacemaker and ICD help keep the heart pumping in a more normal way. The pacemaker device keeps the heart from beating too slowly. It tries to restore the normal squeezing pattern of the heart.
Where is the biventricular pacemaker implanted?
The biventricular pacemaker is implanted in the muscle tissue of the chest, below the collarbone, or in the abdomen. Three leads or wires, one atrial lead [right atrium] and two ventricular leads [right and left ventricles], are transvenously connected from the pacemaker to both sides of the heart. Once the pacemaker is implanted, it is programmed so that both ventricles are stimulated to contract after atrial contraction with the goal of improving left ventricle function, reducing presystolic mitral regurgitation, and improving LV diastolic filling time. The most frequently reported complication of CRT is lead dislodgement, which occurs in approximately 9% of patients.
Is biventricular pacing considered medically necessary?
Cardiac resynchronization therapy, biventricular pacing ( CRT-P )will be considered medically necessary when the following criteria are met (1 or 2):
How many leads are needed for biventricular pacemaker?
Biventricular pacemakers using three leads (one in the right atrium, one endocardial in the right ventricle, one epicardial for the left ventricle), also known as cardiac resynchronization therapy (CRT), have been investigated as a technique to coordinate the contraction of the ventricles, thus improving patients' hemodynamic status. Originally developed CRT devices typically used two ventricular leads for biventricular pacing. Devices and implantation techniques have been developed to allow for multisite pacing, with the goal of improving CRT response. This may be accomplished in one of two ways: through the use of multiple leads within the coronary sinus (triventricular pacing) or through the use of multipolar left ventricular pacing leads, which can deliver pacing stimuli at multiple sites. Wireless left ventricular endocardial pacing is also being evaluated for patients who are not candidates for or do not respond to standard epicardial pacing leads.
What percentage of heart failure patients have intraventricular conduction disorders?
It is estimated that 20% to 30% of patients with heart failure have intraventricular conduction disorders resulting in a contraction pattern that is not coordinated and a wide QRS interval on the electrocardiogram. This abnormality appears to be associated with increased morbidity and mortality.

Understanding The Heart
How The Device Works
- Heart failure weakens your heart muscle. As a result, the ventricles don’t pump as strongly as they should. The pathways that carry the heart's electrical signals are located in the heart muscle. They can also be damaged by CHF. This can cause a bundle branch block. A bundle branch block can throw off the timing of the heart's contraction. This can make the heart's squeezing contraction …
Before The Procedure
- Make sure to: 1. Not eat or drink after midnight or 8 hours before your surgery 2. Follow instructions from your doctor about bathing the night before and the morning of your procedure. You may need to use a special cleaning solution. 3. Tell your doctor what medicines you take. This includes over-the-counter medicines such as ibuprofen. It also includes vitamins, herbs, an…
During The Procedure
- You will get medicine (anesthesia) so you won’t feel pain. Most likely, you will get medicine (sedation) that will make you drowsy or lightly asleep. The doctor will inject local pain medicine to n...
- The doctor will make an incision where the device will be implanted. This is most often on the left side of the chest just below the collarbone (clavicle).
- You will get medicine (anesthesia) so you won’t feel pain. Most likely, you will get medicine (sedation) that will make you drowsy or lightly asleep. The doctor will inject local pain medicine to n...
- The doctor will make an incision where the device will be implanted. This is most often on the left side of the chest just below the collarbone (clavicle).
- The doctor makes a small “pocket” for the generator under the skin.
- The doctor will put a thin, flexible tube (catheter) into a vein leading to the right atrium. He or she will guide the device’s wires (leads) through the catheter to the heart. The doctor will use...
After The Procedure
- You will spend several hours in a recovery room. Once you are stable and awake, you will be put in a room that can monitor your heart rhythm. Your healthcare team will also watch your breathing and other vital signs. You’ll be given pain medicine if you need it. The team may place the arm on the side of the device in a sling. This is just for a short time, to keep the arm and shoulder still. Y…
Recovering at Home
- Follow all the instructions your healthcare provider gives you for medicines, bathing, exercise, diet, and wound care. Ask your doctor when you can go back to work or start driving again. Don’t raise your arm above your shoulder on the side of your incision until your doctor says it’s OK to do so. This gives the leads a chance to secure themselves inside your heart.
Follow-Up Care
- Make sure to keep all your follow-up appointments. This is so your doctor can download information from your device and check its settings. Be sure to tell your doctor how the device is working for you. Most devices can now be connected to a wireless home monitoring system via the internet. The monitor can download information from your device and send it to your doctor. …
Life with A Biventricular Pacemaker and Icd
- Carry an ID card. When you first get your pacemaker, you’ll be given an ID card to carry. This card contains important information about the device. Show it to any doctor, dentist, or other provide...
- Be careful when using a cell phone. Hold it to the ear farthest from your pacemaker. Don’t carry the phone in your breast pocket, even when it’s turned off.
- Carry an ID card. When you first get your pacemaker, you’ll be given an ID card to carry. This card contains important information about the device. Show it to any doctor, dentist, or other provide...
- Be careful when using a cell phone. Hold it to the ear farthest from your pacemaker. Don’t carry the phone in your breast pocket, even when it’s turned off.
- Avoid very strong magnets. These include those used for an MRI or in hand-held security wands. Show your ID card when you go through security.
- Avoid strong electrical fields. These are made by radio transmitting towers and ham radios. They are also made by heavy-duty electrical equipment. A running engine makes an electrical field. Don't...
Popular Posts:
- 1. icd 10 code for l foot osteomyelitis
- 2. what is the icd 10 code for contact with and exposure to asbestos
- 3. icd 10 code for bacterial pneumonia with sepsis
- 4. icd 10 code for side effects of clindamycin
- 5. icd 10 code for anterior uveitis right lid
- 6. icd 10 code for trach status
- 7. icd 10 code for right obstructive ureteral calculi with severe hydronephrosis
- 8. icd 10 code for muscle weakness left arm initial encounter
- 9. icd 10 code for newborn head molding
- 10. icd-10 code for traumatic subdural hematoma with loss of consciousness