Pain, unspecified. R52 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
What is the diagnosis code for body aches?
- Able to cope
- Able to cope with pain
- Aching pain
- Acute pain
- Alimentary tract pain due to vascular insufficiency
- Alteration in comfort: chronic pain
- Alteration in comfort: pain
- Application site pain
- Burning pain
- Catch
What does it mean when your whole body aches?
Muscle pain that affects a small part of your body is usually caused by overuse -- sore arms from lifting boxes all day, for example. Or it could be a minor injury, like a bruised shoulder after a fall. But when you ache all over your body, it’s more likely caused by an infection, illness, or medicine you’ve taken.
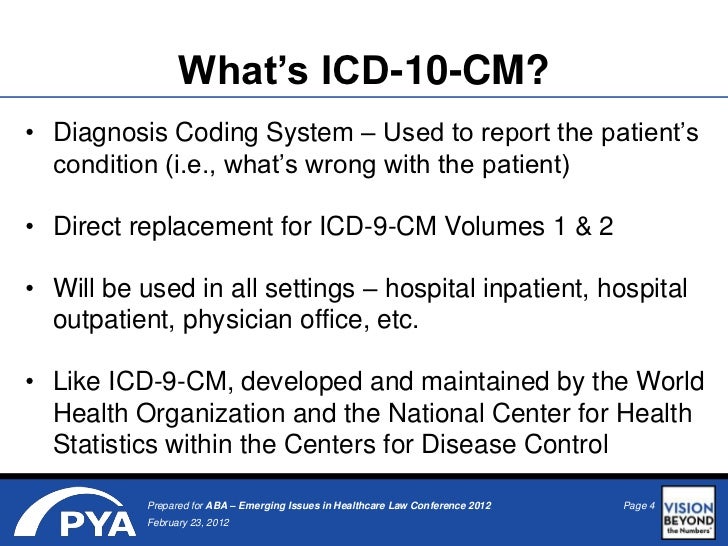
What is the ICD 10 diagnosis code for?
The ICD-10-CM is a catalog of diagnosis codes used by medical professionals for medical coding and reporting in health care settings. The Centers for Medicare and Medicaid Services (CMS) maintain the catalog in the U.S. releasing yearly updates.
What is ICD 10 code for severe persistent asthma?
Severe persistent asthma, uncomplicated. J45.50 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM J45.50 became effective on October 1, 2021.
What is the ICD-10 code for body aches?
ICD-10-CM Code for Myalgia M79. 1.
What is Myalgia unspecified?
Myalgia describes muscle aches and pain, which can involve ligaments, tendons and fascia, the soft tissues that connect muscles, bones and organs. Injuries, trauma, overuse, tension, certain drugs and illnesses can all bring about myalgia.
What is ICD-10 code M79?
2022 ICD-10-CM Diagnosis Code M79: Other and unspecified soft tissue disorders, not elsewhere classified.
What is diagnosis code Z71 89?
Other specified counselingICD-10 code Z71. 89 for Other specified counseling is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
What is myalgia and arthralgia?
Arthralgia is joint pain. Myalgia is muscle pain. Both can be a possible side effect of some chemotherapies, some hormonal therapy agents, growth factors, or a very high white blood cell count. Chemotherapy related pain commonly occurs within two to three days of treatment and resolves within four to seven days.
What's the difference between myalgia and fibromyalgia?
And whereas fibromyalgia is chronic, often lasting a lifetime, polymyalgia usually resolves itself within two years. Treatment differs, too. Fibromyalgia is treated with exercise, relaxation techniques, analgesic medications and antidepressants to relieve pain and promote sleep.
What is the ICD-10 code for joint Pain?
ICD-Code M25. 50 is a billable ICD-10 code used for healthcare diagnosis reimbursement of Pain in Unspecified Joint.
What is the ICD-10-CM code for chronic pain?
NOTE: To utilize these chronic pain diagnosis codes, the exact nature of pain should be specifically documented in the patient medical records; such as “chronic” to utilize ICD-10 code G. 89.29 or the diagnosis term “chronic pain syndrome” to utilize ICD-10 code G89. 4.
What is the ICD-10 code for arthralgia?
The 2022 edition of ICD-10-CM M26. 629 became effective on October 1, 2021. This is the American ICD-10-CM version of M26.
Can Z76 89 be a primary diagnosis?
The patient's primary diagnostic code is the most important. Assuming the patient's primary diagnostic code is Z76. 89, look in the list below to see which MDC's "Assignment of Diagnosis Codes" is first. That is the MDC that the patient will be grouped into.
Is Z76 89 a billable code?
Z76. 89 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
What is the ICD-10 code for no diagnosis?
The DSM-5 Steering Committee subsequently approved the inclusion of this category, and its corresponding ICD-10-CM code, Z03. 89 "No diagnosis or condition," is available for immediate use.
What are the symptoms of myalgia?
Myalgia SymptomsDeep muscle pain in the local area or widespread pain.Dull or sharp aching pain.Mild or severe pain that may last minutes or be constant.Pain with rest or movement.
What does myalgia mean in medical terms?
Listen to pronunciation. (my-AL-juh) Pain in a muscle or group of muscles.
What is myalgia and myositis unspecified?
The word fibro derives from the New Latin, “Fibro” – meaning “fibrous tissue” while myalgia implies pain. People who suffer from fibromyalgia experience chronic widespread muscle and joint pain. Advertisement. Myositis means the muscles are inflamed. Inflammation doesn't always cause pain; sometimes it causes weakness.
How is myalgia diagnosed?
Myalgia is diagnosed by clinical examination. Pain can be provoked by digital palpation of the muscles of mastication. Highly localized hypersensitive spots (trigger points) are typical findings. Patients seek treatment primarily to relieve the pain.
What is pain in the nervous system?
Intensely discomforting, distressful, or agonizing sensation associated with trauma or disease, with well-defined location, character, and timing. Pain is a feeling triggered in the nervous system. Pain may be sharp or dull. It may come and go, or it may be constant.
What does it mean to feel pain?
Sensation of unpleasant feeling indicating potential or actual damage to some body structure felt all over, or throughout the body. Severe pain of limited duration. The sensation of discomfort, distress, or agony, resulting from the stimulation of specialized nerve endings.
What is a disorder characterized by the sensation of marked discomfort, distress or agony?
An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Causing physical or psychological misery, pain or distress. Intensely discomforting, distressful, or agonizing sensation associated with trauma or disease, ...
How long does pain last without pain?
Once you take care of the problem, pain usually goes away. However, sometimes pain goes on for weeks, months or even years. This is called chronic pain.
What is pain in the abdominal region?
A disorder characterized by a sensation of marked discomfort in the abdominal region. Painful sensation in the abdominal region. Sensation of discomfort, distress, or agony in the abdominal region; generally associated with functional disorders, tissue injuries, or diseases.
Is chest pain a serious problem?
The pain may start somewhere else, such as your chest. Severe pain doesn't always mean a serious problem. Nor does mild pain mean a problem is not serious. Call your healthcare provider if mild pain lasts a week or more or if you have pain with other symptoms.
What is the medical term for pain in the neck, shoulders, back, hips, and legs?
M60.-) (my-al-juh) pain in a muscle or group of muscles. A chronic disorder of unknown etiology characterized by pain, stiffness, and tenderness in the muscles of neck, shoulders, back, hips, arms, and legs. Other signs and symptoms include headaches, fatigue, sleep disturbances, and painful menstruation.
What is a thoracic myofascial pain syndrome?
Clinical Information. (my-al-juh) pain in a muscle or group of muscles. A chronic disorder of unknown etiology characterized by pain, stiffness, and tenderness in the muscles of neck, shoulders, back, hips, arms, and legs.
What chapter is a sign and symptom?
Some signs and symptoms are classified in the body system chapters. Before assigning a code from Chapter 18, the medical record must be reviewed to determine if the symptom or sign relates to a more specific diagnosis that is documented in the medical record, and the alphabetic index must be referenced to determine whether ...
What is the O28 code?
Category O28, Abnormal findings on antenatal screening of mother, contains codes for the general type of abnormal finding . Laboratory abnormal findings include hematological (O28.0), biochemical (O28.1), and cytological (O28.2) findings. Radiological abnormal findings include ultrasonic (O28.3) and other radiological studies (O28.4). There is also a code for abnormal chromosomal and genetic findings (O28.5), as well as codes for other abnormal findings (O28.8) and unspecified abnormal findings (O28.9). During pregnancy, abnormal findings would be reported with codes in Category O28 instead of codes from Chapter 18.
What are the factors to be considered when reporting codes from Chapter 18?
This article covers only two factors to be considered when reporting codes from Chapter 18 – whether or not the signs and symptoms routinely are associated with a documented definitive diagnosis, and whether the sign or symptom should be reported with a code from one of the body system chapters. However, prior to assigning codes for symptoms, signs, and abnormal findings, all guidelines should be reviewed. Guidelines related to symptoms, signs and abnormal findings are found in a number of sections, including the General Coding Guidelines (Section I.B.4,5,and 6), the Chapter-Specific Guidelines (Section I.C.18), Selection of Principal Diagnosis (Section II.A), Reporting Additional Diagnosis (Section III.B), and Diagnostic Coding and Reporting Guidelines for Outpatient Services (Section IV.D and P). Taking time to review the guidelines, along with the notes at the beginning of Chapter 18 and coding instructions listed at the category, subcategory, and code levels, should ensure that the correct sign, symptom, or abnormal finding code is assigned.
Popular Posts:
- 1. icd 10 code for iga deficiency
- 2. icd 9 code for arthritis 354.2
- 3. icd 10 code for non pressure ulcer right great toe
- 4. icd 10 code for crush injury left index finger
- 5. icd 10 cm code for long term current use of aspirin
- 6. icd 10 code for q tip
- 7. 2017 icd 10 code for reactive airway changes left lung
- 8. icd-10 code for symptoms of lymphnode
- 9. icd 9 code for psoriasis of scalp
- 10. icd 10 code for atypical lobular hyperplasia