Dietary calcium deficiency. E58 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2019 edition of ICD-10-CM E58 became effective on October 1, 2018.
What is the ICD 10 code for calcium deficiency?
Dietary calcium deficiency. E58 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2019 edition of ICD-10-CM E58 became effective on October 1, 2018. This is the American ICD-10-CM version of E58 - other international versions of ICD-10 E58 may differ.
What is the ICD 10 code for screening for other disorders?
2018/2019 ICD-10-CM Diagnosis Code Z13.89. Encounter for screening for other disorder. Z13.89 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
What is the ICD 10 code for osteoporosis screening?
Encounter for screening for osteoporosis. Z13.820 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2018/2019 edition of ICD-10-CM Z13.820 became effective on October 1, 2018.
What is the ICD 10 code for screening for cardiovascular disorders?
Encounter for screening for cardiovascular disorders. Z13.6 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
What is the ICD-10 code for calcium scoring?
ICD-10 code I25. 84 for Coronary atherosclerosis due to calcified coronary lesion is a medical classification as listed by WHO under the range - Diseases of the circulatory system .
What is the ICD-10 code Z13 89?
Code Z13. 89, encounter for screening for other disorder, is the ICD-10 code for depression screening.
What is the ICD-10 code for bone density screening?
Encounter for screening for osteoporosis Z13. 820 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM Z13. 820 became effective on October 1, 2021.
What is the ICD-10 code for screening?
9.
What does Z13 31 mean?
ICD-10 code Z13. 31 for Encounter for screening for depression is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
What is code Z12 39?
39 (Encounter for other screening for malignant neoplasm of breast). Z12. 39 is the correct code to use when employing any other breast cancer screening technique (besides mammogram) and is generally used with breast MRIs.
What ICD-10 codes does Medicare cover for DEXA scan?
ICD-10 CM code Z79. 83 should be reported for DXA testing while taking medicines for osteoporosis/osteopenia. ICD-10 CM code Z09 should be reported for an individual who has COMPLETED drug therapy for osteoporosis and is being monitored for response to therapy.
What diagnosis will cover a bone density test?
Bone mass measurements Your X-rays show possible osteoporosis, osteopenia, or vertebral fractures. You're taking prednisone or steroid-type drugs or are planning to begin this treatment. You've been diagnosed with primary hyperparathyroidism. You're being monitored to see if your osteoporosis drug therapy is working.
How do you code a bone density test?
CPT code for this procedure for one or more sites is 77080. CPT code for vertebral fracture assessment is 77082. A DEXA scan is currently the most widely-used test in measuring bone mineral density.
What is the ICD-10 code for preventive care?
The adult annual exam codes are as follows: Z00. 00, Encounter for general adult medical examination without abnormal findings, Z00.
What is the ICD-10 code for annual wellness visit?
An initial Annual Wellness Visit code is documented using G0438, subsequent Annual Wellness Visits are documented using code G0439.
What are preventive ICD-10 codes?
“Routine” diagnosis codes are considered Preventive. For example: ICD-10-CM codes Z00. 121, Z00. 129, Z00.
When will the ICD-10 Z13.820 be released?
The 2022 edition of ICD-10-CM Z13.820 became effective on October 1, 2021.
What is screening for asymptomatic individuals?
Screening is the testing for disease or disease precursors in asymptomatic individuals so that early detection and treatment can be provided for those who test positive for the disease. Type 1 Excludes. encounter for diagnostic examination-code to sign or symptom. Encounter for screening for other diseases and disorders.
When will the ICD-10 Z13.89 be released?
The 2022 edition of ICD-10-CM Z13.89 became effective on October 1, 2021.
What is the ICd 10 code for a syringe?
Encounter for screening for other disorder 1 Z13.89 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. 2 The 2021 edition of ICD-10-CM Z13.89 became effective on October 1, 2020. 3 This is the American ICD-10-CM version of Z13.89 - other international versions of ICD-10 Z13.89 may differ.
What is screening for asymptomatic individuals?
Screening is the testing for disease or disease precursors in asymptomatic individuals so that early detection and treatment can be provided for those who test positive for the disease. Type 1 Excludes. encounter for diagnostic examination-code to sign or symptom. Encounter for screening for other diseases and disorders.
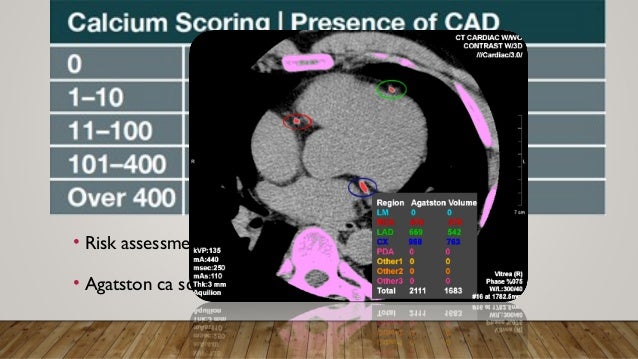
Why does Aetna use calcium scoring?
Aetna considers calcium scoring (e.g., with ultrafast [electron-beam] CT, spiral [helical] CT, and multi-slice CT) experimental and investigational for all other indications because of insufficient evidence in the peer-reviewed published medical literature.
What is CCTA in medical terms?
Coronary computed tomography angiography (CCTA) is a noninvasive imaging modality designed to be an alternative to invasive cardiac angiography (cardiac catheterization) for diagnosing CAD by visualizing the blood flow in arterial and venous vessels. The gold standard for diagnosing coronary artery stenosis is cardiac catheterization.
Does Aetna recommend CT angiography?
Aetna considers cardiac computed tomography (CT) angiography medically necessary for evaluation of aortic erosion in symptomatic members (e.g., chest pain) who have been treated for atrial septal defect with an occlusive device.
Does Aetna use a single calcium score?
Aetna considers a single calcium scoring by means of low-dose multi-slice CT angiography, ultrafast [electron-beam] CT, or spiral [helical] CT medically necessary for screening the following:
Is repeat calcium scoring necessary?
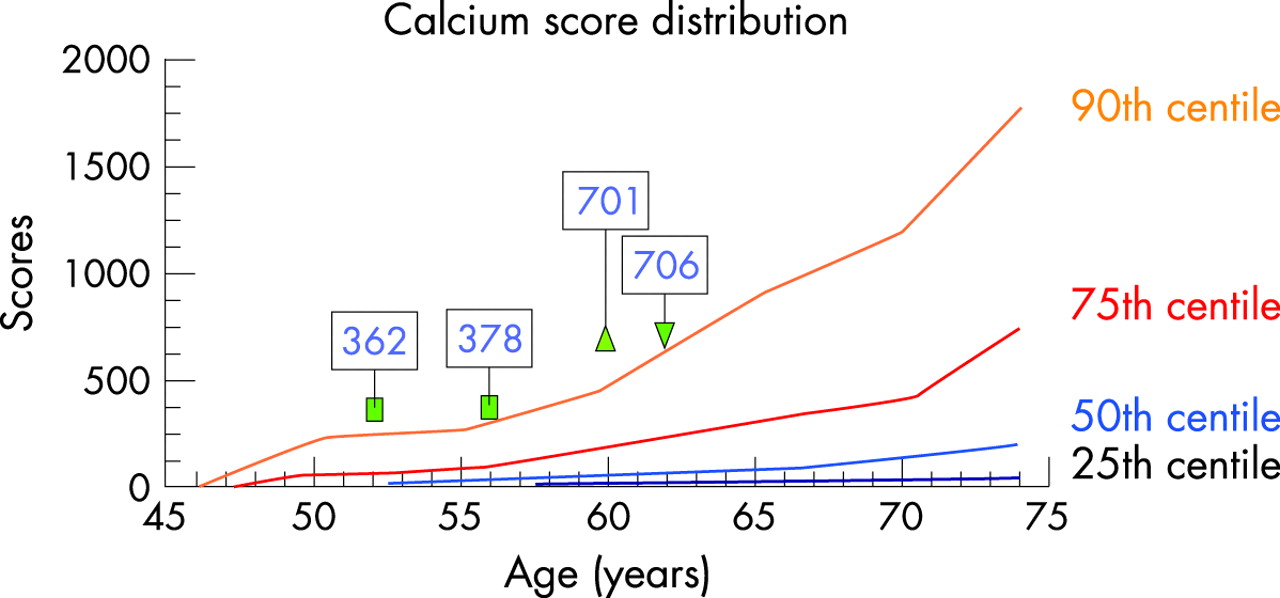
Repeat calcium scoring is considered medically necessary only if the following criteria are met:
Is calcium scoring necessary for aortic valve?
Aetna considers calcium scoring of the aortic valve medically necessary in the setting of persons with suspected paradoxical low-flow, low-gradient symptomatic severe aortic stenosis when transthoracic echocardiography is inconclusive.
Is cardiac CT angiography experimental?
Aetna considers cardiac CT angiography experimental and investigational for persons with any of the following contraindications to the procedure because its effectiveness for indications other than the ones listed above has not been established:
What happens if you submit a claim without a diagnosis code?
A claim submitted without a valid ICD-10-CM diagnosis code will be returned to the provider as an incomplete claim under Section 1833 (e) of the Social Security Act.
What is CMS in healthcare?
The Centers for Medicare & Medicaid Services (CMS), the federal agency responsible for administration of the Medicare, Medicaid and the State Children's Health Insurance Programs, contracts with certain organizations to assist in the administration of the Medicare program. Medicare contractors are required to develop and disseminate Articles. CMS believes that the Internet is an effective method to share Articles that Medicare contractors develop. While every effort has been made to provide accurate and complete information, CMS does not guarantee that there are no errors in the information displayed on this web site. THE UNITED STATES GOVERNMENT AND ITS EMPLOYEES ARE NOT LIABLE FOR ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION, PRODUCT, OR PROCESSES DISCLOSED HEREIN. Neither the United States Government nor its employees represent that use of such information, product, or processes will not infringe on privately owned rights. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information, product, or process.
Does ICD-10-CM code cover a service?
The use of an ICD-10-CM code listed below does not assure coverage of a service. The service must be reasonable and necessary in the specific case and must meet the criteria specified in the attached determination.
Can you use CPT in Medicare?
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials of CMS internally within your organization within the United States for the sole use by yourself, employees and agents. Use is limited to use in Medicare, Medicaid or other programs administered by the Centers for Medicare and Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
What is CMS in healthcare?
The Centers for Medicare & Medicaid Services (CMS), the federal agency responsible for administration of the Medicare, Medicaid and the State Children's Health Insurance Programs, contracts with certain organizations to assist in the administration of the Medicare program. Medicare contractors are required to develop and disseminate Local Coverage Determinations (LCDs). CMS believes that the Internet is an effective method to share LCDs that Medicare contractors develop. While every effort has been made to provide accurate and complete information, CMS does not guarantee that there are no errors in the information displayed on this web site. THE UNITED STATES GOVERNMENT AND ITS EMPLOYEES ARE NOT LIABLE FOR ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION, PRODUCT, OR PROCESSES DISCLOSED HEREIN. Neither the United States Government nor its employees represent that use of such information, product, or processes will not infringe on privately owned rights. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information, product, or process.
Does Medicare cover physical checkups?
Under CMS National Coverage Policy for Title XVIII of the Social Security Act, §1862 (a) (1) (D) revised the verbiage to read “Items and services related to research and experimentation” and for Title XVIII of the Social Security Act, §1862 (a) (7) revised the verbiage to read “states Medicare will not cover any services or procedures associated with routine physical checkups”.
Can you use CPT in Medicare?
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials of CMS internally within your organization within the United States for the sole use by yourself, employees and agents. Use is limited to use in Medicare, Medicaid or other programs administered by the Centers for Medicare and Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
Does Medicare cover CCTA?
2. Medicare does not cover a screening CCTA for asymptomatic patients, for risk stratification or for quantitative evaluation of coronary calcium. This Local Coverage Determination (LCD) does not address Heartflow determinations.
Does CMS have a CDT license?
Organizations who contract with CMS acknowledge that they may have a commercial CDT license with the ADA, and that use of CDT codes as permitted herein for the administration of CMS programs does not extend to any other programs or services the organization may administer and royalties dues for the use of the CDT codes are governed by their commercial license.
Popular Posts:
- 1. icd 10 code for marijuana use during pregnancy
- 2. 2017 icd 10 code for bladder calculi
- 3. icd 10 code for right breast swelling with implant
- 4. icd 10 code for ulcer right lower leg
- 5. icd 10 code for e11.42
- 6. icd 10 pcs code for needle emg musculoskeletal system
- 7. icd 10 code for mild hypertrophy unspecified
- 8. icd 10 cm 2018 code for acute respiratory distress
- 9. icd 10 code for lumbago with sciatica unspec
- 10. icd 10 code for fusobacterium necrophorum