What is the ICD 10 code for chronic back pain?
The ICD 10 code for chronic back pain is M54.5 and it is used for diagnosis purposes. The code was introduced on October 1, 2018. This code is the American version and it is necessary that it is labeled thus.
What is the ICD 10 code for spondylosis in rheumatology?
Rheumatology medical coding involves using the specific ICD-10 diagnosis codes for reporting spondylosis on your medical claims. ICD-10-CM codes used to indicate a diagnosis of spondylosis include – M47.011 – Anterior spinal artery compression syndromes, occipito-atlanto-axial region
What is the ICD 10 code for post thoracotomy pain syndrome?
Chronic post-thoracotomy (after chest surgery) pain; Chronic post-thoracotomy pain syndrome ICD-10-CM Diagnosis Code L98.423 [convert to ICD-9-CM] Non-pressure chronic ulcer of back with necrosis of muscle Chronic ulcer of back with muscle necrosis; Chronic ulcer of back, muscle necrosis
What is the ICD 10 code for spondylosis without myelopathy?
Spondylosis without myelopathy or radiculopathy, lumbar region. M47.816 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.

What is the ICD-10-CM code for Spondylosis?
M47. 9 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM M47.
What is the ICD-10 code for lumbar Spondylosis?
ICD-10-CM Code for Spondylosis without myelopathy or radiculopathy, lumbar region M47. 816.
What is the diagnosis code for Spondylosis?
ICD-10 Code for Spondylosis without myelopathy or radiculopathy, cervical region- M47. 812- Codify by AAPC.
What is Spondylosis of the spine?
Spondylosis is a condition in which there is abnormal wear on the cartilage and bones of the neck (cervical vertebrae). It is a common cause of chronic neck pain. Spondylosis is caused by chronic wear on the spine.
What is the ICD-10 code for chronic pain?
89.29 or the diagnosis term “chronic pain syndrome” to utilize ICD-10 code G89. 4.
Is lumbar Spondylosis arthritis?
This age-related condition is called lumbar spondylosis. It's also frequently called arthritis of the lower back and results in chronic lower back pain that worsens with age and increases with movement. When this condition occurs in the neck, it's called cervical spondylosis.
What is the ICD-10 code for back pain?
5 – Low Back Pain. ICD-Code M54. 5 is a billable ICD-10 code used for healthcare diagnosis reimbursement of chronic low back pain.
What is the ICD-10 code M47 812?
M47. 812 Spondylosis w/o myelopathy or radiculopathy, cervical region - ICD-10-CM Diagnosis Codes.
What is the ICD-10 code for Spondylosis without myelopathy or radiculopathy?
M47.817Spondylosis without myelopathy or radiculopathy, lumbosacral region. M47. 817 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
What is the difference between spondylitis and spondylosis?
Spondylitis is the result of an inflammatory condition of the joint that causes arthritis. Spondylosis describes the vertebral joints' general wear and tear, resulting in degeneration of the disks and joints.
What is the difference between spondylosis and spondylolysis?
Spondylosis refers to degenerative changes within the spine, often related to arthritis; spondylolysis refers to a defect in the pars interarticularis of the vertebrae, often related to an injury.
Are spondylolisthesis and spondylosis the same thing?
Spondylosis involves the separation of the pars interarticularis. In contrast, spondylolisthesis is defined by a slipped vertebra. When one bone of the spine slips forward over another, it causes damage to the spinal structure. In some cases, a stress fracture may be to blame.
What is the ICd 10 code for back pain?
The ICD 10 code for chronic back pain is M54.5 and it is used for diagnosis purposes. The code was introduced on October 1, 2018. This code is the American version and it is necessary that it is labeled thus. The reason is that there are several other international codes which could cause a conflict if you are not sure of the origin.
Why is my lower back pain chronic?
Why the back pain is referred to as chronic is because it has been there for a while or it is recurring.
Why does my back hurt?
When the bones are porous and brittle, there is a greater risk of fractures. These are among the main causes of chronic back pain. Kidney stones. You could feel pain in your back if you have a kidney infection such as kidney stones. 3.
What causes back pain?
These are the most common causes of strains in the back. Muscle spasms. Strained ligaments or muscles. Damaged discs.
Where is the pain in the back?
In some cases it may be in the upper back while the most common are found in the lower back, sometimes extending to the buttocks and legs. With a little rest or corrective activity, the pain should go away.
Can you stay away from chronic back pain?
You should have gained some knowledge about the causes, symptoms, risks factors, and treatment associated with chronic back pain. With the knowledge gained you can stay away from chronic back pain for the rest of your life.
What is the term for pain in the lower back?
Sciatica – Pain which radiates down to one or both the legs from the lower back caused due to compression of the sciatic nerve by a herniated disk or a bone spur. Lumbago- The medical term for low back pain.
How long does back pain last?
Chronic back pain – Back pain is said to be chronic if it is a constant nagging pain usually lasting for more than 3-6 months duration, which begins to affect the daily routine of the person.
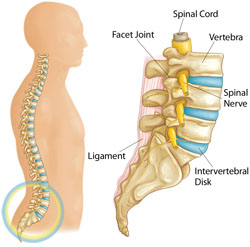
What is the longest region of the spine?
Cervicothoracic region – The region connecting the cervical and thoracic regions of the spine (C7-T1). Thoracic region – The longest region of the spine which extends from the base of the neck to the abdomen. It comprises of 12 vertebrae (T1 to T12).
Which region of the spine is curved slightly inwards and made of 5 vertebrae?
Lumbar region – The lower back region of the spine which is curved slightly inwards and made of 5 vertebrae (L1-L5). Lumbosacral region – The region connecting the last lumbar vertebrae to the sacrum which is made of 5 bones fused together.
Is back pain a symptom of a disease?
Back pain being a symptom of an underlying disease in most cases is coded only in the absence of a confirmed diagnosis of an underlying condition like intervertebral disc disorders, traumatic disc fracture, muscle strain etc..
How much does it cost to treat back pain?
It is estimated that 80 percent of Americans report back pain at one time or another, and treatment for such issues comes at a cost of $50 billion annually. Roughly 40 percent of those with back pain seek help from a primary care physician; another 40 percent see a chiropractor, and the remaining 20 percent find some other specialist for help.
What is the M50.2?
M50.2- and M51.2- are the subcategories for “other disc displacement,” and this phrase has led to some confusion. “Displacement” is a very general term that does not distinguish between disc bulges or prolapses. However, it is notable that it does not mention nervous system involvement.
Is myelopathy more serious than radiculopathy?
Myelopathy could include symptoms affecting the bowel and bladder, for example, and it is potentially much more serious and less common than radiculopathy, which typically only involves a single extremity. The fifth character for each of these codes identifies a specific anatomic location.
Documentation: Key to Coding
Documentation is the key to the correct code assignment when coding these conditions. Several of the codes are similar but vary slightly. Code 338.0 describes central pain syndrome; 338.4, Chronic pain syndrome; and 338.29, Other chronic pain. These conditions are different, and code assignments are based upon physician documentation.
Pain Coding Guidelines
With the creation of the new codes, guidelines related to these codes were added to the ICD-9-CM Official Guidelines for Coding and Reporting, effective November 15, 2006. A thorough review of these guidelines (section I. C. 6) is important for correct code assignment.
Principal or First-Listed Diagnosis
Category 338 codes are acceptable as the principal diagnosis (or first-listed code) for reporting purposes in two instances: when the related definitive diagnosis has not been established (confirmed) or when pain control or pain management is the reason for the admission or encounter.
Use of Category 338 Codes with Pain Codes
Category 338 should be used in conjunction with site-specific pain codes (including codes from chapter 16) if category 338 codes provide additional information about the pain, such as if it is acute or chronic.
Postoperative Pain
When postoperative pain is not associated with a specific postoperative complication, it is assigned to the appropriate postoperative pain code in category 338. Postoperative pain from a complication (such as a device left in the body) is assigned to the appropriate code (s) found in chapter 17, Injury and Poisoning.
Neoplasm-Related Pain
Code 338.3 is used to classify pain related to, associated with, or due to a tumor or cancer whether primary or secondary. This code is used as the principal code when the admission or encounter is for pain control or pain management. In this case, the underlying neoplasm should be reported in addition.
Popular Posts:
- 1. icd 10 cm code for acute coronary syndrome
- 2. icd 10 code for abrasion of right elbow
- 3. icd-10 code for hiv negative testing results
- 4. icd 10 code for vegetarian status
- 5. icd-10 code for quadriceps tendonitis
- 6. icd 10 code for family history of colon cancer syndrome
- 7. icd 9 code for autism in adults
- 8. icd 10 code for abnormal loss of weight
- 9. icd 10 code for post partum depression
- 10. icd 10 code for type 1 diabetes with peripheral neuropathy