What is the ICD 10 code for sepsis?
· Other specified sepsis. 2016 2017 2018 2019 2020 2021 2022 Billable/Specific Code. A41.89 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM …
What is the ICD 10 code for bacterial infection?
· ICD-9 Code: Nomenclature: ICD-10 Code: Nomenclature: 038.0: Streptococcal septicemia: A40.0: Sepsis due to streptococcus, group A: A40.1: Sepsis due to streptococcus, group B No code: A40.8: Other streptococcal sepsis No code: A40.9: Streptococcal sepsis, unspecified: 038.10: Staphylococcal septicemia, unspecified: A41.2: Sepsis due to unspecified …
What is the ICD 10 code for Enterobacter sakazakii infection?
· ICD 10 code for Sepsis due to E coli is A41.51. Patient presence for Sepsis due to Serratia: ICD 10 code for sepsis due to Serratia is A41.53. If the doctor documents “Sepsis” but the type of infection or causal organism is not specified, then will assign the A41.9 code, which indicates Sepsis, unspecified organism.
What is the CPT code for sepsis with E coli?
· B96.89 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. Short description: Oth bacterial agents as the cause of diseases classd elswhr The 2022 edition of ICD-10-CM …
What is the ICD-10 code for sepsis without acute organ failure?
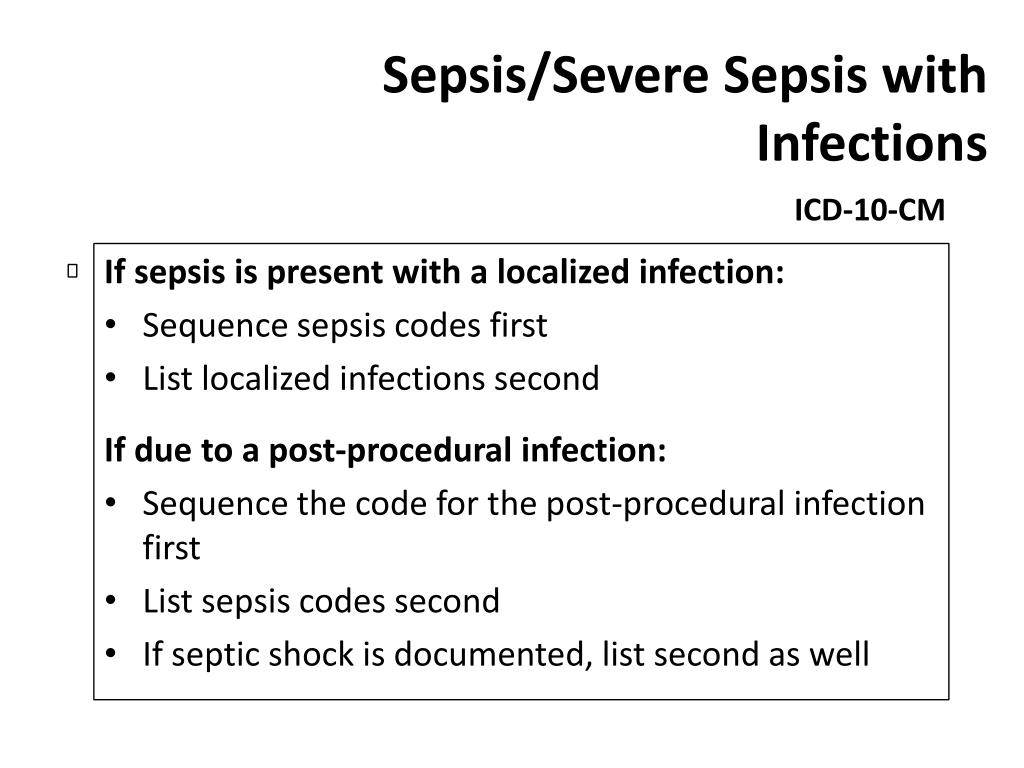
Because ICD-10-CM utilizes combination coding, sepsis without acute organ failure will require only one code: the code for the underlying systemic infection (A40.0 – A41.9). Complete and accurate coding of the condition of severe sepsis will continue to require a minimum of two codes. The first code sequenced in this combination identifies the underlying organism (Sepsis, A40.0 – A41.9) or cause of the sepsis (postprocedural infection, trauma, or burn), followed by a code indicating the extent to which the septic condition has progressed: severe sepsis with or without septic shock.#N#ICD-10-CM splits the condition of severe sepsis with combination codes R65.21 Severe sepsis with septic shock and R65.20 Severe sepsis without septic shock. As with other combination codes, assigning a separate code for septic shock in addition to the combination code is unnecessary. When documented, any associated organ dysfunction should be assigned following the code for severe sepsis. Although the condition of sepsis and its associated code may not be the first listed for the principle diagnosis, the sequencing of these codes remains the same.
What is the ICD-10 code for urosepsis?
Considered in ICD-10-CM as a nonspecific term and not associated with sepsis, the default code for this condition in ICD-9-CM (599.0 Urinary tract infection, site not specified) is not carried forward in ICD-10-CM. If the provider documents this condition, further clarification should be sought prior to coding.
Is septic shock a separate code?
As with other combination codes, assigning a separate code for septic shock in addition to the combination code is unnecessary. When documented, any associated organ dysfunction should be assigned following the code for severe sepsis. Although the condition of sepsis and its associated code may not be the first listed for the principle diagnosis, ...
What is the meaning of the code for sepsis?
Sepsis means potentially fatal condition caused when the body responses to the presence of infection or organisms in the blood. Choose the appropriate “A” code from the alphabetical index to indicate sepsis with type of infection or causal organism, if the doctor documents “Sepsis with type of infection or causal organism”.
What is the code for severe sepsis with septic shock?
Severe sepsis with septic shock: Septic shock means severe sepsis associated with circulatory failure. Assign the code in the same above format (severe sepsis) as it represents the type of acute organ dysfunction. But here, we will report a code R65.21 (which indicates severe sepsis with septic shock) instead of R65.20 (severe sepsis).
What is the A41.9 code?
If the doctor documents “Sepsis” but the type of infection or causal organism is not specified, then will assign the A41.9 code, which indicates Sepsis, unspecified organism.
When is the ICD-10 code for sepsis?
The 2021 edition of ICD-10-CM A41.5 became effective on October 1, 2020.
When will the ICD-10 A41.5 be released?
The 2022 edition of ICD-10-CM A41.5 became effective on October 1, 2021.
What is the code for sepsis?
A41.59 is a billable diagnosis code used to specify a medical diagnosis of other gram-negative sepsis. The code A41.59 is valid during the fiscal year 2021 from October 01, 2020 through September 30, 2021 for the submission of HIPAA-covered transactions.
How is sepsis treated?
People with sepsis are usually treated in hospital intensive care units. Doctors try to treat the infection, sustain the vital organs, and prevent a drop in blood pressure. Many patients receive oxygen and intravenous (IV) fluids. Other types of treatment, such as respirators or kidney dialysis, may be necessary.
How do you know if you have sepsis?
Doctors diagnose sepsis using a blood test to see if the number of white blood cells is abnormal. They also do lab tests that check for signs of infection.
Where does sepsis occur?
The infections are often in the lungs, stomach, kidneys, or bladder. It's possible for sepsis to begin with a small cut that gets infected or with an infection that develops after surgery. Sometimes, sepsis can occur in people who didn't even know that they had an infection.
When was the ICd 10 code implemented?
FY 2016 - New Code, effective from 10/1/2015 through 9/30/2016 (First year ICD-10-CM implemented into the HIPAA code set)
Can you get sepsis from a leaky heart?
In severe cases, one or more organs fail. In the worst cases, blood pressure drops and the heart weakens, leading to septic shock. Anyone can get sepsis, but the risk is higher in.
Can sepsis be caused by other conditions?
Many of the signs and symptoms of sepsis can also be caused by other medical conditions. This may make sepsis hard to diagnose in its early stages.
What is septic shock with acute organ dysfunction due to?
Septic shock with acute organ dysfunction due to group a streptococcus. Septic shock with acute organ dysfunction due to group b streptococcus. Septic shock with acute organ dysfunction due to meningococcal septicemia.
What is septic shock?
Septic shock with acute organ dysfunction. Septic shock with acute organ dysfunction due to anaerobic septicemia. Septic shock with acute organ dysfunction due to chromobacterium. Septic shock with acute organ dysfunction due to coagulate-negative staphylococcu.
When will the ICd 10-CM R65.21 be released?
The 2021 edition of ICD-10-CM R65.21 became effective on October 1, 2020.
What is post-procedural sepsis?
Post-procedural Sepsis and Sepsis Due to a Device, Implant, or Graft. A systemic infection can occur as a complication of a procedure or due to a device, implant, or graft. This includes systemic infections due to wound infection, infusions, transfusions, therapeutic injections, implanted devices, and transplants.
Why is severe sepsis not assigned?
For instance, if severe sepsis, pneumonia, and acute renal failure due to dehydration are documented, the code for severe sepsis may not be assigned because the acute renal failure is not stated as due to or associated with sepsis. If the documentation is unclear, query the physician.
What is the term for a lab finding of infectious organisms in the blood?
Bacteremia . Bacteremia is a lab finding of infectious organisms in the blood. The patient has no clinical signs of sepsis or SIRS. Bacteremia may be transient, or may lead to sepsis. When a patient’s blood cultures are positive and not believed to be a contaminant, the patient is usually treated with antibiotics.
When to query a physician for sepsis?
You must query the physician when the term “sepsis syndrome” is documented as a final diagnosis. Know when to Query. Sepsis is a complicated condition to code, and it is often necessary to query the physician to code the case correctly.
Can you code for sepsis?
Documentation issues: You can code for sepsis when the physician documents the term “sepsis.”. Documentation should be consistent throughout the chart. Occasionally, during an extended length of stay, sepsis may resolve quickly and the discharging doctor may not include the diagnosis of sepsis on the discharge summary.
Is sepsis a systemic infection?
term “sepsis” must also be documented to code a systemic infection. This is a major change from ICD-9-CM. If the term “sepsis” is not documented with “SIRS” when it’s due to a localized infection, you must ask for clarification from the physician.
Is septic shock documented without sepsis?
Documentation issues: The term “septic shock” is occasionally documented without the term “sepsis.”. According to the guidelines, for all cases of septic shock the code for the underlying systemic infection is sequenced first, followed by R65.21 Severe sepsis with septic shock or T81.12- Postprocedural septic shock.
What is the primary focus of a sepsis claim?
When reviewing sepsis claims, all too often the primary focus is on searching provider documentation for signs and symptoms and/or clinical indicators that support the diagnosis of sepsis, or that support a query regarding the presence of sepsis.
Do sepsis guidelines get overlooked?
Many times the more subtle details in the sepsis guidelines are overlooked, and sometimes they are not noticed at all. I would like to challenge readers to periodically review and re-review the guidelines in an effort to gain complete understanding of all aspects of sepsis coding, and consider the following sepsis coding scenarios.
Does sepsis equal noninfectious sepsis?
However, it is important to note here that the absence of positive blood cultures in a patient with severe sepsis does not equal noninfectious sepsis.
Is sepsis always sequenced as the principal diagnosis when it is present on admission?
Is sepsis always sequenced as the principal diagnosis when it is present on admission? Some may say yes , because after all, that’s what is stated in the official coding guidelines. However, my answer to this question is no, not always. I believe that there are very few absolutes in coding, and the sepsis guidelines are a good example of this. ICD-10-CM Official Coding Guidelines for Coding and Reporting direct us that “if severe sepsis is present on admission and meets the definition of principal diagnosis, the underlying systemic infection should be assigned as principal diagnosis followed by the appropriate code from subcategory R65.2 as required by the sequencing rules in the Tabular List.” We are further directed that, “if the reason for admission is both sepsis or severe sepsis and a localized infection, such as pneumonia or cellulitis, a code (s) for the underlying systemic infection should be assigned as principal diagnosis followed by the appropriate code from subcategory R65.2 as required by the sequencing rules in the Tabular List.”
Can negative blood cultures negate sepsis?
We are directed by ICD-10-CM Official Guidelines for Coding and Reporting that even though negative or inconclusive blood cultures do not negate a diagnosis of sepsis in patients with clinical evidence of the condition; providers should be queried under these circumstances. So in this scenario, which is an actual real-life scenario, the provider would need to be queried as to the cause of patient’s septic shock and whether it was a noninfectious source (possibly patient’s GI bleed) or a suspected infection before an appropriate principal diagnosis could be chosen.
Popular Posts:
- 1. icd 10 code for pain in right ankle in subtalar joint
- 2. icd-10 code for glucose test
- 3. icd 10 procedure code for permacath
- 4. icd 10 code for diabete screen
- 5. icd 10 code for intentional aspirin overdose
- 6. icd 10 code for elevated bp postpartum
- 7. icd 10 code for acute sexually transmitted disease
- 8. icd 10 cm code for heel spur
- 9. icd 10 code for lumbar disc narrowing
- 10. icd 10 code for right inguinal hernia unspecified