How do you code a colonoscopy?
To report screening colonoscopy on a patient not considered high risk for colorectal cancer, use HCPCS code G0121 and diagnosis code Z12. 11 (encounter for screening for malignant neoplasm of the colon).Dec 16, 2021
What is the ICD 9 code for colonoscopy?
45.23 Colonoscopy - ICD-9-CM Vol.
Can Z12 11 be a principal diagnosis?
The code Z12. 11 describes a circumstance which influences the patient's health status but not a current illness or injury. The code is unacceptable as a principal diagnosis.
What is the ICD 10 code for incomplete colonoscopy?
Incomplete Colonoscopy B Incomplete Colonoscopies) are 44388, 45378, G0105, and G0121.Jul 8, 2021
Is a colonoscopy?
A colonoscopy (koe-lun-OS-kuh-pee) is an exam used to detect changes or abnormalities in the large intestine (colon) and rectum. During a colonoscopy, a long, flexible tube (colonoscope) is inserted into the rectum. A tiny video camera at the tip of the tube allows the doctor to view the inside of the entire colon.Apr 18, 2020
What is the difference between a diagnostic and screening colonoscopy?
Screening colonoscopies and diagnostic colonoscopies are performed similarly using the same equipment. The difference is how the procedure is billed to your insurance. Billing will depend on your symptoms (or lack of symptoms) and what your doctor finds during the procedure.Jan 25, 2022
Is a follow up colonoscopy a screening?
For example, colonoscopy can be used as a follow-up for a patient with abnormalities identified during a previous colorectal cancer screening. In this situation, the primary purpose of the follow-up colonoscopy is not screening for colorectal cancer.
What is the ICD 10 code for colon polyp?
K63.5K63. 5 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
This Billing and Coding Article provides billing and coding guidance for Local Coverage Determination (LCD) L33671 (Diagnostic Colonoscopy). Please refer to the LCD for reasonable and necessary requirements.
ICD-10-CM Codes that Support Medical Necessity
It is the provider’s responsibility to select codes carried out to the highest level of specificity and selected from the ICD-10-CM code book appropriate to the year in which the service is rendered for the claim (s) submitted
ICD-10-CM Codes that DO NOT Support Medical Necessity
All those not listed under the “ICD-10 Codes that Support Medical Necessity” section of this article.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
What is colonoscopy procedure?
Definition of Terms Colonoscopy: A colonoscopy is a procedure that permits the direct examination of the mucosa of the entire colon by using a flexible lighted tube. The procedure is done with sedation in a hospital outpatient department, in a clinic , or an office facility. During the colonoscopy a doctor can biopsy and remove pre – cancerous ...
What is a screening colonoscopy?
General definitions of procedure indications from various specialty societies , including the ACA: * A screening colonoscopy is done to look for disease, such as cancer, and treat early conditions, if indicated, in people without symptoms. * A diagnostic colonoscopy is done to confirm or rule out a condition in a person who is symptomatic ...
What is a provider policy?
A provider also can be a place where medical care is given, like a hospital, clinic, or lab.This policy informs them about when a service may be covered.
Is colonoscopy a screening test?
This guideline applies only to people of average risk. Colonoscopy is only one of the screening tests that can be used. This benefit coverage guideline provides general information about how the health plan decides whether a colonoscopy is covered under the preventive or diagnostic (medical) benefits.
Is screening colonoscopy covered by insurance?
Colonoscopies are covered by insurance — with no copay, thanks to the Affordable Care Act — when the main purpose of the test is to screen for cancer in a person who is at average risk for cancer.
What does CPT code 45378 mean?
CPT code 45378 is the base code for a colonoscopy without biopsy or other interventions. It includes brushings or washings, if performed. This modifier also may be appended to therapeutic colonoscopies, such as 45385 (colonoscopy, with removal of tumor, polyp, or other lesion by snare technique).
What is the CPT code 45380?
CPT® 45380 in section: Colonoscopy, flexible, proximal to splenic flexure.
What is procedure code 45378?
CPT code 45378 is the base code for a colonoscopy without biopsy or other interventions. It includes brushings or washings, if performed. If the procedure is a screening exam, modifier 33 (preventative service) is appended.
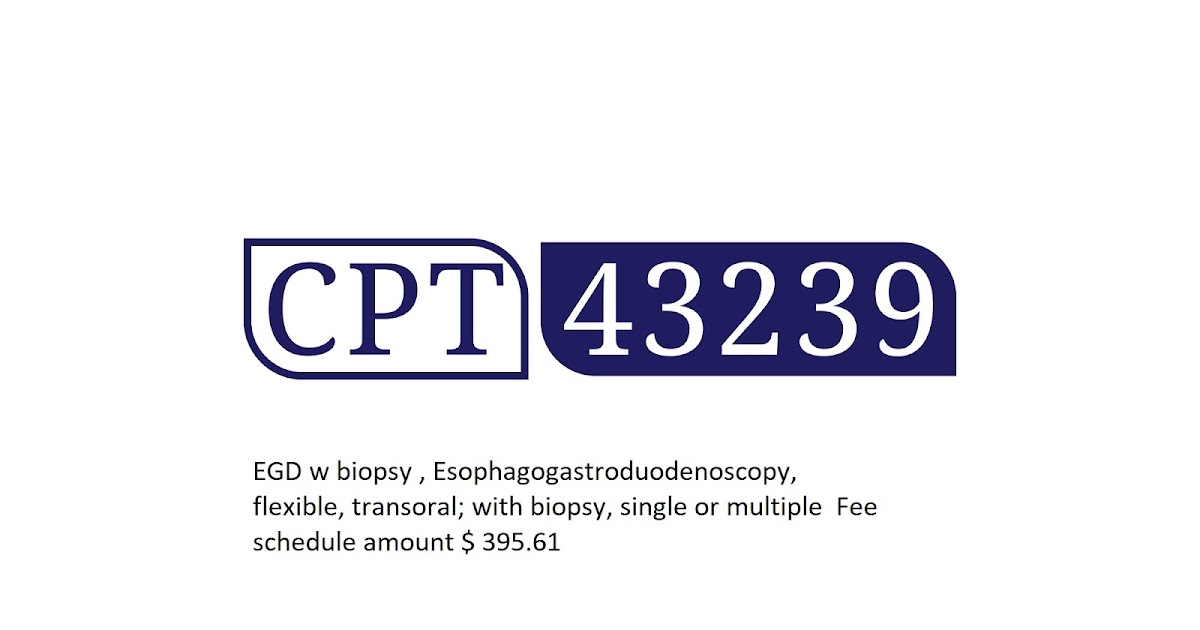
What is the difference between CPT code 43235 and 43239?
If no Biopsy is performed and the only procedure performed is an Esophageal Dilation using the scope instrument itself, only the 43235 Diagnostic EGD code is billable.#N#Most used CPT code list and description.
What is considered a screening colonoscopy?
Diagnostic Colonoscopy: Patient has past or present history of gastrointestinal symptoms or disease, polyps, or cancer. High Risk Screening Colonoscopy: Patient is asymptomatic (no gastrointestinal symptoms either past or present), but has personal history of gastrointestinal disease, colon polyps, or cancer.
Can 45380 and 45381 be billed together?
Hi Maarit, yes you are allowed to bill for only one procedure if several Px are performed in a single lesion. 45383 and 45380 performed on same lesion, you will report 45383 only as per the CPT assistant. The second scenario bill both the codes 45385 and 45381-51 as there is no bundling between these codes.
What is an incomplete colonoscopy?
Colonoscopy is the most widely used screening modality for the detection and removal of colon polyps and for the prevention of colorectal cancer. Incomplete colonoscopy rates vary from 4% to 25% and are associated with higher rates of interval proximal colon cancer.
What modifier is used for a failed procedure?
Submit CPT modifier 53 with surgical codes or medical diagnostic codes when the procedure is discontinued because of extenuating circumstances. This modifier is used to report services or procedure when the services or procedure is discontinued after anesthesia is administered to the patient.
What is the 52 modifier?
Modifier -52 (reduced services) indicates that a service was partially reduced or eliminated at a physician's discretion, per the CPT Manual. When a physician performs a bilateral procedure on one side only, append modifier -52.
What is a TC modifier?
Modifier TC is used when only the technical component of a procedure is being billed when certain services combine both the professional and technical portions in one procedure code. Use modifier TC when the physician performs the test but does not do the interpretation.
What is modifier 73 used for?
Modifier -73 is used by the facility to indicate that a surgical or diagnostic procedure requiring anesthesia was terminated due to extenuating circumstances or to circumstances that threatened the well being of the patient after the patient had been prepared for the procedure (including procedural pre-medication when
What is the difference between modifier 52 and 53?
By definition, modifier 53 is used to indicate a discontinued procedure and modifier 52 indicates reduced services. In both the cases, a modifier should be appended to the CPT code that represents the basic service performed during a procedure.
What is modifier 50 used for?
CPT Modifier 50 Bilateral Procedures – Professional Claims Only. Modifier 50 is used to report bilateral procedures that are performed during the same operative session by the same physician in either separate operative areas (e.g. hands, feet, legs, arms, ears), or one (same) operative area (e.g. nose, eyes, breasts).
What is the code for colonoscopy?
To report screening colonoscopy on a patient not considered high risk for colorectal cancer, use HCPCS code G0121 and diagnosis code Z12.11 ( encounter for screening for malignant neoplasm of the colon ).
What is a colonoscopy screening?
As such, “screening” describes a colonoscopy that is routinely performed on an asymptomatic person for the purpose of testing for the presence of colorectal cancer or colorectal polyps. Whether a polyp or cancer is ultimately found does not ...
What are the global periods for colonoscopy?
Typically, procedure codes with 0, 10 or 90-day global periods include pre-work, intraoperative work, and post-operative work in the Relative Value Units (RVUs) assigned . As a result, CMS’ policy does not allow for payment of an Evaluation and Management (E/M) service prior to a screening colonoscopy. In 2005, the Medicare carrier in Rhode Island explained the policy this way:
Does Medicare cover colonoscopy?
However, diagnostic colonoscopy is a test performed as a result of an abnormal finding, sign or symptom. Medicare does not waive the co-pay and deductible when the intent of the visit is to perform a diagnostic colonoscopy. Medicare waives the deductible but not the co-pay when a procedure scheduled as a screening is converted to a diagnostic ...
Is E/M covered by Medicare?
Medicare defines an E/M prior to a screening colonoscopy as routine, and thus non-covered. However, when the intent of the visit is a diagnostic colonoscopy an E/M prior to the procedure ordered for a finding, sign or symptom is a covered service.
What does PT mean in CPT?
The PT modifier ( colorectal cancer screening test, converted to diagnostic test or other procedure) is appended to the CPT ® code.
Can you remove polyps at screening colonoscopy?
It is not uncommon to remove one or more polyps at the time of a screening colonoscopy. Because the procedure was initiated as a screening the screening diagnosis is primary and the polyp (s) is secondary. Additionally, the surgeon does not report the screening colonoscopy HCPCS code, but reports the appropriate code for the diagnostic or therapeutic procedure performed, CPT ® code 45379—45392.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Title XVIII of the Social Security Act (SSA), §1862 (a) (1) (A) states that no Medicare payment shall be made for items or services that “are not reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member.”
Article Guidance
The following billing and coding guidance is to be used with its associated Local Coverage Determination.#N#Coding Guidelines#N#Do not report a colonoscopy procedure code for an endoscopy performed with a sigmoidoscope on a patient with a normal length colon, even if the sigmoidoscope reaches proximal to the splenic flexure.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
What is the ICD-10 code for colonoscopy without biopsy?
Point to note: Code 45378 is the base code for a colonoscopy without biopsy or other interventions. It includes brushings or washings if performed. Report 45378 with ICD-10 code Z86.010 on the first line of the CMS 1500 form.
What is the HCPCS code for colonoscopy?
For Medicare beneficiaries, screening colonoscopy is reported using the following HCPCS codes: - G0105 (Colorectal cancer screening; colonoscopy on individual at high risk), for a Medicare beneficiary at high risk for colorectal cancer, and the appropriate diagnosis code that necessitates the more frequent screening.
What is colonoscopy examination?
CPT defines a colonoscopy examination as "the examination of the entire colon, from the rectum to the cecum or colon-small intestine anastomosis, and may include an examination of the terminal ileum or small intestine proximal to an anastomosis" as well.
How often does Medicare require colonoscopy?
Medicare beneficiaries without high-risk factors are eligible for a screening colonoscopy every ten years. Beneficiaries at higher risk for developing colorectal cancer are eligible for screening once every 24 months. Medicare considers an individual who is at high risk of developing colorectal cancer as one who has one or more of the following:
What is a colonoscopy?
A Diagnostic colonoscopy is performed when an abnormal finding, sign, or symptom is found such as diarrhea, anemia, abdominal pain, or rectal bleeding. A Screening colonoscopy is performed on person without symptoms in order to test for the presence of colorectal cancer or colorectal polyps. Even if a polyp or cancer is found during ...
What modifier is used for colonoscopy?
53 - Medicare guidelines state that if a patient is scheduled for a screening colonoscopy, but because of poor prep the scope cannot be advanced beyond the splenic fixture, the procedure should be coded as a colonoscopy with modifier 53 (discontinued procedure).
How effective is colonoscopy?
According to a study by the American Cancer Society, 90% colorectal cancer (CRC) cases are detected in individuals with over 50 years in the U.S and colonoscopy is the most effective and the most commonly adopted procedure for the diagnosis and screening of CRC in older adults.
Popular Posts:
- 1. icd 10 code for mobility
- 2. icd 10 code for foreign body left elbow
- 3. icd 10 code for gram negative rods in urine
- 4. icd-10 code for deconditioning and weakness
- 5. icd 10 code for ulcer open right leg
- 6. icd 10 code for cerebral thrombosis of left posterior artery
- 7. icd 10 code for neuropathic pain foot
- 8. icd 10 code for chronic epistaxis
- 9. icd-10 code for gluten sensitivity
- 10. icd 10 code for post op appointment