How to code screening and diagnostic colonoscopy?
- G0121 – Colorectal cancer screening; colonoscopy on individual not meeting criteria for high risk
- G0105 – Colorectal cancer screening; colonoscopy on individual at high risk
- G0104 – Colorectal cancer screening; flexible sigmoidoscopy
What is the ICD 10 code for screening colonoscopy?
The following ICD-10 codes are used to report a screening colonoscopy:
- Z12.11: Encounter for screening for malignant neoplasm of the colon
- Z80.0: Family history of malignant neoplasm of digestive organs
- Z86.010: Personal history of colonic polyps
What is z12.11 diagnosis code?
POA Exempt | ICD-10 from 2011 - 2016 Z12.11 is a billable ICD code used to specify a diagnosis of encounter for screening for malignant neoplasm of colon. A 'billable code' is detailed enough to be used to specify a medical diagnosis.
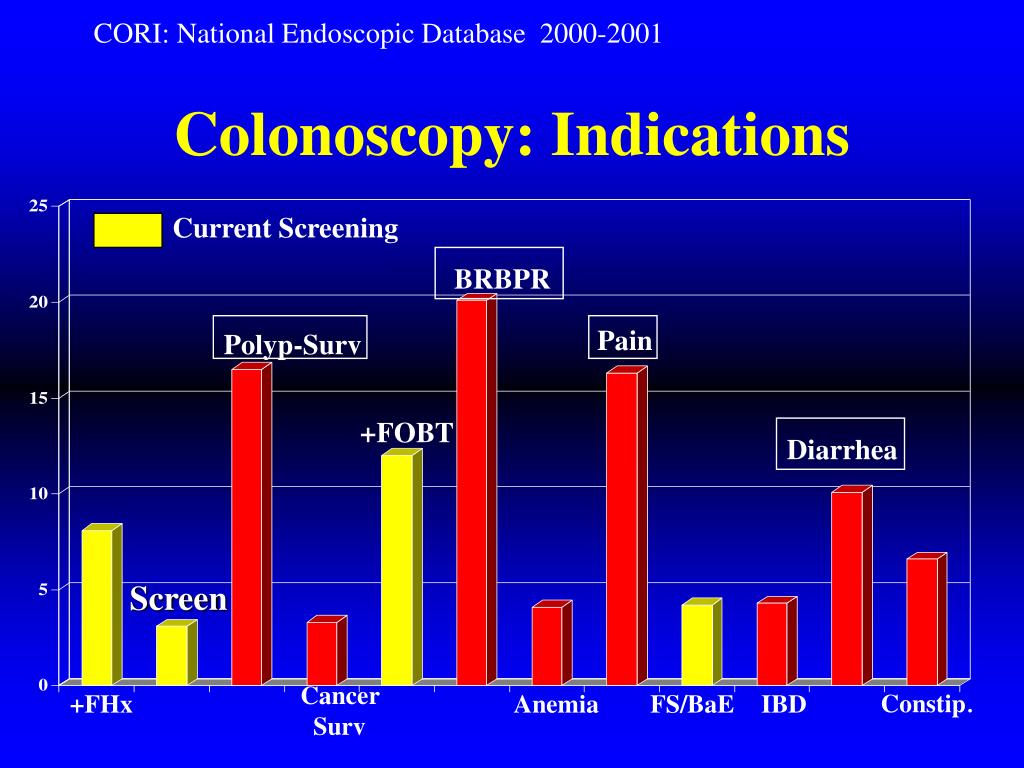
What is the diagnosis for colonoscopy?
Diagnostic Colonoscopy: Patient has past or present history of gastrointestinal symptoms or disease, polyps, or cancer. Additionally, if the colonoscopy is performed due to physical symptoms such as rectal bleeding or pain, the procedure will be considered diagnostic. What does the code include for a diagnostic colonoscopy? Colonoscopy CPT ® codes.
What is the diagnosis code for preventive colonoscopy?
Procedure code: G0121 (Average risk screening) or 45378-33 (Diagnostic colonoscopy with modifier 33 indicating this is a preventive service).
What does Z12 11 mean?
ICD-10 Code for Encounter for screening for malignant neoplasm of colon- Z12. 11- Codify by AAPC.
Does Medicare require prior authorization for colonoscopy?
Many people have extra coverage. However, Medicare requires prior authorization for a colonoscopy before most advantage plans start paying. Pre-approval means your doctor must get a green light before sending you to a Gastroenterologist.
How do I bill for a patient seen in our office prior to a screening colonoscopy with no GI symptoms and WHO is otherwise healthy?
How do I bill for a patient seen in our office prior to a screening colonoscopy with no GI symptoms and who is otherwise healthy? A visit prior to a screening colonoscopy for a healthy patient is not billable.
What does code Z12 31 mean?
For example, Z12. 31 (Encounter for screening mammogram for malignant neoplasm of breast) is the correct code to use when you are ordering a routine mammogram for a patient.
How do I code a Medicare screening colonoscopy?
G0121 – Colorectal cancer screening; colonoscopy on individual not meeting criteria for high risk.G0105 – Colorectal cancer screening; colonoscopy on individual at high risk.G0104 – Colorectal cancer screening; flexible sigmoidoscopy.
Does Medicare pay for colonoscopies?
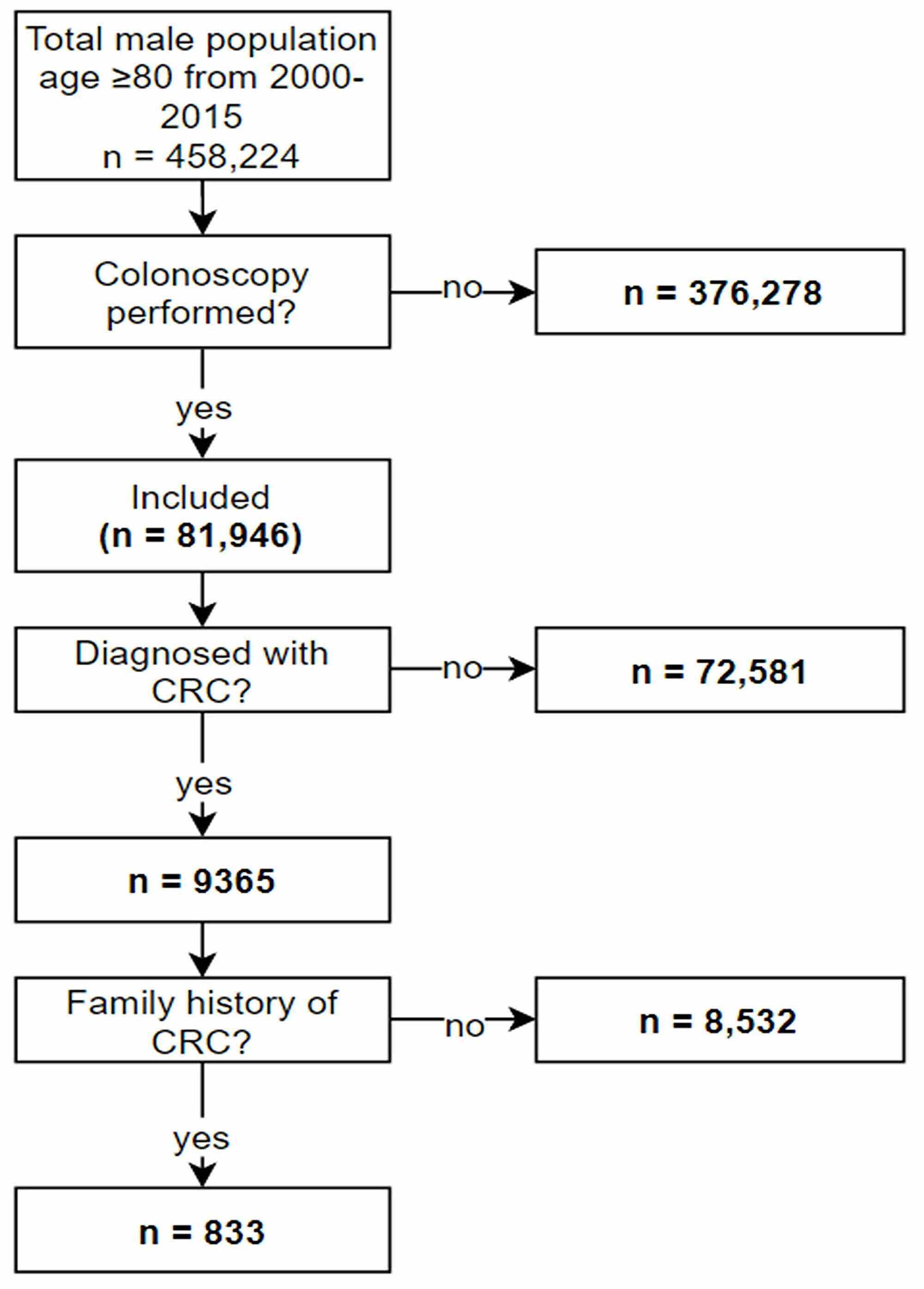
Colonoscopies. Medicare covers screening colonoscopies once every 24 months if you're at high risk for colorectal cancer. If you aren't at high risk, Medicare covers the test once every 120 months, or 48 months after a previous flexible sigmoidoscopy.
Does Medicare require pre authorization?
Traditional Medicare, in contrast, does not require prior authorization for the vast majority of services, except under limited circumstances, although some think expanding use of prior authorization could help traditional Medicare reduce inappropriate service use and related costs.
Does Medicare cover colonoscopies after age 75?
Screening guidelines from the U.S. Preventive Services Task Force recommend screening for colon cancer with any method, including colonoscopy, from age 50 to 75. Medicare reimburses colonoscopy, regardless of age.
What is the ICD-10 code for poor preparation for colonoscopy?
19.
How do you bill a screening colonoscopy turned diagnostic?
If during a colonoscopy a pathology is encountered that necessitates an intervention which converts the screening colonoscopy to a diagnostic/therapeutic colonoscopy, the appropriate CPT® code which includes the –PT modifier for the diagnostic/therapeutic colonoscopy must be submitted with an appropriate diagnosis to ...
When do you code a screening colonoscopy?
To report screening colonoscopy on a patient not considered high risk for colorectal cancer, use HCPCS code G0121 and diagnosis code Z12. 11 (encounter for screening for malignant neoplasm of the colon).
What does PT mean in CPT?
The PT modifier ( colorectal cancer screening test, converted to diagnostic test or other procedure) is appended to the CPT ® code.
What is the code for colonoscopy?
To report screening colonoscopy on a patient not considered high risk for colorectal cancer, use HCPCS code G0121 and diagnosis code Z12.11 ( encounter for screening for malignant neoplasm of the colon ).
What is a colonoscopy screening?
As such, “screening” describes a colonoscopy that is routinely performed on an asymptomatic person for the purpose of testing for the presence of colorectal cancer or colorectal polyps. Whether a polyp or cancer is ultimately found does not ...
What is a G0121?
Colonoscopy, flexible, proximal to splenic flexure; diagnostic, with or without collection of specimen (s) by brushing or washing, with or without colon decompression (separate procedure) G0121 ( colorectal cancer screening; colonoscopy on individual not meeting the criteria for high risk.
What are the global periods for colonoscopy?
Typically, procedure codes with 0, 10 or 90-day global periods include pre-work, intraoperative work, and post-operative work in the Relative Value Units (RVUs) assigned . As a result, CMS’ policy does not allow for payment of an Evaluation and Management (E/M) service prior to a screening colonoscopy. In 2005, the Medicare carrier in Rhode Island explained the policy this way:
Why is diagnosis code ordering important?
Diagnosis Code Ordering is Important for a Screening Procedure turned Diagnostic. When the intent of a visit is screening, and findings result in a diagnostic or therapeutic service, the ordering of the diagnosis codes can affect how payers process the claim.
What is 1862 A?
However, section 1862 (a) (1) (A) states that no payment may be made for items or services that are not reasonable and necessary for the diagnosis or treatment of an illness or injury or to improve the functioning of a malformed body member . In addition, section 1862 (a) (7) prohibits payment for routine physical checkups.
What is colonoscopy procedure?
Definition of Terms Colonoscopy: A colonoscopy is a procedure that permits the direct examination of the mucosa of the entire colon by using a flexible lighted tube. The procedure is done with sedation in a hospital outpatient department, in a clinic , or an office facility. During the colonoscopy a doctor can biopsy and remove pre – cancerous ...
What can a doctor do during a colonoscopy?
During the colonoscopy a doctor can biopsy and remove pre – cancerous polyps and some early stage cancers and also diagnose other conditions or diseases. General definitions of procedure indications from various specialty societies , including the ACA: * A screening colonoscopy is done to look for disease, such as cancer, ...
What is a provider policy?
A provider also can be a place where medical care is given, like a hospital, clinic, or lab.This policy informs them about when a service may be covered.
What is the introduction section of a medical policy?
Note:The Introduction section is for your general knowledge and is not to be takenas policy coverage criteria. The rest of the policy uses specific words and concepts familiar to medical professionals. It is intended for providers.A provider can be a person, such as a doctor, nurse, psychologist, or dentist.
Is colonoscopy a screening test?
This guideline applies only to people of average risk. Colonoscopy is only one of the screening tests that can be used. This benefit coverage guideline provides general information about how the health plan decides whether a colonoscopy is covered under the preventive or diagnostic (medical) benefits.
Can a colonoscopy be done during a biopsy?
It can also be doneas a diagnostic procedure when symptoms or lab tests suggest there might be a problem in the rectum or colon.In some cases, minor procedures may be done during a colonoscopy,such as taking a biopsy or destroying an area of unhealthy tissue (a lesion).
General Information
CPT codes, descriptions and other data only are copyright 2021 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Title XVIII of the Social Security Act, Section 1833 (e) states that no payment shall be made to any provider of services or other person under this part unless there has been furnished such information as may be necessary in order to determine the amounts due such provider or other person under this part for the period with respect to which the amounts are being paid or for any prior period..
Article Guidance
This Billing and Coding Article provides billing and coding guidance for Local Coverage Determination (LCD) L38812 (Diagnostic Colonoscopy).
ICD-10-CM Codes that Support Medical Necessity
It is the provider’s responsibility to select codes carried out to the highest level of specificity and selected from the ICD-10-CM code book appropriate to the year in which the service is rendered for the claim (s) submitted.
ICD-10-CM Codes that DO NOT Support Medical Necessity
All those not listed under the “ICD-10 Codes that Support Medical Necessity” section of this article.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Title XVIII of the Social Security Act, Section 1833 (e) states that no payment shall be made to any provider of services or other person under this part unless there has been furnished such information as may be necessary in order to determine the amounts due such provider or other person under this part for the period with respect to which the amounts are being paid or for any prior period..
Article Guidance
This Billing and Coding Article provides billing and coding guidance for Local Coverage Determination (LCD) L33671 (Diagnostic Colonoscopy). Please refer to the LCD for reasonable and necessary requirements.
ICD-10-CM Codes that Support Medical Necessity
It is the provider’s responsibility to select codes carried out to the highest level of specificity and selected from the ICD-10-CM code book appropriate to the year in which the service is rendered for the claim (s) submitted
ICD-10-CM Codes that DO NOT Support Medical Necessity
All those not listed under the “ICD-10 Codes that Support Medical Necessity” section of this article.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
General Information
CPT codes, descriptions and other data only are copyright 2021 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Title XVIII of the Social Security Act, Section 1833 (e) states that no payment shall be made to any provider of services or other person under this part unless there has been furnished such information as may be necessary in order to determine the amounts due such provider or other person under this part for the period with respect to which the amounts are being paid or for any prior period..
Article Guidance
This Billing and Coding Article provides billing and coding guidance for Local Coverage Determination (LCD) L38805 Colon Capsule Endoscopy (CCE). Please refer to the LCD for reasonable and necessary requirements.
ICD-10-CM Codes that Support Medical Necessity
It is the provider’s responsibility to select codes carried out to the highest level of specificity and selected from the ICD-10-CM code book appropriate to the year in which the service is rendered for the claim (s) submitted. The following ICD-10-CM diagnosis codes support medical necessity and provide coverage for CPT code: 91113.
ICD-10-CM Codes that DO NOT Support Medical Necessity
All those not listed under the “ICD-10 Codes that Support Medical Necessity” section of this article.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Title XVIII of the Social Security Act (SSA), §1862 (a) (1) (A) states that no Medicare payment shall be made for items or services that “are not reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member.”
Article Guidance
The following billing and coding guidance is to be used with its associated Local Coverage Determination. Coding Guidelines Do not report a colonoscopy procedure code for an endoscopy performed with a sigmoidoscope on a patient with a normal length colon, even if the sigmoidoscope reaches proximal to the splenic flexure.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
Popular Posts:
- 1. icd 10 code for cavitary lung lesion
- 2. icd 9 code for homelessness
- 3. icd 9 code for type 2 diabetes mellitus without complications
- 4. what is the icd-10 cm code for admission for adjustment of artificial leg
- 5. icd 10 code for vaginal ppain
- 6. icd 10 code for lifting strain in care giving role
- 7. what is icd-10-cm code for chronic serous otitis media
- 8. icd 10 code for infection of pacemaker pocket
- 9. icd 10 code for subcutaneous abscess
- 10. icd 10 code for status post vaccination