What is Procedure Code 96127?
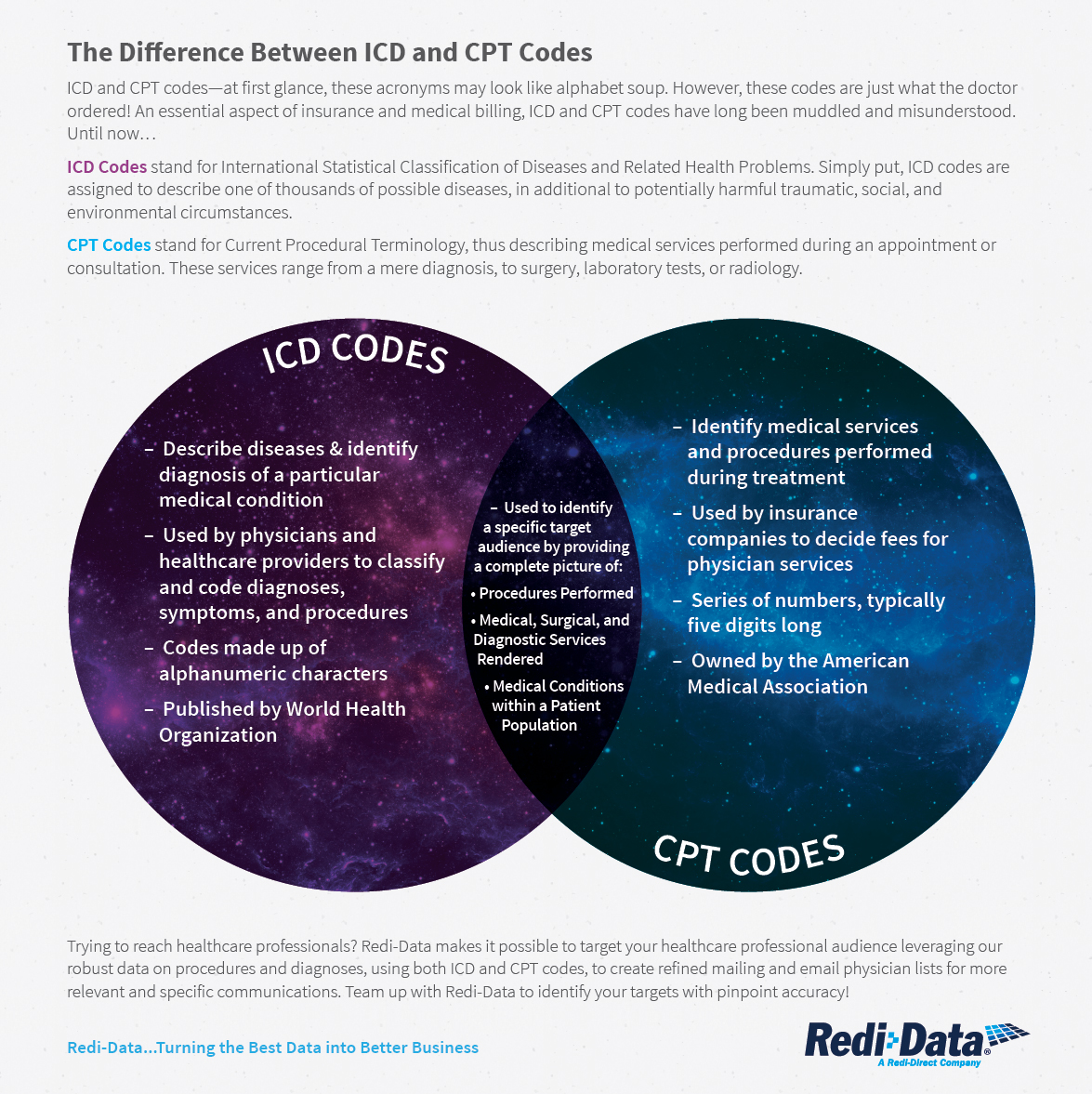
CPT Code 96127 – Brief Behavioral Assessment CPT Code 96127 may be used to report behavioral assessments in children and adolescents. CPT code description (AMA published) definition: Brief emotional/behavioral assessment with scoring and documentation, per standardized instrument.
Who can Bill 96127?
Patients can be screened and billing submitted for the following visits: post hospitalization, new diagnosis or complex medical issue, patients with pain, patients with substance abuse, and patients diagnosed with or being treated for mental illness. When can I bill for CPT 96127?
How CPT code 96127 can impact your income?
How CPT Code 96127 Can Impact Your Income. Video by . TherapyNotes. on . youtube · Looking for ways to boost revenue for your practice? Learn how CPT Code 96127 may ...
How to Bill 96127?
Billing for Standardized Screening: CPT 96127 (with Modifier 59) When you perform a standardized screen ing such as the PHQ -A or PHQ-9 , you should bill for it. This can be used whether you are using it with a well or evaluation and management ( E&M) code for the visit.
Is CPT code 96127 preventive?
Service 96127 is not a preventive service. It is can be billed by specialist only (regarding credentialing list).
Who can bill for CPT code 96127?
Who can bill CPT code 96127? Screening and assessment has to be completed under an MD supervision, and a MD needs to file the report. It means that, for example, primary care physicians can also bill it – not only psychiatrists.
What modifier do you use for 96127?
modifier 59Most insurances require modifier 59 when using CPT code 96127. Please check with each insurance provider for specific guidelines. Under certain circumstances, a physician may need to indicate that a procedure or service was distinct or independent from other services performed on the same day.
Does Medicare pay for CPT 96127?
Many major health insurance companies reimburse for CPT code 96127, including Aetna, Cigna, Medicare, and United Health Care.
How do you use CPT code 96127?
CPT Code 96127 may be used to report behavioral assessments in children and adolescents.
What is the CPT code for anxiety?
ICD-9 Code Transition: 300.02 Code F41. 1 is the diagnosis code used for Generalized Anxiety Disorder.
Is CPT code 96127 time based?
96127 Time Length There is no designated time length for CPT code 96127. Each assessment and subsequent scoring will vary in length. (Source) As noted in the description of this procedure code, these assessments are often brief with multiple units (up to 4 per session) being used per visit.
Do you need modifier 25 with 96127?
4) Preventive visit and screening questionnaire (96127, 96110) would not need a 25 because no NCCI edit. Same for a sick visit.
Can you bill depression screening with annual wellness visit?
Depression Screening This screening can be performed annually, but it cannot be billed when performed with the initial AWV.
Can a nurse practitioner Bill 96127?
No. LPCs, LSWs, etc cannot bill 96127 because the CPT codes used for their services already include uncovering or monitoring mental health conditions.
Does Unitedhealthcare cover 96127?
What codes apply? 14 A: Yes, the preventive care services benefit includes coverage for screening for depression in all adults, including maternal depression screenings, when billed in accordance with the coding in the Screening for Depression in Adults row listed in this guideline (when billed with code 96127 and Z13.
What is the difference between 96160 and 96127?
Codes 96110, 96160, and 96161 are typically limited to developmental screening and the health risk assessment (HRA). However, code 96127 should be reported for both screening and follow-up of emotional and behavioral health conditions.
What is the 96127 CPT code?
The 96127 CPT Code has been getting serious attention from professionals who are looking to maximize their services / revenue with screening or assessment services. This specialized code has been approved by the Center for Medicare and Medicaid Services Administration (CMS) since 2015 (search for “92167” on page 14 of this CMS document ). Fees associated with the 96127 CPT code can be almost $25 per administration and are billable up to four times per year. A variety of sources are now offering tools for behavioral health professionals to quickly and easily be implementing such a service, and billing automatically. One such service offered by an affiliate of TBHI is Mentegram, automated practice management and patient engagement platform that offers clinicians a wide range of tools and services to expedite the routine communication needs of practice to focus on patient care.
Can a CPT code be billed on the same date?
Unlike many other psychological tests, the 96127 CPT Code can be billed on the same date of service as other common services such as psychiatry or therapy appointments.
When to use CPT 96127?
Primary care and other specialists may use CPT code 96127 when screening and assessing their patients, up to four times per year per patient.
What modifier is used for 96127?
Most payers may require that modifier 59 is appended to the screening code. If multiple screenings are performed on a date of service CPT 96127 should be reported with the number of test as the number of Units. NOTE: Modifier 25 should be appended to the E/M and modifier 59 should be appended to the 96127 CPT code.
What is the CPT code for emotional assessment?
CPT code 96127 (Brief emotional/behavioral assessment) has only been around since early 2015, and has been approved by the Center for Medicare & Medicaid Services (CMS) and is reimbursed by major insurance companies, such as Aetna, Anthem, Cigna, Humana, United Healthcare, Medicare and others.
What is modifier 59?
Modifier 59 is used to identify procedures/services that are not normally reported together, but are appropriate under the circumstances. This may represent a different session or patient encounter, different procedure or surgery, different site or organ system, separate incision/excision, separate lesion, or separate injury (or area of injury in extensive injuries) not ordinarily encountered or performed on the same day by the same physician.
Does CPT 96127 include scoring?
Since CPT code 96127 includes scoring and documentation of the test, you would need to report the date that the testing conclude d . The provider does not need to be the one to administer the assessment, since the code description also references scoring and documenting the result. The provider reporting the service should be ...
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Social Security Act 1861 (s) Medical And Other Health Services Social Security Act 1862 (a) (7) does not extend coverage to screening procedures. 42 CFR (Code of Federal Regulations):
Article Guidance
The billing and coding information in this article is dependent on the coverage indications, limitations and/or medical necessity described in the associated LCD L34646 Psychological and Neuropsychological Testing.
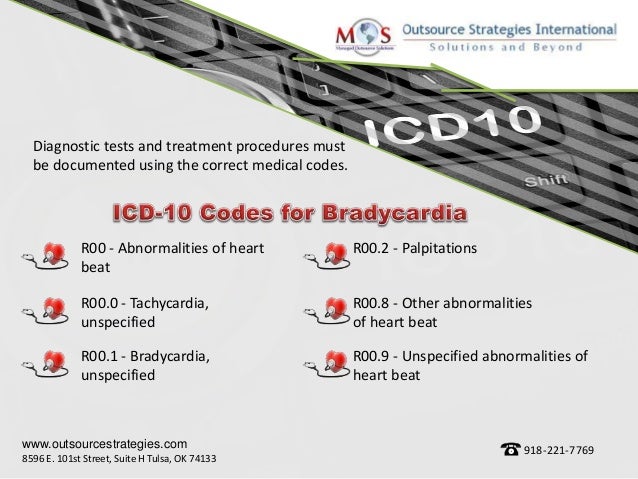
ICD-10-CM Codes that Support Medical Necessity
There are no ICD-10 codes listed in this Article because coverage of the service is not based on diagnosis. Providers should use the appropriate ICD-10 code.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
Popular Posts:
- 1. icd 10 code for sciatica complicating pregnancy
- 2. icd 10 code for fall and hit
- 3. icd 10 code for sprain left lower back
- 4. icd 10 code for rapid weight losee
- 5. icd 10 code for sudden onset headache
- 6. tri-luma icd-10 code for dark areas
- 7. icd 10 code for hypertension s p renal disease
- 8. what is the icd 10 code for spinal stenosis
- 9. what is the icd 10 code for scarring of nerve of foot
- 10. icd 10 code for spotting in pregnancy