How to treat infected diabetic foot ulcer?
To be extra careful, we suggest the preventable measures below:
- Take care of any cuts or wounds early before it gets infected
- Wash your feet every other day
- Keep feet dry and moisturized
- Keep toenails trimmed and keep good hygiene
- Change socks everyday
- Wear comfortable shoes
- Never walk barefoot outside
- Avoid alcohol and tobacco use
What is debridement of foot ulcer?
Preparation may include:
- physical exam
- measurement of wound
- pain medication (mechanical debridement)
- local or general anesthesia (sharp debridement)
What is treatment for infected ulcers?
Treatment
- Treatment team
- Reducing pressure. The first step in treating a bedsore is reducing the pressure and friction that caused it. ...
- Cleaning and dressing wounds. Care for pressure ulcers depends on how deep the wound is. ...
- Removing damaged tissue. To heal properly, wounds need to be free of damaged, dead or infected tissue. ...
- Other interventions. ...
- Surgery. ...
How do you treat a diabetic foot ulcer?
What can I do to prevent diabetic foot ulcers?
- Keep your blood sugar levels under control. Continue the plan for your diabetes that you and your healthcare provider have discussed. ...
- Protect your feet. Do not walk barefoot or wear your shoes without socks. ...
- Do not smoke. Nicotine can damage your blood vessels and increase your risk for foot ulcers. ...
- Maintain a healthy weight. ...
What is the ICD-10 code for foot ulcer?
ICD-10 code L97. 509 for Non-pressure chronic ulcer of other part of unspecified foot with unspecified severity is a medical classification as listed by WHO under the range - Diseases of the skin and subcutaneous tissue .
What is the ICD-10 for diabetic foot ulcer?
ICD-10 code E11. 621 for Type 2 diabetes mellitus with foot ulcer is a medical classification as listed by WHO under the range - Endocrine, nutritional and metabolic diseases .
How do you code a foot ulcer?
Of these options, the most commonly used codes for diabetic foot ulcers are E10. 621 (Type 1 diabetes mellitus with foot ulcer) and E11. 621 (Type 2 diabetes mellitus with foot ulcer).
What is the ICD-10 code for ulcer left foot?
ICD-10 Code for Non-pressure chronic ulcer of other part of left foot with unspecified severity- L97. 529- Codify by AAPC.
What is ICD-10 code for diabetic wound infection?
Type 2 diabetes mellitus with other skin ulcer The 2022 edition of ICD-10-CM E11. 622 became effective on October 1, 2021.
Is diabetic foot ulcer a pressure ulcer?
Diabetic ulcers may look similar to pressure ulcers; however, it is important to note that they are not the same thing. As the name may imply, diabetic ulcers arise on individuals who have diabetes, and the foot is one of the most common areas affected by these skin sores.
How do you code a non-pressure ulcer?
Non-pressure chronic ulcers are similar to pressure ulcers in that they require documentation of the site, severity and laterality. Category L97 and L98 are for non-pressure ulcers, and have an instructional note to code first any associated underlying condition, such as: Associated gangrene.
What is an ulcer on the foot?
Foot ulcers are open sores or lesions that will not heal or that return over a long period of time. These sores result from the breakdown of the skin and tissues of the feet and ankles and can get infected. Symptoms of foot ulcers can include swelling, burning, and pain.
What is the ICD-10 code for foot infection?
X7 for Direct infection of ankle and foot in infectious and parasitic diseases classified elsewhere is a medical classification as listed by WHO under the range - Arthropathies .
What is the difference between a pressure ulcer and a non-pressure ulcer?
The term “non-pressure ulcer” was coined to designate a primary mechanism other than shear or pressure. If there is poor circulation, such as that caused by venous or arterial insufficiency or excessive moisture or trauma, a patient may develop a non-pressure ulcer.
What is the ICD 10 code for arterial ulcer?
ICD-10-CM Code for Atherosclerosis of native arteries of other extremities with ulceration I70. 25.
What is the ICD 10 code for venous stasis ulcer?
The stasis ulcer caused by venous insufficiency is captured first with the code for underlying disease (459.81) followed by the code for the location of the ulcer (707.13).
What is the difference between a pressure ulcer and a non pressure ulcer?
The term “non-pressure ulcer” was coined to designate a primary mechanism other than shear or pressure. If there is poor circulation, such as that caused by venous or arterial insufficiency or excessive moisture or trauma, a patient may develop a non-pressure ulcer.
What is the ICD-10 code for arterial ulcer?
ICD-10-CM Code for Atherosclerosis of native arteries of other extremities with ulceration I70. 25.
How do you code a diabetic foot infection?
Wiki Diabetic foot infection???Code: E11.621.Code Name: ICD-10 Code for Type 2 diabetes mellitus with foot ulcer.Block: Diabetes mellitus (E08-E13)Details: Type 2 diabetes mellitus with foot ulcer. ... Excludes1: diabetes mellitus due to underlying condition (E08.-)More items...•
What is diabetic foot ulcer?
A diabetic foot ulcer is an open sore or wound that occurs in approximately 15 percent of patients with diabetes, and is commonly located on the bottom of the foot. Of those who develop a foot ulcer, six percent will be hospitalized due to infection or other ulcer-related complication.
What causes diabetic foot ulcers?
A “diabetic foot ulcer,” which is caused exclusively by hyperglycemia, in the absence of neuropathy or ischemia, is a rarity. That term almost always refers to an ulcer on the foot of a diabetic that derives from neuro/ischemic etiology, as opposed to being strictly and principally due to pressure injury.
Why do diabetics get ulcers on their feet?
The American Podiatric Medical Association adds that “ (diabetic foot) ulcers form due to a combination of factors, such as lack of feeling in the foot, poor circulation, foot deformities, irritation (such as friction or pressure), and trauma, as well as duration of diabetes.” They go on to note that “vascular disease can complicate a foot ulcer, reducing the body’s ability to heal and increasing the risk for an infection.”
What is a malum perforans pedis ulcer?
Neuropathy results in malum perforans pedis (a.k.a. bad perforating foot) ulcers. These are painless, non-necrotic, circular lesions circumscribed by hyperkeratosis. They often overlie a metatarsal head. Ischemic wounds manifest local signs of ischemia such as thin, shiny, hairless skin with pallor and coldness. These are often found at areas of friction and may be painful.
Why are pressure ulcers considered a patient safety indicator?
Pressure ulcers are deemed patient safety indicators and hospital acquired conditions because a concerted program for prevention and treatment can prevent them and protect our patients from iatrogenic harm. The diagnosis of a “pressure ulcer” may trigger prevalence and incident reporting.
What is the most common site of ulceration?
The plantar surface is the most common site of ulceration, especially at areas of bony prominence.”.
Why should we specifically carve out pressure ulcers?
Why should we specifically carve out pressure ulcers? Pressure ulcers are deemed patient safety indicators and hospital acquired conditions because a concerted program for prevention and treatment can prevent them and protect our patients from iatrogenic harm. The diagnosis of a “pressure ulcer” may trigger prevalence and incident reporting.
What is non pressure ulcer?
The term “non-pressure ulcer” was coined to designate a primary mechanism other than shear or pressure. If there is poor circulation, such as that caused by venous or arterial insufficiency or excessive moisture or trauma, a patient may develop a non-pressure ulcer.
Convert E11621 To Icd
The General Equivalency Mapping crosswalk indicates an approximate mapping between the ICD-10 code E11.621 its ICD-9 equivalent. The approximate mapping means there is not an exact match between the ICD-10 code and the ICD-9 code and the mapped code is not a precise representation of the original code.
What Are The Symptoms Of Type 2 Diabetes
Many people with type 2 diabetes have no symptoms at all. If you do have them, the symptoms develop slowly over several years. They might be so mild that you do not notice them. The symptoms can include
Type 2 Diabetes Mellitus With Foot Ulcer
E11.621 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
Counts And Classification Of Patients With Diabetic Foot Infections
We identified 61,007 patients with one or more specific or moderately-specific codes for diabetic foot infection in inpatient records. Of these, 42,063 had specific codes that were classifiable into one of our predefined groups.
Statistical Methods Of The Study
Statistical data processing was performed using SPSS statistical software version 22.0. The calculation and construction of diagrams reflecting the dynamics of the studied indicators were carried out with the support of Open Office Apache 4. All digital data were processed via variation statistics using Students t-test.
Outcomes Of Patients With Diabetic Foot Infections
Using ICD-9-CM codes and our classification system, we determined: 1) The proportion of patients who were rehospitalized for any type of foot infection 2) The type of foot infection that was present and, 3) The number of days between admissions.
Characteristics Of The Classification Developed And Used In The Study Of Diabetic Foot Syndrome
We have developed a classification of diabetic foot syndrome that can be introduced into the ICD-10 and the ICD-11 under development.
How wide is the unroofed area of the foot?
There was a small amount of bleeding from the tissues. The area unroofed on the plantar surface of the foot included approximately 4 to 5 mm wide from the first to the third metatarsals and extending all the way from the mid foot all the way to the toes. This area, after thorough debridement, was packed open with gauze.
What is the procedure for a left foot abscess?
Name of Procedure: 1. Debridement skin, subqu tissues and muscle over the the medial aspect of the left foot, over the MTP joint. 2. I&D abscess on the plantar surface of the foot extending between the first and second toes, and extending to the dorsum of the foot, with debridement of skin, subqu tissues and muscles on the plantar surface ...
What is the size of a wound after debridement?
Curette was used to debride the wound to the level of capsule. All nonviable tissue was removed. The size of the wound debrided was 0.3 cm x 2.2 cm x 1.0 cm. The appearance of the wound after debridement was clean bleeding base. There was negligible blood loss and any active bleeding during the procedure was controlled by compression. The wound was dressed with compression dressing.
Can I and D be coded separately?
If the I & D is on a seperate area from where the debridement took place ( a different part of the foot) it can be coded seperatly.

Terminology
Diagnosis
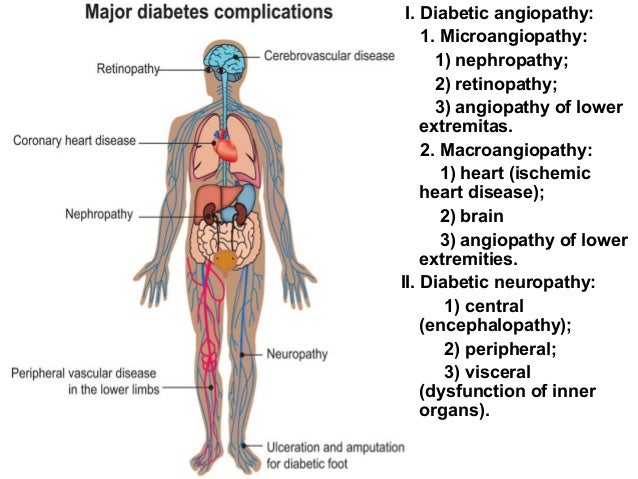
- There are medical diagnoses that predispose patients to develop secondary conditions. Diabetes mellitus is a pervasive endocrinopathy whereby hyperglycemia affects every organ and system in the body, including the nerves and blood vessels. It makes a patient more prone to infection and poor healing. Diabetics are prone to foot ulcers, often with contributions from neuropathic, ische…
Clinical significance
- Diabetics also often have diseases of both large and small arteries. Poorly controlled blood sugars weaken the small blood vessel walls and predispose patients to arteriosclerosis. This impairs the circulation and causes ischemia of the soft tissues, especially of the lower extremities.
Causes
- Heel ulcers, however, are usually a consequence of a pressure injury, although it is also possible to have another mechanism cause a non-pressure injury involving the heel. Diabetes may accelerate or complicate the injury. The American Podiatric Medical Association adds that (diabetic foot) ulcers form due to a combination of factors, such as lack of feeling in the foot, po…
Signs and symptoms
- Neuropathy results in malum perforans pedis (a.k.a. bad perforating foot) ulcers. These are painless, non-necrotic, circular lesions circumscribed by hyperkeratosis. They often overlie a metatarsal head. Ischemic wounds manifest local signs of ischemia such as thin, shiny, hairless skin with pallor and coldness. These are often found at areas of friction and may be painful.
Epidemiology
- The American Orthopaedic Foot & Ankle Society states that ulceration is an extremely common complication in diabetic patients (up to 12 percent of the population). The plantar surface is the most common site of ulceration, especially at areas of bony prominence. The Society also points out that the presence of neuropathy is the key factor in development of diabetic ulceration.
Society and culture
- In the podiatric literature, NPUAP is often referenced as having given guidance to use diabetic foot ulcer for any ulcer on the foot of a diabetic, even if arterial disease and/or pressure played a role in its development. I think this is simplistic and derived from literature not aimed at physicians/APPs. It is common in the literature to see the term diabetic foot ulcer used for all-co…
Treatment
- Ultimately, the clinical concern is to treat the lesion appropriately, regardless of the name attached to it. The treatment for both pressure ulcers and diabetic foot ulcers includes offloading (i.e., pressure mitigation, often by means of padding, shoe modifications, contact casts, boots, or non-weight-bearing strategies). Any non-healing wound should be assessed for neuropathy and …
Popular Posts:
- 1. 2017 icd 10 code for injury left toes
- 2. icd 10 code for allergy to bees
- 3. icd 10 code for slipped in shower
- 4. icd 10 code for levoconvex scoliosis
- 5. icd 10 code for lafb
- 6. icd 10 code for mmr titers
- 7. 2020 icd 10 code for right knee pain
- 8. medicare icd 10 code for vitamin d
- 9. icd 10 code for left ankle joint effusion
- 10. icd 9 code for non cardiac chest pain