What is the ICD 10 code for lumbar degeneration?
Other intervertebral disc degeneration, lumbar region. M51.36 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
What is the ICD 10 code for pyogenic discitis of lumbar spine?
Pyogenic disc inflammation of lumbar spine; Pyogenic discitis of lumbar spine; Pyogenic infection of lumbar intervertebral disc ICD-10-CM Diagnosis Code M51.06 [convert to ICD-9-CM] Intervertebral disc disorders with myelopathy, lumbar region
What is the correct ICD-10 code for disc disorders?
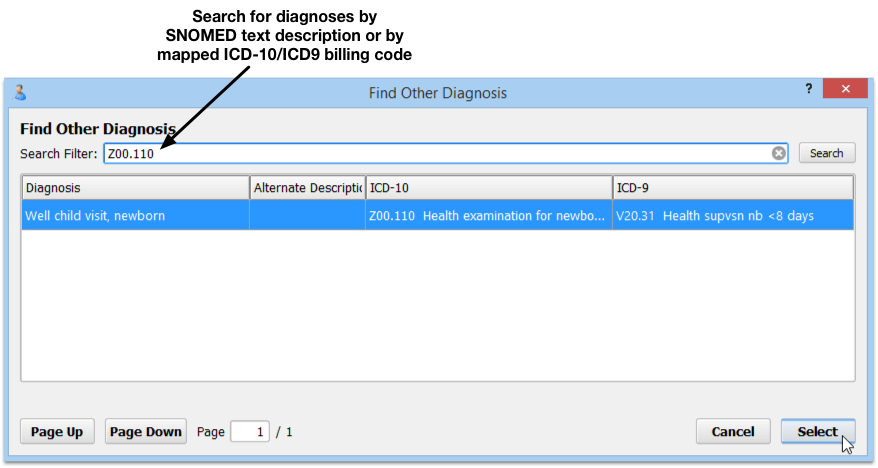
Selecting the correct ICD-10 code for disc disorders can take a little bit of research. There are many options found in the M50 and M51 categories, which are: M51- Thoracic, Thoracolumbar, and Lumbosacral Intervertebral Disc Disorders The fifth character provides detail about the anatomical location within the spinal region.
What is the CPT code for intervertebral disc degeneration?
Other intervertebral disc degeneration, lumbar region. M51.36 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2021 edition of ICD-10-CM M51.36 became effective on October 1, 2020.
What is the ICD-10 code for DDD lumbar?
M51. 36 - Other intervertebral disc degeneration, lumbar region. ICD-10-CM.
What is the ICD code for DDD?
722.52 is the accurate diagnosis code for DDD of the lumbar or lumbosacral intervertebral disc. Other terms used to describe DDD are disc desiccation and discogenic spondylosis. It also can be commonly described as an aggravation of a pre-existing condition of DDD.
What is the ICD-10 code for degenerative changes of the lumbar spine?
M51. 36 Other intervertebral disc degeneration, lumbar region - ICD-10-CM Diagnosis Codes.
What does DDD of the spine mean?
Degenerative disc disease isn't actually a disease, but rather a condition in which a damaged disc causes pain. This pain can range from nagging to disabling. The condition can be caused by the drying out of the disc over time, daily activities, sports and injuries.
Is DDD same as DJD?
Degenerative disc disease or DDD can be the cause of many different symptoms resulting in localized pain or pain that radiates down the leg. Degenerative joint disease or DJD is very different, but can have overlapping symptoms with DDD.
Is DDD the same as osteoarthritis?
Degenerative joint disease is just another name for osteoarthritis, which is the most common type of arthritis – and it occurs when the components of a joint wear down. So whether we call it degenerative joint disease, osteoarthritis, or arthritis, we're really talking about the same condition.
What is the ICD-10 code for degenerative changes?
According to Coding Clinic: “Assign code M16. 0—Bilateral primary osteoarthritis of hip for degenerative changes of hips”. Coding Clinic's rationale is, “ICD-10- CM's Alphabetic Index under “Degeneration, joint disease” instructs “see Osteoarthritis.”
What does diagnosis code m54 9 mean?
9: Dorsalgia, unspecified.
What is the difference between Ivds and DDD?
Intervertebral disk (IVD) degeneration is a natural progression of the aging process. Degenerative disk disease (DDD) is a pathologic condition associated with IVD that has been associated with chronic back pain.
What is severe degenerative disc disease L5 S1?
The L5-S1 situated at the bottom of the vertebral column is typically subject to excessive biomechanical stress, leading to more loads and an increased risk of injury. Common problems include: Disc problems. Lower back disc herniation typically occurs at the L5-S1 level.
What is degenerative disc disease at L4 L5?
DISC DEGENRATIVE DISEASE L4-L5 CAUSES Tiny tears or cracks in the outer layer of the disc – Pressure on the outer layer of a disc can result in the development of small tears. The jellylike material from inside the disc can then seep through these cracks – a condition known as a herniated disc.
What is ICD-10 code for multilevel degenerative disc disease?
Other intervertebral disc degeneration, lumbar region M51. 36 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM M51. 36 became effective on October 1, 2021.
What is the ICD-10 code for chronic back pain?
ICD-10 Code M54. 5 for Chronic Low Back Pain | CareCloud.
What is the ICD-10 code for disc space narrowing?
Intervertebral disc stenosis of neural canal of lumbar region. M99. 53 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM M99.
What is the ICD-10 code for lumbar disc herniation with radiculopathy?
ICD-10 Code for Intervertebral disc disorders with radiculopathy, lumbar region- M51. 16- Codify by AAPC.
What is the T12-L1 code?
Though it is not specifically mentioned, “thoracolumbar” likely only includes T12-L1, and “lumbosacral” probably only refers to the L5-S1 interspace. There is a strange rule for cervical disc disorders indicating that you should code to the most superior level of the disorder.
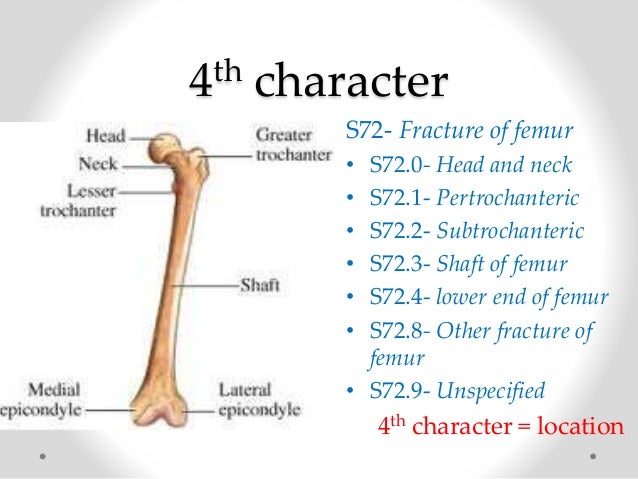
What character is used for disc disorders?
Only use the fourth character “9” for unspecified disc disorders if the documentation does not indicate anything more than the presence of a disc problem. But beware, payors are expected to ask for clarification if unspecified or “NOS” codes are used.
What is the 5th character of a disc?
9 = unspecified disc disorder. The fifth character provides detail about the anatomical location within the spinal region. A basic knowledge of spinal anatomy should make fifth-character selection easy, but only if it is documented properly. This includes transitionary regions.
Can a spinal disc be coded?
These spinal disc codes appear to be a bit complex, but with some study and evaluation, the logic used to create them becomes clear. The provider can use the codes to guide proper documentation and the coder then can select the right codes with confidence.
Is sciatica a code for lumbar radiculopathy?
It is already included in the code. Likewise, don’t code sciatica (M54.3-) if you code for lumbar disc with radiculopathy. It would be redundant. On a side note, lumbar radiculopathy (M54.16) might be used if pain is not yet known to be due a disc, but it radiates from the lumbar spine.
Popular Posts:
- 1. icd-10-cm code for post status left mastectomy
- 2. icd 10 code for pustular psoriasis
- 3. icd 10 code for right ankle pain
- 4. icd 9 code for poikiloderma of civatte
- 5. icd 10 code for ckd4
- 6. icd 10 code for cystitis due to radiation
- 7. 2019 icd 10 code for elevated psa
- 8. icd 10 code for foreign body right foot
- 9. icd 10 code for tina capitis
- 10. icd 10 code for encounter for titers