How to cure degenerative disc disease naturally?
Natural Treatments For Degenerative Disc Disease
- Apply Hot Or Cold Packs For Pain Relief. Applying hot or cold packs can ease pain linked to degenerative disc disease. ...
- Correct Your Posture. Poor posture can stress your spinal discs and lead to joint compression and muscular fatigue. ...
- Lose Weight If You’re Overweight. ...
- Exercise. ...
- Practice Yoga. ...
- Consume Fish Oil. ...
- Have Boswellia. ...
- Drink Ginger Tea. ...
What to know about degenerative disc disease?
What increases my risk for degenerative disc disease?
- A previous herniated disc or spinal injury
- A job that requires heavy, physical work
- Obesity
- Inherited genes
- Smoking
What does it mean to have degenerative disc disease?
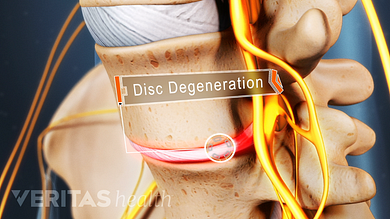
Degenerative disc disease, or DDD, is pain stemming from a degenerated disc in the spine. With continued disc degeneration, the inflammatory proteins within the disc will burn out, and the disc will have a hard time moving on the micro-level, which can cause intense pain.
Is degenerative disc disease the same thing as arthritis?
What is degenerative disc disease? ... Arthritis in the low back has similar symptoms and can cause pain in the back and sometimes into the buttocks. Sometimes the pain can radiate into the thighs, and if it does then it could indicate involvement of the nerves. ... The guidelines for symptoms of tingling, numbness and weakness are the same in ...

What is the ICD-10 code for lumbar disc degeneration?
M51. 36 Other intervertebral disc degeneration, lumbar region - ICD-10-CM Diagnosis Codes.
What is degeneration of L4 and L5?
The L4-L5 disc is at a high risk of degeneration. This risk may be due to increased loads at the L4-L5 motion segment and decreased movement in the segments below this level. A change in disc height due to degeneration may affect the lordosis of the lumbar spine.
What is the ICD-10 code for degenerative changes?
According to Coding Clinic: “Assign code M16. 0—Bilateral primary osteoarthritis of hip for degenerative changes of hips”. Coding Clinic's rationale is, “ICD-10- CM's Alphabetic Index under “Degeneration, joint disease” instructs “see Osteoarthritis.”
What is the CPT code for degenerative disc disease?
722.4 is the correct code for degenerative disease of the cervical intervertebral disc.
What is the ICD 10 code for degenerative disc disease?
ICD-10 code M51. 36 for Other intervertebral disc degeneration, lumbar region is a medical classification as listed by WHO under the range - Dorsopathies .
What causes L4-L5 disc degeneration?
Lumbar disc disease is due to a change in the structure of the normal disc. Most of the time, disc disease comes as a result of aging and the degeneration that occurs within the disc. Occasionally, severe trauma can cause a normal disc to herniate. Trauma may also cause an already herniated disc to worsen.
Is degenerative disc disease a diagnosis?
How is degenerative disc disease diagnosed? A diagnosis is based on a medical history and a physical examination, as well as the symptoms and the circumstances where the pain started. Magnetic resonance imaging can show damage to discs, but it alone cannot confirm degenerative disc disease.
What is the ICD-10 code for G31 9?
ICD-10 code: G31. 9 Degenerative disease of nervous system, unspecified.
What is the ICD-10 code for chronic back pain?
ICD-10 Code M54. 5 for Chronic Low Back Pain | CareCloud.
Is Degenerative Disc Disease the same as osteoarthritis?
However, degenerative disc disease and osteoarthritis are different conditions and can occur separately: one can have degenerative discs without any facet osteoarthritis; or one can have facet osteoarthritis without degenerative discs.
What does lumbar DDD mean?
Degenerative disc disease, or DDD, indicates that the intervertebral disc has undergone degenerative, wear-and-tear (arthritic) changes, which may or may not lead to significant spinal problems. These degenerative changes may occur alone or in combination with other lumbar disorders such as a herniated disc.
What is the T12-L1 code?
Though it is not specifically mentioned, “thoracolumbar” likely only includes T12-L1, and “lumbosacral” probably only refers to the L5-S1 interspace. There is a strange rule for cervical disc disorders indicating that you should code to the most superior level of the disorder.
Is sciatica a code for lumbar radiculopathy?
It is already included in the code. Likewise, don’t code sciatica (M54.3-) if you code for lumbar disc with radiculopathy. It would be redundant. On a side note, lumbar radiculopathy (M54.16) might be used if pain is not yet known to be due a disc, but it radiates from the lumbar spine.
Popular Posts:
- 1. icd 10 code for postpartum dilation and curettage
- 2. icd-10 code for irregular menstruation
- 3. icd-10-cm 2016 code for stapacocol pneumonia
- 4. icd 10 code for deep abscess inguinal
- 5. icd 10 code for mural thrombus
- 6. icd 10 code for gastric sleeve
- 7. icd 10 code for cellulitis on chest
- 8. icd 10 code for waiting for kidney transplant
- 9. icd 10 code for history leg dvt
- 10. icd 10 code for history of recurrent uti