What does ICD 10 do you use for EKG screening?
The specific amount you’ll owe may depend on several things, like:
- Other insurance you may have
- How much your doctor charges
- Whether your doctor accepts assignment
- The type of facility
- Where you get your test, item, or service
What is the diagnosis code for drug screening?
Z51. 81 is a billable ICD code used to specify a diagnosis of encounter for therapeutic drug level monitoring. Furthermore, what is the CPT code for urine drug screen?
Does a 10 panel drug test detect alcohol?
The 10-panel drug test screens for these substances because they’re among the most commonly misused drugs in the United States. The 10-panel drug test doesn’t screen for alcohol. Employers can test...
What is the ICD 10 code for urine drug screen?
- Blanket Orders
- Reflex definitive UDT is not reasonable and necessary when presumptive testing is performed at point of care because the clinician may have sufficient information to manage the patient. ...
- Routine standing orders for all patients in a physician’s practice are not reasonable and necessary.
How do you code a urine drug screen?
In order to match our testing method that is currently being performed, urine drug screen analysis will be billed using CPT code 80101 for each drug class.
What is ICD-10 code for positive urine drug screen?
ICD-10 code R82. 5 for Elevated urine levels of drugs, medicaments and biological substances is a medical classification as listed by WHO under the range - Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified .
What is the code for a drug test?
CPT code 80305: Drug tests(s), presumptive, any number of drug classes; any number of devices or procedures, (e.g. immunoassay) capable of being read by direct optical observation only (e.g., dipsticks, cups, cards, cartridges), includes sample validation when performed, per date of service.
What is the ICD-10 code 80307?
CPT® 80307, Under Presumptive Drug Class Screening Procedures. The Current Procedural Terminology (CPT®) code 80307 as maintained by American Medical Association, is a medical procedural code under the range - Presumptive Drug Class Screening Procedures.
What is a urine tox screen?
A toxicology test ("tox screen") checks for drugs or other chemicals in your blood, urine, or saliva. Drugs can be swallowed, inhaled, injected, or absorbed through the skin or a mucous membrane. In rare cases, a tox screen may check your stomach contents or sweat.
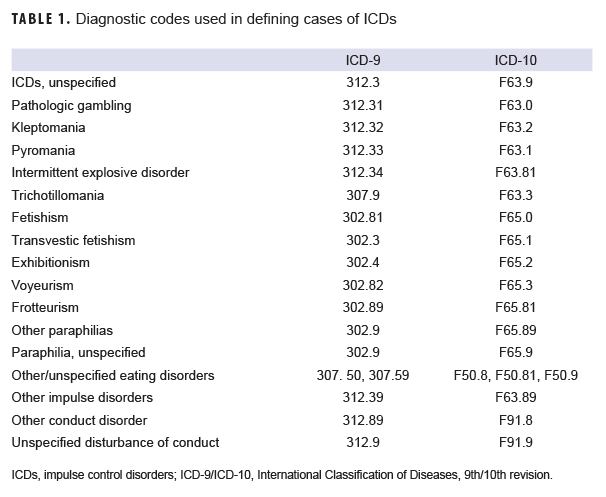
What is the ICD-10 code for substance abuse?
Substance use disorders and ICD-10-CM codingSpecifiers for Substance CodingCode1Abuse.1Uncomplicated.10With intoxication.12...uncomplicated.12064 more rows•Sep 10, 2015
Does Medicare cover urine drug screens?
Medicare also covers clinical laboratory services, including urine drug testing (UDT), under Part B. Physicians use UDT to detect the presence or absence of drugs or to identify specific drugs in urine samples.
What is the difference between 80305 and 80306?
Use 80305 for testing capable of being read by direct optical observation only. Test includes validity testing when performed and may be performed only once per date of service. Use 80306 when test is read by instrument- assisted direct optical observation.
What code is G0483?
• G0483: Drug test(s), definitive, utilizing (1) drug identification methods able to identify individual. drugs and distinguish between structural isomers (but not necessarily stereoisomers), including, but not limited to GC/MS (any type, single or tandem) and LC/MS (any type, single or tandem.
What is presumptive drug testing?
Presumptive drug tests are used to detect the presence or absence of a drug or drug class; they do not typically indicate a specific level of drug but rather give a positive or negative result. A presumptive drug test may be followed with a definitive drug test in order to identify specific drugs or metabolites.
What does CPT 80307 test for?
CPT 80307 is drug screening on a chemistry analyzer. Each code is only reported once per date of service regardless of the number of drugs tested. The codes include sample validation testing such as pH, specific gravity, nitrites, etc.
What is code F12?
ICD-10 code F12 for Cannabis related disorders is a medical classification as listed by WHO under the range - Mental, Behavioral and Neurodevelopmental disorders .
What does CPT code 80307 mean?
CPT code: 80307 Drug test(s), presumptive, any number of drug classes, qualitative; any number of devices or procedures, by instrument chemistry and analyzers (eg, utilizing immunoassay [EIA, ELISA, EMIT, FPIA, IA, KIMS, RIA]), chromatography (eg, GC, HPLC), and mass spectrometry either with or without chromatography, ...
What is procedure code 81001?
81001. Urinalysis, by dip stick or tablet reagent for. bilirubin, glucose, hemoglobin, ketones, leukocytes, nitrite, pH, protein, specific.
What is the CPT code for urine collection?
CPT code 36415 code is used to report routine venipunctures (and for Medicare only, the collection of urine by catheter) Medicare pays a flat rate of $3.00 for HCPCS code 36415 and does not cover CPT capillary blood collection (CPT code 36416).
Can you bill 80307 and G0480 together?
b. Drug confirmation testing is considered included in CPT codes 80305 – 80307 and HCPCS codes G0480 – G0483, G0659, and is not eligible for separate reimbursement.
What is the ICd 10 code for alcohol?
Encounter for blood-alcohol and blood-drug test 1 Z02.83 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. 2 The 2021 edition of ICD-10-CM Z02.83 became effective on October 1, 2020. 3 This is the American ICD-10-CM version of Z02.83 - other international versions of ICD-10 Z02.83 may differ.
What does the title of a manifestation code mean?
In most cases the manifestation codes will have in the code title, "in diseases classified elsewhere.". Codes with this title are a component of the etiology/manifestation convention. The code title indicates that it is a manifestation code.
What is the diagnosis code for drug treatment?
For monitoring of patient compliance in a drug treatment program, use diagnosis code Z03.89 as the primary diagnosis and the specific drug dependence diagnosis as the secondary diagnosis.
What documentation is required for a drug test?
Medical record documentation (e.g., history and physical, progress notes) maintained by the ordering physician/treating physician must indicate the medical necessity for performing a drug test. All tests must be ordered in writing by the treating provider and all drugs/drug classes to be tested must be indicated in the order.
Why do contractors need to specify revenue codes?
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination. Complete absence of all Revenue Codes indicates that coverage is not influenced by Revenue Code and the article should be assumed to apply equally to all Revenue Codes.
How often is a drug test billed?
One definitive drug testing code may be billed once per patient per day as indicated by the code description and should only be billed at one unit regardless of the provider.
What information is needed for a patient's medical record?
Every page of the record must be legible and include appropriate patient identification information (e.g., complete name, dates of service (s)). The record must include the identity of the physician or non-physician practitioner responsible for and providing the care to the patient.
Does LCD apply to acute inpatient claims?
This LCD does not apply to acute inpatient claims.
What is a drug test?
DRUG TEST (S), DEFINITIVE, UTILIZING DRUG IDENTIFICATION METHODS ABLE TO IDENTIFY INDIVIDUAL DRUGS AND DISTINGUISH BETWEEN STRUCTURAL ISOMERS (BUT NOT NECESSARILY STEREOISOMERS), INCLUDING BUT NOT LIMITED TO GC/MS (ANY TYPE, SINGLE OR TANDEM) AND LC/MS (ANY TYPE, SINGLE OR TANDEM), EXCLUDING IMMUNOASSAYS (E.G., IA, EIA, ELISA, EMIT, FPIA) AND ENZYMATIC METHODS (E.G., ALCOHOL DEHYDROGENASE), PERFORMED WITHOUT METHOD OR DRUG-SPECIFIC CALIBRATION, WITHOUT MATRIX-MATCHED QUALITY CONTROL MATERIAL, OR WITHOUT USE OF STABLE ISOTOPE OR OTHER UNIVERSALLY RECOGNIZED INTERNAL STANDARD (S) FOR EACH DRUG, DRUG METABOLITE OR DRUG CLASS PER SPECIMEN; QUALITATIVE OR QUANTITATIVE, ALL SOURCES, INCLUDES SPECIMEN VALIDITY TESTING, PER DAY, ANY NUMBER OF DRUG CLASSES
What happens if you submit a claim without a diagnosis code?
A claim submitted without a valid ICD-10-CM diagnosis code will be returned to the provider as an incomplete claim under Section 1833 (e) of the Social Security Act.
Is CPT a year 2000?
CPT is provided “as is” without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. AMA warrants that due to the nature of CPT, it does not manipulate or process dates, therefore there is no Year 2000 issue with CPT. AMA disclaims responsibility for any errors in CPT that may arise as a result of CPT being used in conjunction with any software and/or hardware system that is not Year 2000 compliant. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon no upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
Can you use CPT in Medicare?
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials of CMS internally within your organization within the United States for the sole use by yourself, employees and agents. Use is limited to use in Medicare, Medicaid or other programs administered by the Centers for Medicare and Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
Why do contractors need to specify revenue codes?
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination. Complete absence of all Revenue Codes indicates that coverage is not influenced by Revenue Code and the article should be assumed to apply equally to all Revenue Codes.
Does CMS have a CDT license?
Organizations who contract with CMS acknowledge that they may have a commercial CDT license with the ADA, and that use of CDT codes as permitted herein for the administration of CMS programs does not extend to any other programs or services the organization may administer and royalties dues for the use of the CDT codes are governed by their commercial license.
Popular Posts:
- 1. icd 9 code for liver transplant
- 2. icd 10 code for sternum fracture
- 3. icd 10 code for moving furniture
- 4. icd 10 code for multiple cat bites unspecified right forearm
- 5. icd 10 cm code for thrombosed external hemorrhoids
- 6. what icd 10 code would you use for someone poked in the eye with a stick
- 7. icd-10 code for phonophobia
- 8. icd 10 code for history of colorectal cancer
- 9. icd-10-cm code for migraine headache
- 10. icd-10 code for gravida 6 para 5 who is seen today at 22 weeks gestation for gestational edema.