What does EGPA stand for?
Eosinophilic granulomatosis with polyangiitis ( EGPA ), also known as allergic granulomatosis, is an extremely rare autoimmune condition that causes inflammation of small and medium-sized blood vessels ( vasculitis) in persons with a history of airway allergic hypersensitivity...
What is the ICD 10 code for granulomatosis with polyangiitis?
This is the American ICD-10-CM version of M30.1 - other international versions of ICD-10 M30.1 may differ. Applicable To. Allergic granulomatous angiitis. Eosinophilic granulomatosis with polyangiitis [EGPA] The following code (s) above M30.1 contain annotation back-references. Annotation Back-References.
How does EGPA affect the body?
Everyone who gets EGPA has a history of asthma and/or allergies. It can affect many of your organs. Almost all people with EGPA have increased numbers of "allergic type" blood cells called eosinophils. Eosinophils are a type of white blood cell that usually make up 5% or less of the total white blood cell count.
What are eosinophils in EGPA?
Eosinophils are a type of white blood cell that usually make up 5% or less of the total white blood cell count. In EGPA, eosinophils usually make up more than 10% of the total white blood cell count. In addition, most biopsies (tissue samples) contain clusters of cells called "granulomas" that may or may not involve blood vessels.
What is EGPA disease?
Overview. Churg-Strauss syndrome is a disorder marked by blood vessel inflammation. This inflammation can restrict blood flow to organs and tissues, sometimes permanently damaging them. This condition is also known as eosinophilic granulomatosis with polyangiitis (EGPA).
Is EGPA a vasculitis?
Eosinophilic granulomatosis with polyangiitis (EGPA) is an extremely rare form of vasculitis, characterized by inflammation within small blood vessels. This inflammation results in blood flow restriction, which can cause organ damage throughout the body if left untreated. EGPA is a serious, but treatable disease.
Is EGPA an autoimmune disease?
The inflamed vessels can affect various organ systems including the lungs, gastrointestinal tract, skin, heart and nervous system. The exact cause of Eosinophilic granulomatosis with polyangiitis is unknown, but it is thought to be an autoimmune disorder.
What is the ICD 10 code for Churg-Strauss syndrome?
ICD-10-CM Code for Polyarteritis with lung involvement [Churg-Strauss] M30. 1.
What is the difference between GPA and EGPA?
Eosinophilic Granulomatosis with Polyangiitis (EGPA) It is similar in nature to Granulomatosis with Polyangiitis (GPA) but the main white blood cell involved in the inflammation is the eosinophil. EGPA is much less common than GPA and EGPA is associated with allergies, asthma and nasal polyps.
How do you diagnose EGPA?
Diagnosis. There is no single test for diagnosing EGPA, so your doctor will consider a number of factors, including a detailed medical history; physical examination; laboratory tests; specialized imaging studies; and, when indicated, a biopsy of an affected tissue or organ.
What are the stages of EGPA?
The 3 phases of EGPAProdromal. Severe asthma (typically adult onset) and allergies.Eosinophilic. Peripheral blood eosinophilia.Vasculitic. Necrotizing vasculitis and granulomas.
Is eosinophilic asthma an autoimmune disorder?
Eosinophilic diseases are not autoimmune diseases; instead, they are like exacerbated allergies or an atypical allergic response to molecules that most people do not find harmful.
Can you live with EGPA?
Overall, without treatment, the 5-year survival rate in EGPA is about 25%. With treatment, the 1-year survival rate is 90% and the 5-year survival rate is 62%. The principal causes of morbidity and mortality in EGPA are myocarditis and myocardial infarction secondary to coronary arteritis.
What is the ICD 10 code for vasculitis?
ICD-10 code L95. 9 for Vasculitis limited to the skin, unspecified is a medical classification as listed by WHO under the range - Diseases of the skin and subcutaneous tissue .
What is the ICD 10 code for granulomatosis with Polyangiitis?
M31. 3 - Wegener's granulomatosis | ICD-10-CM.
What is pulmonary vasculitis?
The term pulmonary vasculitis refers to distinct disorders that are pathologically characterized by the destruction of blood vessels (1). Pulmonary vasculitis may be secondary to other conditions or constitute a primary and in most cases idiopathic disorder.
The ICD code M301 is used to code Churg-Strauss syndrome
Churg–Strauss syndrome (CSS, also known as eosinophilic granulomatosis with polyangiitis [EGPA] or allergic granulomatosis) is an autoimmune condition that causes inflammation of small and medium-sized blood vessels (vasculitis) in persons with a history of airway allergic hypersensitivity (atopy). It usually manifests in three stages.
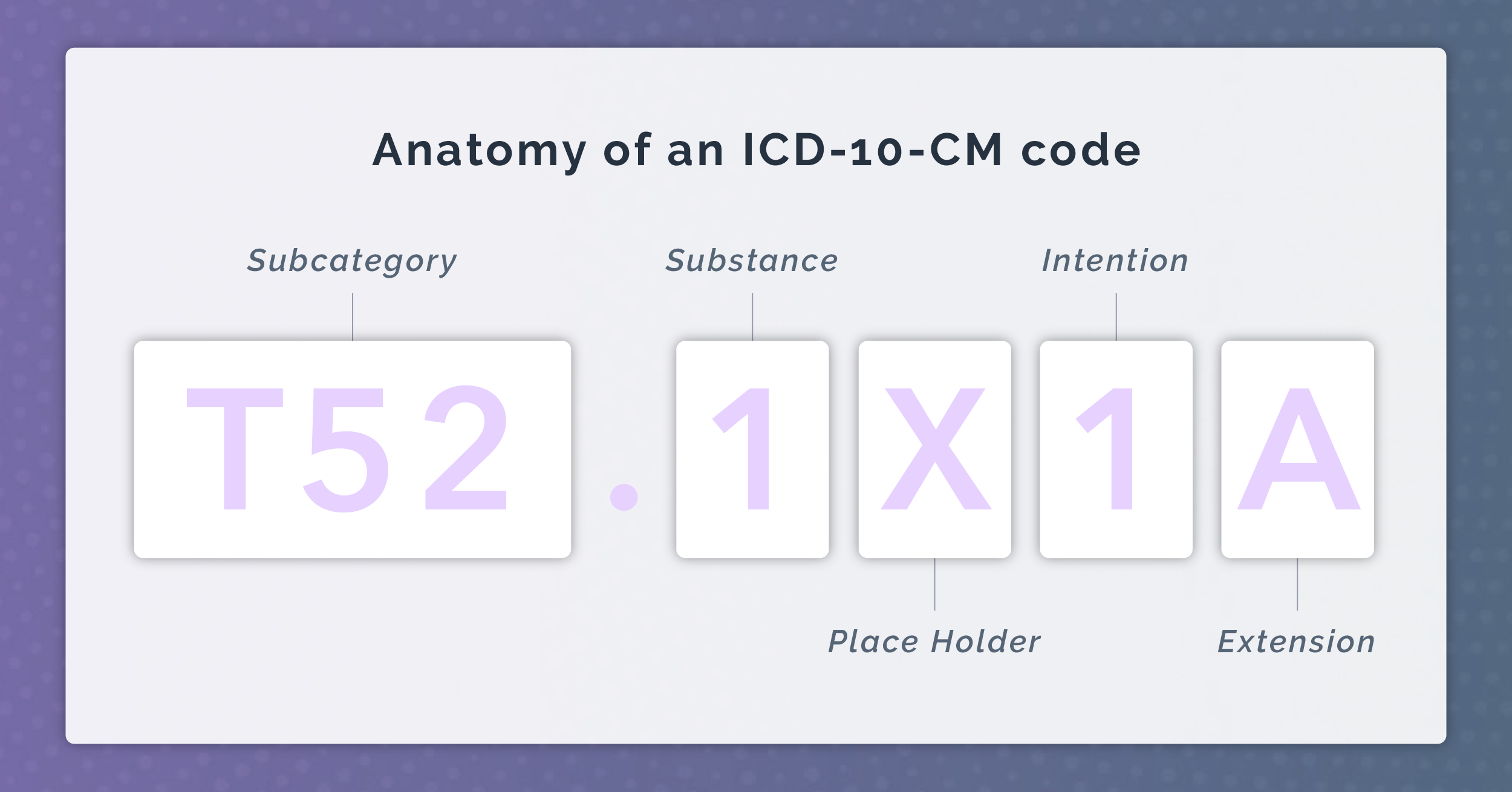
Coding Notes for M30.1 Info for medical coders on how to properly use this ICD-10 code
Inclusion Terms are a list of concepts for which a specific code is used. The list of Inclusion Terms is useful for determining the correct code in some cases, but the list is not necessarily exhaustive.
MS-DRG Mapping
DRG Group #542-544 - Pathological fractures and musculoskelet and connective tissue malig with MCC.
Equivalent ICD-9 Code GENERAL EQUIVALENCE MAPPINGS (GEM)
This is the official approximate match mapping between ICD9 and ICD10, as provided by the General Equivalency mapping crosswalk. This means that while there is no exact mapping between this ICD10 code M30.1 and a single ICD9 code, 446.4 is an approximate match for comparison and conversion purposes.
Clinical description
Onset of eosinophilic granulomatosis with polyangiitis (EGPA) usually occurs in adulthood but may occur anywhere between 15 and 70 years of age. EGPA may involve multiple organ systems. The onset of EGPA is often associated, in patients with preexisting asthma, with worsening of the asthma.
Diagnostic methods
Classification criteria of EGPA include, in the presence of evidence of vasculitis, four of the following six features: asthma, eosinophilia, neuropathy, pulmonary infiltrates, paranasal sinus abnormalities and eosinophilic vasculitis.
Differential diagnosis
Differential diagnoses of EGPA include granulomatosis with polyangiitis, hypereosinophilic syndrome, microscopic polyangiitis, polyarteritis nodosa, drug reactions, bronchocentric granulomatosis, fungal and parasitic infections, and malignancy.
Management and treatment
The treatment of patients with mild disease involves glucocorticoids (GC) monotherapy. Other immunosuppressive regimens, such as those using cyclophosphamide (CP), azathioprine or methotrexate, are used for patients with an aggressive disease.
Prognosis
Cardiac involvement used to be the leading cause of death related to EGPA, followed by cerebral hemorrhage and stroke. GC-related toxicity is also a frequent cause of morbidity and mortality. Despite treatment, neurological sequelae rarely resolve completely.
What is EGPA in medical terms?
Eosinophilic granulomatosis with polyangiitis ( EGPA ), formerly known as allergic granulomatosis, is an extremely rare autoimmune condition that causes inflammation of small and medium-sized blood vessels ( vasculitis) in persons with a history of airway allergic hypersensitivity ( atopy ). It usually manifests in three stages.
What is the third stage of EGPA?
The third and final stage, and hallmark of EGPA, is inflammation of the blood vessels, and the consequent reduction of blood flow to various organs and tissues. Local and systemic symptoms become more widespread and are compounded by new symptoms from the vasculitis. Severe complications may arise.
What are the diagnostic markers for Churg Strauss syndrome?
Diagnostic markers include eosinophil granulocytes and granulomas in affected tissue, and antineutrophil cytoplasmic antibodies (ANCA) against neutrophil granulocytes. The American College of Rheumatology 1990 criteria for diagnosis of Churg–Strauss syndrome lists these criteria:
What is the treatment for eosinophilic granulomatosis with polyangiitis
Treatment. Treatment for eosinophilic granulomatosis with polyangiitis includes glucocorticoids (such as prednisolone) and other immunosuppressive drugs (such as azathioprine and cyclophosphamide ). In many cases, the disease can be put into a type of chemical remission through drug therapy, but the disease is chronic and lifelong.
What is the prodromal stage of asthma?
The early ( prodromal) stage is marked by airway inflammation; almost all patients experience asthma and/or allergic rhinitis. The second stage is characterized by abnormally high numbers of eosinophils ( hypereosinophilia ), which causes tissue damage, most commonly to the lungs and the digestive tract.
Is EGPA a variable condition?
Eosinophilic granulomatosis with polyangiitis consists of three stages, but not all patients develop all three stages or progress from one stage to the next in the same order; whereas some patients may develop severe or life-threatening complications such as gastrointestinal involvement and heart disease, some patients are only mildly affected, e.g. with skin lesions and nasal polyps. EGPA is consequently considered a highly variable condition in terms of its presentation and its course.
How to diagnose EGPA?
The healthcare provider may use the following tests to diagnose EGPA: 1 Medical history: to look for EGPA, especially asthma, allergies and other features of the disease. 2 Physical examination: to discover which organs are involved and to rule out other illnesses that may look similar. 3 Blood tests: to look for abnormal blood counts and an increase in eosinophils and special antibody testing called ANCA. 4 Urinalysis: to detect whether there is too much protein, or red blood cells, in the urine. 5 Imaging tests such as x-rays and computed tomography (CT) to look for any abnormalities in areas such as the lungs or sinuses.
Why does EGPA cause inflammation?
Your immune system plays a role in EGPA. The immune system acts to protect the body against “foreign invaders” (germs, bacteria) that cause infections, disease and other injuries to the body. Sometimes your immune system become s over active and can cause inflammation.
What is eosinophilic granulomatosis with polyangiitis?
What is eosinophilic granulomatosis with polyangiitis (EGPA, formerly Churg-Strauss Syndrome)? Eosinophilic granulomatosis with polyangiitis (EGPA, formerly Churg-Strauss Syndrome) is a disease caused by inflammation (swelling) that occurs in certain types of cells in your blood or in your tissues. Everyone who gets EGPA has a history ...
How long does it take for EGPA to go away?
If cyclophosphamide is used for severe EGPA, it is often only given until you go into remission (usually around three to six months); you’ll then switch to another immunosuppressive agent, such as methotrexate, Mycophenolate Mofetil, azathioprine or Mepolizumab, to maintain remission.
How long does it take to recover from EGPA?
EGPA is a serious illness that can affect a variety of organs but, fortunately, more than 80% survive the symptoms (after five years of illness). Stay in close contact with your healthcare provider and be sure to follow his or her instructions regarding your care.
What tests are used to diagnose EGPA?
The healthcare provider may use the following tests to diagnose EGPA: Medical history: to look for EGPA, especially asthma, allergies and other features of the disease. Physical examination: to discover which organs are involved and to rule out other illnesses that may look similar.
Can EGPA cause numbness?
You may have any combination of these symptoms. Kidney disease caused by EGPA often does not have any symptoms. You may not know about inflammation of the kidney until the kidneys begin to stop working.
Popular Posts:
- 1. icd 10 code for enteric tube status
- 2. icd 10 code for adenocarcinoma of esophagus
- 3. icd 10 dx code for gallbladder disease
- 4. icd 10 code for foul odor to urine
- 5. icd 10 code for mycoplasma igm positive
- 6. icd 10 code for status post left foot tibialis repair
- 7. icd 1 code for pushed out of vehicle
- 8. icd 10 code for status post right shoulder arthroscopy
- 9. icd-10 code for stenotrophomonas maltophilia
- 10. icd 10 code for gastric antral vascular ectasia