What is the purpose of ICD 10?
Encntr for follow-up exam after trtmt for malignant neoplasm; ... ICD-10-CM Diagnosis Code Z30.012. Encounter for prescription of emergency contraception. ... Dining room in other specified residential institution as the place of occurrence of the external cause.
Are You Ready for ICD 10?
Z09 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. Short description: Encntr for f/u exam aft trtmt for cond oth than malig neoplm; The 2022 edition of ICD-10-CM Z09 became effective on October 1, 2021.
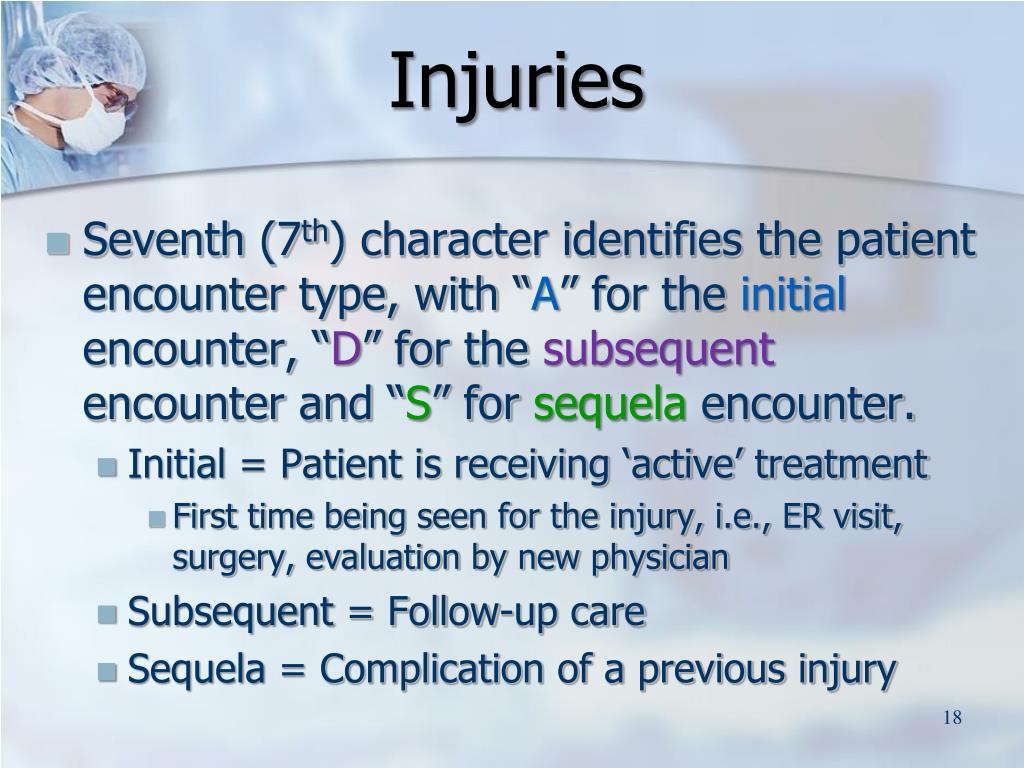
What does subsequent encounter mean in ICD 10?
ICD-10 will require more work on the provider to document the exact type of diagnosis found with the patient. ICD-10 demands documentation of the anatomical area affected and allows for coding of chronic modalities. Under ICD-10-CM, you have the following codes for Otitis Media: H66.9 Otitis media, unspecified
What is the ICD 10 code for follow up?
Aug 18, 2021 · Aftercare and Follow-up: ICD-10 Coding. Aftercare visit codes cover situations in which the initial treatment of a disease has been performed but the patient requires continued care during the healing or recovery phase, or for the long-term consequences of the disease. ICD-10 makes two important points about the use of aftercare codes in the final chapter.
When do you use ICD-10 Z09?
Z09 ICD 10 codes should be used for diseases or disroder other than malignant neoplasm which has been completed treatment.Oct 14, 2020
What is the ICD code for ER visit?
ER claims are defined as claims with CPT codes 99281, 99282, 99283, 99284, and 99285. ICD -9 and ICD -10 standard codes are reported. If multiple diagnostic codes are attached to a claim, primary diagnosis is used. Providers are billing providers.Sep 14, 2017
What is diagnosis Z09?
2022 ICD-10-CM Diagnosis Code Z09: Encounter for follow-up examination after completed treatment for conditions other than malignant neoplasm.
How do you follow-up a code?
Follow-up visits, like initial visits, should be coded using the appropriate evaluation and management (E/M) code (i.e., 99211–99215). Given the limited interaction with the patient and limited work involved, the level of service is likely to be low (e.g., 99211 or 99212).
How do you code an emergency room visit?
A1: Under the OPPS, hospitals report Type A emergency department visits using HCPCS codes 99281-99285. Hospitals report Type B emergency department visits using HCPCS codes G0380-G0384. Hospitals report hospital outpatient clinic visits using HCPCS codes 99201- 99215 and 99241-99245.
What is the most common ER visit?
Ten Common ER VisitsSkin Infections.Back Pain. ... Contusions and Cuts. ... Upper Respiratory Infections. ... Broken Bones and Sprains. ... Toothaches. ... Abdominal Pains. Around 2000 people visit the ER every single day due to abdominal pains. ... Chest Pains. Chest pains are one of the most common reasons why people visit the ER. ... More items...
What is the ICD-10 code for hyperlipidemia?
E78.5ICD-10 | Hyperlipidemia, unspecified (E78. 5)
What is the ICD-10 code for syncope and collapse?
Syncope is in the ICD-10 coding system coded as R55. 9 (syncope and collapse).Nov 4, 2012
What is aftercare code?
Aftercare and Follow-up: ICD-10 Coding 1 The aftercare Z code should not be used if treatment is directed at a current, acute disease. 2 The aftercare Z codes should also not be used for aftercare for injuries.
Can aftercare Z codes be used for injuries?
The aftercare Z codes should also not be used for aftercare for injuries. Certain aftercare Z code categories need a secondary diagnosis code to describe the resolving condition or sequelae. For others, the condition is included in the code title.
What is the ICd 10 for a sprain?
ICD-10-CM supports much more precise anatomic description of the injury or condition. Simply stating “pneumonia” or “ankle sprain” may be inadequate. While many of these descriptors were present in the older system, they are more prominent and enhanced, such as laterality, with ICD-10-CM.
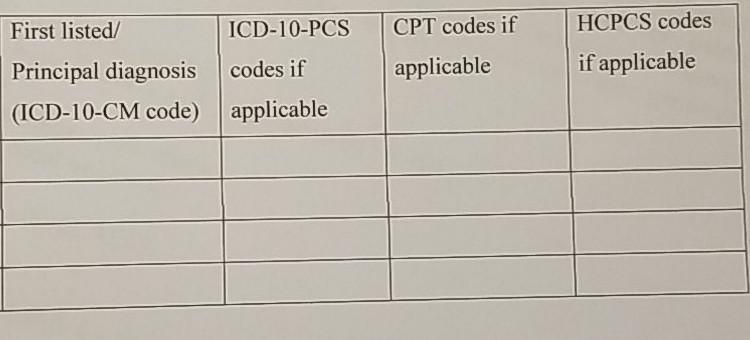
When documenting multiple final diagnoses, the order of your diagnosis is very important.
While there are ICD rules that certain diagnoses should be listed first (principal ), you should list your first (principal) diagnosis as the one which best addresses the primary reason for the patient encounter. Secondary (contributing) conditions that are addressed and provide additional details to support the medical necessity of the encounter are listed AFTER the principal diagnosis. Patients with multiple fractures or injuries, the injury that is most severe should be listed first.
What is severity of illness?
Severity of Illness is a term that indicates the acuity of the pathophysiologic changes that have occurred. It provides a basis for evaluating resource consumption, medical necessity and the patient care provided. Severity of Illness reflects the patient’s level of sickness and disease complications. Sicker patients are more expensive to treat and they utilize more resources, have a higher rate of complications, and have worse outcomes. ICD-10-CM codes allow improved support for documentation of Severity of Illness.
Does ICd 10 require a definitive diagnosis?
ICD-10-CM does not require a “definitive final diagnosis”. Using signs and symptoms such as “chest pain” or “vomiting” as a principal diagnosis is appropriate. You should always strive to document to the highest level of certainty but there will be times when your highest level of clinical certainty results in an “unspecified” diagnosis.
What is the ICD-10 manual for outpatient services?
Those are the guidelines for Diagnostic Coding and Report Guidelines for Outpatient Service. According to that, most facilities – just to give you an idea of what happens in most facilities – if a patient presents to the emergency room, ...
Can you code for a probable diagnosis?
What those guidelines say is if you’re coding for the hospital outpatient department, you do not code for any diagnoses that is documented as “probable,” “suspected,” “questionable,” “rule out,” or “working diagnosis” or anything else that indicate uncertainty; so no “probable,” “likely,” “suspected,” anything like that.
What happens if secondary diagnoses are not reported?
If secondary diagnoses are not reported, then HCC’s are not captured for the claim. This may impact reimbursement and quality measure statistics. Below are several websites that are available and that go into great detail about what HCC’s are, how they are calculated, and why they are important.
Can't describe HCC?
If you can’t describe what HCC’s are, it is recommended that you review some of the websites above and become familiar with these. If you know the why things are reported it is easier to remember to report them. Coders must review the entire outpatient encounter rather than only focusing on the reason for the visit.
What is the final impression by the physician?
The final impression by the physician is COPD exacerbation. In this case, a code for the COPD exacerbation would be reported as well as “Z” codes for personal history of pneumonia, history of smoking, and family history of lung cancer and colon cancer.
Why do you report secondary diagnosis?
Another reason to report all secondary diagnosis, history and status codes is to confirm medical necessity. Some payors will deny tests done outpatient if the medical necessity is not met. Many times medical necessity is determined by the ICD-10-CM codes reported on the outpatient claim. For example, if an EKG is done on a patient in an encounter for outpatient fracture repair, and the chronic atrial fibrillation is not coded as a secondary diagnosis by the coder, the EKG charge/reimbursement could be denied by the payor. There are also many other examples, such as a patient getting extended laboratory tests because they are on long term anticoagulants such as Coumadin. It is very important that all secondary diagnosis/status/history codes be reported on the outpatient claim.
When should chronic conditions be reported?
Chronic conditions should be reported on each visit when they are under treatment or are systemic medical conditions. Chronic systemic conditions should be reported even in the absence of intervention or further evaluation.
Can a code be reported on a radiology report?
Coders may report confirmed diagnoses on radiology and pathology reports (except for incidental findings) “Z” codes help paint the entire health picture for the patient. If there is a specific code for a past or family condition, it will most likely always be reported. Code only confirmed diagnosis on outpatient encounters.
What is a Z09. code?
Z09. Billable codes are sufficient justification for admission to an acute care hospital when used a principal diagnosis. The Center for Medicare & Medicaid Services (CMS) requires medical coders to indicate whether or not a condition was present at the time of admission, in order to properly assign MS-DRG codes.
What is the approximate match between ICd9 and ICd10?
This is the official approximate match mapping between ICD9 and ICD10, as provided by the General Equivalency mapping crosswalk. This means that while there is no exact mapping between this ICD10 code Z09 and a single ICD9 code, V67.9 is an approximate match for comparison and conversion purposes.
Popular Posts:
- 1. icd 10 code for healthy sinusitis
- 2. icd 10 code for metastatic choriocarcinoma
- 3. icd 10 code for patellar disintegration
- 4. icd 10 code for inflammatory arthritis right hip
- 5. icd 9 code for intractable pain
- 6. icd 10 code for status post open reduction internal fixation of right ankle
- 7. icd 10 code for amnesia
- 8. what is the icd 9 code for
- 9. icd 10 code for tendinopathy biceps tendon
- 10. icd 10 code for neuropathy diabetic