What is the ICD 10 code for HIV infection?
2018/2019 ICD-10-CM Diagnosis Code B20. Human immunodeficiency virus [HIV] disease. 2016 2017 2018 2019 Billable/Specific Code. B20 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
What is the ICD 10 code for end stage renal disease?
End stage renal disease. N18.6 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2020 edition of ICD-10-CM N18.6 became effective on October 1, 2019. This is the American ICD-10-CM version of N18.6 - other international versions of ICD-10 N18.6 may differ.
What is the CPT code for HIV with no definitive diagnosis?
Patients with inconclusive HIV serology, and no definitive diagnosis or manifestations of the illness, may be assigned code R75 Inconclusive laboratory evidence of human immunodeficiency virus [HIV]. Known prior diagnosis of an HIV-related illness should be coded to B20.
What is the B20 code for HIV infection?
When a patient is admitted for an HIV-related condition, sequence B20 Human immunodeficiency virus [HIV] disease first, followed by additional diagnosis codes for all reported HIV-related conditions.
What is the difference between B20 and Z21?
Following ICD-10 guidelines, if a patient has or has had an HIV related condition, use B20 AIDS. If the patient has a positive HIV status, without symptoms or related conditions, use Z21.
What does the ICD-10 code B20 mean?
ICD-10 Coding: Diagnosis of B20 (HIV)
What are the 4 stages of AIDS?
Stages of HIV InfectionStages of Infection – (assuming no treatment) ... Stage 1: Infection. ... Stage 2: Asymptomatic. ... Stage 3: Symptomatic. ... Stage 4: AIDS/Progression of HIV to AIDS.
What are the 3 stages of AIDS?
With the advancements in treatment, progression to Stage 3 is less common today than in the early days of HIV.Stage 1: Acute HIV Infection.Stage 2: Chronic HIV Infection.Stage 3: Acquired Immunodeficiency Syndrome (AIDS)
What is ICD-10 code Z21?
ICD-10 code Z21 for Asymptomatic human immunodeficiency virus [HIV] infection status is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
What is code Z71 7?
ICD-10-CM Code for Human immunodeficiency virus [HIV] counseling Z71. 7.
What are the 4 stages of infection?
10.3B: Disease DevelopmentStages of Disease.STAGE 1: INCUBATION PERIOD.STAGE 2: PRODROMAL PERIOD.STAGE 3: ACUTE PERIOD.STAGE 4: CONVALESCENCE PERIOD.
What is the sequence for HIV?
Sequencing. The proper sequencing for HIV depends on the reason for the admission or encounter. When a patient is admitted for an HIV-related condition, sequence B20 Human immunodeficiency virus [HIV] disease first, followed by additional diagnosis codes for all reported HIV-related conditions. Conditions always considered HIV-related include ...
What condition must be confirmed to select the code?
In the inpatient setting, HIV is the only condition that must be confirmed to select the code. All other conditions documented as “probable,” suspected,” likely,” “questionable,” “probable,” or “still to rule out” are coded as if they exist in the inpatient setting. Dx. Sequencing. The proper sequencing for HIV depends on the reason for ...
When to use Z21?
Apply Z21 Asymptomatic human immunodeficiency virus [HIV] infection status when the patient is HIV positive and does not have any documented symptoms of an HIV-related illness. Do not use this code if the term AIDS is used. If the patient is treated for any HIV-related illness, or is described as having any condition resulting from HIV positive ...
Is HIV a diagnosis?
HIV infection/illness is coded as a diagnosis only for confirmed cases. Confirmation does not require documentation of a positive blood test or culture for HIV; the physician’s diagnostic statement that the patient is HIV positive or has an HIV-related illness is sufficient.#N#In the inpatient setting, HIV is the only condition that must be confirmed to select the code. All other conditions documented as “probable,” suspected,” likely,” “questionable,” “probable,” or “still to rule out” are coded as if they exist in the inpatient setting.#N#Dx. Sequencing#N#The proper sequencing for HIV depends on the reason for the admission or encounter. When a patient is admitted for an HIV-related condition, sequence B20 Human immunodeficiency virus [HIV] disease first, followed by additional diagnosis codes for all reported HIV-related conditions. Conditions always considered HIV-related include Kaposi’s sarcoma, lymphoma, Pneumocystis carinii pneumonia (PCP), cryptococcal meningitis, and cytomegaloviral disease. These conditions are considered opportunistic infections.#N#If a patient with HIV disease is admitted for an unrelated condition (e.g., fracture), sequence the code for the unrelated condition, first. Report B20 as an additional diagnosis, along with any HIV-related conditions.#N#Apply Z21 Asymptomatic human immunodeficiency virus [HIV] infection status when the patient is HIV positive and does not have any documented symptoms of an HIV-related illness. Do not use this code if the term AIDS is used. If the patient is treated for any HIV-related illness, or is described as having any condition resulting from HIV positive status, use B20.#N#Patients with inconclusive HIV serology, and no definitive diagnosis or manifestations of the illness, may be assigned code R75 Inconclusive laboratory evidence of human immunodeficiency virus [HIV].#N#Known prior diagnosis of an HIV-related illness should be coded to B20. After a patient has developed an HIV-related illness, the patient’s condition should be assigned code B20 on every subsequent admission/encounter. Never assign R75 or Z21 to a patient with an earlier diagnosis of AIDS or symptomatic HIV (B20).#N#If a patient is being seen to determine HIV status, use code Z11.4 Encounter for screening for human immunodeficiency virus [HIV]. Should a patient with signs, symptoms or illness, or a confirmed HIV-related diagnosis be tested for HIV, code the signs and symptoms or the diagnosis. If the results are positive and the patient is symptomatic, report B20 with codes for the HIV-related symptoms or diagnosis. The HIV counseling code (Z71.7) may be used if counseling is provided for patients with positive test results. When a patient believes that he/she has been exposed to or has come into contact with the HIV virus, report Z20.6.
When will the 2022 ICd-10-CM N18.6 be released?
The 2022 edition of ICD-10-CM N18.6 became effective on October 1, 2021.
What does the title of a manifestation code mean?
In most cases the manifestation codes will have in the code title, "in diseases classified elsewhere.". Codes with this title are a component of the etiology/manifestation convention. The code title indicates that it is a manifestation code.
What is Z53 in healthcare?
Z53 Persons encountering health services for... are intended for use to indicate a reason for care. They may be used for patients who have already been treated for a disease or injury, but who are receiving aftercare or prophylactic care, or care to consolidate the treatment, or to deal with a residual state.
What is a Z40-Z53?
Categories Z40-Z53 are intended for use to indicate a reason for care. They may be used for patients who have already been treated for a disease or injury, but who are receiving aftercare or prophylactic care, or care to consolidate the treatment, or to deal with a residual state. Type 2 Excludes.
When will ICD-10-CM I12.0 be released?
The 2022 edition of ICD-10-CM I12.0 became effective on October 1, 2021.
What is end stage renal disease?
End stage renal disease due to hypertension, on dialysis. End stage renal disease on dialysis due to hypertension. Hypertension concurrent and due to end stage renal disease on dialysis due to type 2 diabetes mellitus. Hypertension in chronic kidney disease stage 5 due to type 2 diabetes mellitus.
What does the title of a manifestation code mean?
In most cases the manifestation codes will have in the code title, "in diseases classified elsewhere.". Codes with this title are a component of the etiology/manifestation convention. The code title indicates that it is a manifestation code.
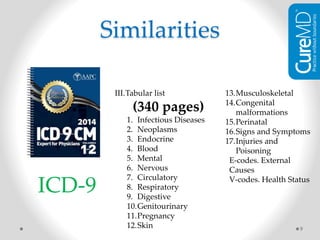
Why is ICD-9 used?
A second reason to update the ICD-9–based instrument was to reflect developments in the treatment of HIV infection, which in isolation is no longer associated with near-term (90-day) mortality . The category for AIDS created by Charlson and colleagues explicitly excluded HIV-positive status, whereas instruments based on administrative data either did not differentiate between the 2 conditions3,7,8or did not include AIDS and HIV infection as clinical categories.9Quan and colleagues assigned to HIV infection the same weight (6 points) that was assigned to metastatic cancer.7Adding to the problem, the World Health Organization has discontinued using the code for AIDS in ICD-9and ICD-10, leaving only HIV-positive category as a valid diagnosis.10
When was the last time ICD-9 was used?
The initial two 12-month time windows were the last 1-year periods in which ICD-9codes were used exclusively in the United States (ie, October 2013-September 2014 and October 2014-September 2015) . The third time window was the earliest 1-year window where ICD-10codes were used exclusively (ie, October 2015-September 2016). The CCI scoring was based on diagnosis codes in claims for services received during these time periods.
How many points are assigned to HIV without AIDS?
For renal disease, we changed the 2 points for a single category to 1 for mild-to-moderate disease and to 3 for severe renal disease. We assigned 3 points to HIV without AIDS, based on our authors' consensus, and ascribed 6 points to AIDS as is the case in previous scoring versions.
What is the term for a disease of the bronchi, trachea, esophag?
Candidiasis of bronchi, trachea, esophagus, or lungs
What is the 9th revision of CCI?
An early CCI instrument based on diagnosis codes translated chart review condition categories into International Classification of Diseases, Ninth Revision(ICD-9) diagnosis codes with 3-digit specificity.2 The use of diagnostic coding for reimbursement purposes creates an incentive for providers to use more accurate and precise coding. Accordingly, newer claims-based versions of the CCI, such as the frequently used instrument designed by Deyo and colleagues, incorporated 4- and 5-digit codes.3
Popular Posts:
- 1. icd 10 code for palliative ge stent placement
- 2. what is the icd 10 code for grade 1 diastolic dysfunction of lv
- 3. icd 10 code for history of alcohol abuse
- 4. icd 10 code for limited range of motion right knee
- 5. icd 10 code for attention and concentration deficit
- 6. icd 10 code for past hepatitis of a and b
- 7. icd 10 code for metastatic brain cancer
- 8. icd 9 code for paresthesia
- 9. icd-9-cm diagnosis code for a patient with an elevated prostate specific antigen (psa) test result.
- 10. icd 10 code for 787.01