Where can one find ICD 10 diagnosis codes?
Search the full ICD-10 catalog by:
- Code
- Code Descriptions
- Clinical Terms or Synonyms
What are the new ICD 10 codes?
The new codes are for describing the infusion of tixagevimab and cilgavimab monoclonal antibody (code XW023X7), and the infusion of other new technology monoclonal antibody (code XW023Y7).
Are Cancer Registrars ready for ICD-10?
Currently, there is no requirement for ICD-10-PCS training. Cancer registrars who don't maintain AHIMA credentials don't need ICD-10-specific credit hours, but it is strongly recommended that they familiarize themselves with the code set. Unfortunately, medical coder classes likely are more in-depth than what's necessary for registrars.
What is the ICD 10 diagnosis code for?
The ICD-10-CM is a catalog of diagnosis codes used by medical professionals for medical coding and reporting in health care settings. The Centers for Medicare and Medicaid Services (CMS) maintain the catalog in the U.S. releasing yearly updates.

What is diagnosis code Z71 89?
Other specified counselingICD-10 code Z71. 89 for Other specified counseling is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
What does code Z12 31 mean?
For example, Z12. 31 (Encounter for screening mammogram for malignant neoplasm of breast) is the correct code to use when you are ordering a routine mammogram for a patient.
What is diagnosis code Z80 9?
9: Family history of malignant neoplasm, unspecified.
What is code Z12 39?
ICD-10 code Z12. 39 for Encounter for other screening for malignant neoplasm of breast is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
What does code Z12 11 mean?
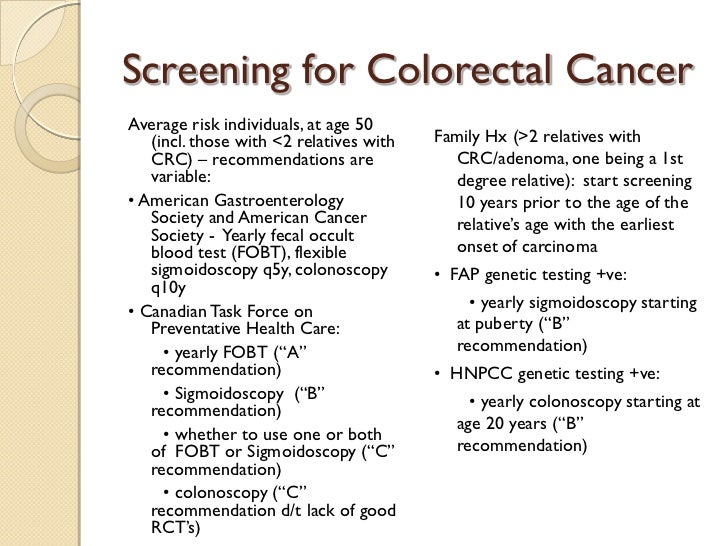
A screening colonoscopy should be reported with the following International Classification of Diseases, 10th edition (ICD-10) codes: Z12. 11: Encounter for screening for malignant neoplasm of the colon. Z80. 0: Family history of malignant neoplasm of digestive organs.
What is the difference between Z12 31 and Z12 39?
Z12. 31 (Encounter for screening mammogram for malignant neoplasm of breast) is reported for screening mammograms while Z12. 39 (Encounter for other screening for malignant neoplasm of breast) has been established for reporting screening studies for breast cancer outside the scope of mammograms.
What is the ICD-10 code for family history of melanoma?
Family history of malignant neoplasm, unspecified Z80. 9 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM Z80. 9 became effective on October 1, 2021.
What is the ICD-10 code for family history of leukemia?
Z80. 6 - Family history of leukemia. ICD-10-CM.
What is the ICD-10 code for family history of heart disease?
ICD-10 Code for Family history of ischemic heart disease and other diseases of the circulatory system- Z82. 49- Codify by AAPC.
Can Z12 31 be a primary diagnosis?
Z12. 31, Encounter for screening mammogram for malignant neoplasm of breast, is the primary diagnosis code assigned for a screening mammogram. If the mammogram is diagnostic, the ICD-10-CM code assigned is the reason the diagnostic mammogram was performed.
What is Z00 01?
ICD-10 code Z00. 01 for Encounter for general adult medical examination with abnormal findings is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
What is diagnosis code N64 4?
ICD-10 code N64. 4 for Mastodynia is a medical classification as listed by WHO under the range - Diseases of the genitourinary system .
What is the Z80.8 code?
Z80.8 is a billable diagnosis code used to specify a medical diagnosis of family history of malignant neoplasm of other organs or systems. The code Z80.8 is valid during the fiscal year 2021 from October 01, 2020 through September 30, 2021 for the submission of HIPAA-covered transactions.
How does cancer start?
Cancer begins in your cells, which are the building blocks of your body. Normally, your body forms new cells as you need them, replacing old cells that die. Sometimes this process goes wrong. New cells grow even when you don't need them, and old cells don't die when they should. These extra cells can form a mass called a tumor. Tumors can be benign or malignant. Benign tumors aren't cancer while malignant ones are. Cells from malignant tumors can invade nearby tissues. They can also break away and spread to other parts of the body.
What is the difference between benign and malignant tumors?
These extra cells can form a mass called a tumor. Tumors can be benign or malignant. Benign tumors aren't cancer while malignant ones are. Cells from malignant tumors can invade nearby tissues. They can also break away and spread to other parts of the body. Cancer is not just one disease but many diseases.
What is the term for the spread of cancer from one part of the body to another?
For example, lung cancer starts in the lung, and breast cancer starts in the breast. The spread of cancer from one part of the body to another is called metastasis. Symptoms and treatment depend on the cancer type and how advanced it is. Most treatment plans may include surgery, radiation and/or chemotherapy.
Is Z80.8 a POA?
Z80.8 is exempt from POA reporting - The Present on Admission (POA) indicator is used for diagnosis codes included in claims involving inpatient admissions to general acute care hospitals. POA indicators must be reported to CMS on each claim to facilitate the grouping of diagnoses codes into the proper Diagnostic Related Groups (DRG). CMS publishes a listing of specific diagnosis codes that are exempt from the POA reporting requirement. Review other POA exempt codes here.
What is the ICd 10 code for cancer?
For more context, consider the meanings of “current” and “history of” (ICD-10-CM Official Guidelines for Coding and Reporting; Mayo Clinic; Medline Plus, National Cancer Institute):#N#Current: Cancer is coded as current if the record clearly states active treatment is for the purpose of curing or palliating cancer, or states cancer is present but unresponsive to treatment; the current treatment plan is observation or watchful waiting; or the patient refused treatment.#N#In Remission: The National Cancer Institute defines in remission as: “A decrease in or disappearance of signs or symptoms of cancer. Partial remission, some but not all signs and symptoms of cancer have disappeared. Complete remission, all signs and symptoms of cancer have disappeared, although cancer still may be in the body.”#N#Some providers say that aromatase inhibitors and tamoxifen therapy are applied during complete remission of invasive breast cancer to prevent the invasive cancer from recurring or distant metastasis. The cancer still may be in the body.#N#In remission generally is coded as current, as long as there is no contradictory information elsewhere in the record.#N#History of Cancer: The record describes cancer as historical or “history of” and/or the record states the current status of cancer is “cancer free,” “no evidence of disease,” “NED,” or any other language that indicates cancer is not current.#N#According to the National Cancer Institute, for breast cancer, the five-year survival rate for non-metastatic cancer is 80 percent. The thought is, if after five years the cancer isn’t back, the patient is “cancer free” (although cancer can reoccur after five years, it’s less likely). As coders, it’s important to follow the documentation as stated in the record. Don’t go by assumptions or averages.
What is the ICd 10 code for primary malignancy?
According to the ICD-10 guidelines, (Section I.C.2.m):#N#When a primary malignancy has been excised but further treatment, such as additional surgery for the malignancy, radiation therapy, or chemotherapy is directed to that site, the primary malignancy code should be used until treatment is complete.#N#When a primary malignancy has been excised or eradicated from its site, there is no further treatment (of the malignancy) directed to that site, and there is no evidence of any existing primary malignancy, a code from category Z85, Personal history of malignant neoplasm, should be used to indicate the former site of the malignancy.#N#Section I.C.21.8 explains that when using a history code, such as Z85, we also must use Z08 Encounter for follow-up examination after completed treatment for a malignant neoplasm. This follow-up code implies the condition is no longer being actively treated and no longer exists. The guidelines state:#N#Follow-up codes may be used in conjunction with history codes to provide the full picture of the healed condition and its treatment.#N#A follow-up code may be used to explain multiple visits. Should a condition be found to have recurred on the follow-up visit, then the diagnosis code for the condition should be assigned in place of the follow-up code.#N#For example, a patient had colon cancer and is status post-surgery/chemo/radiation. The patient chart notes, “no evidence of disease” (NED). This is reported with follow-up code Z08, first, and history code Z85.038 Personal history of other malignant neoplasm of large intestine, second. The cancer has been removed and the patient’s treatment is finished.
What is preventative cancer?
Preventative or Prophylactic – to keep cancer from reoccurring in a person who has already been treated for cancer or to keep cancer from occurring in a person who has never had cancer but is at increased risk for developing it due to family history or other factors.
Does history of cancer affect relative value units?
The fear is, history of will be seen as a less important diagnosis, which may affect relative value units . Providers argue that history of cancer follow-up visits require meaningful review, examinations, and discussions with the patients, plus significant screening and watching to see if the cancer returns.
Is cancer history?
History of Cancer: The record describes cancer as historical or “history of” and/or the record states the current status of cancer is “cancer free,” “no evidence of disease,” “NED,” or any other language that indicates cancer is not current. According to the National Cancer Institute, for breast cancer, the five-year survival rate ...
Do providers look at cancer at the cellular level?
According to a presentation by James M. Taylor, MD, CPC, providers look at cancer at a cellular level; whereas, coding guidelines look more at the organ level. In his opinion, common concerns among providers are: Some neoplasms may not be active but remain at a cellular level, and can become active.
Section 1.C.2 Provides Guidance
- According to the ICD-10 guidelines, (Section I.C.2.m): When a primary malignancy has been excised but further treatment, such as additional surgery for the malignancy, radiation therapy, or chemotherapy is directed to that site, the primary malignancy code should be used until treatment is complete. When a primary malignancy has been excised or era...
Defining Terms with Care
- For more context, consider the meanings of “current” and “history of” (ICD-10-CM Official Guidelines for Coding and Reporting; Mayo Clinic; Medline Plus, National Cancer Institute): Current: Cancer is coded as current if the record clearly states active treatment is for the purpose of curing or palliating cancer, or states cancer is present but unresponsive to treatment; the curr…
Active Treatment vs. Preventative Care
- What if a patient with breast cancer is status post-surgery/chemotherapy/radiation and is currently on tamoxifen for five years? If the patient is on tamoxifen or an aromatase inhibitor, such as Arimidex®, is that active treatment or preventive care (to inhibit returning cancer). Ultimately, what determines active treatment versus preventive care is how the drug is used. For example: 1…
The Provider Perspective
- Do providers agree with the above guidelines, or are the clinical and coding worlds at odds? According to a presentation by James M. Taylor, MD, CPC, providers look at cancer at a cellular level; whereas, coding guidelines look more at the organ level. In his opinion, common concerns among providers are: 1. Some neoplasms may not be active but remain at a cellular level, and ca…
“History Of” Doesn’T Mean A Lesser Service
- I’ve heard providers worry about the level of medical decision-making assigned to a history of diagnosis, versus a current status diagnosis. The fear is, history of will be seen as a less important diagnosis, which may affect relative value units. Providers argue that history of cancer follow-up visits require meaningful review, examinations, and discussions with the patients, plu…
Popular Posts:
- 1. icd 9 code for routine blood work
- 2. icd 10 code for incarcerated epigastric hernia
- 3. icd 10 code for proteinaceous
- 4. icd 10 code for encounter for preoperative clearance
- 5. icd 10 code for atypical squamous cells of undetermined significance
- 6. icd 10 code for disc space narrowing
- 7. icd-9 code for 365.9
- 8. icd 10 code for repair hiatal hernia
- 9. icd 10 code for orthostatic tachycardia
- 10. 2017 icd 10 code for tendinitis of left supraspinatus tendon