What is the ICD 10 code for hga1c?
Unit Code: 16600CPT: 83036 HgA1C ICD-10 codes covered if selection criteria are met: Note: Policy subject to change and does not guarantee reimbursement.
What is the CPT code for screening diagnosis?
The screening diagnosis code V77.1 is required in the header diagnosis section of the claim and the modifier “TS” (follow-up service) is to be reported on the line item. Important Note: The Centers for Medicare and Medicaid Services (CMS) monitors the use of its preventive and screening benefits.
What is the ICD 10 code for diabetes mellitus screening?
Encounter For Screening For Diabetes Mellitus Z13.1 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. This is the American ICD-10-CM version of Z13.1 - other international versions of ICD-10 Z13.1 may differ.
What is the diagnosis code for prediabetes screening?
To indicate that the purpose of the test (s) is diabetes screening for a beneficiary who meets the *definition of prediabetes. The screening diagnosis code V77.1 is required in the header diagnosis section of the claim and the modifier “TS” (follow-up service) is to be reported on the line item.
What ICD-10 codes cover HbA1c?
This NCD lists the ICD-10 codes for HbA1c for frequencies up to once every three months. The ICD-10-CM codes for test frequencies exceeding one every 90 days are listed below. E08. 319 Diabetes mellitus due to underlying condition with unspecified diabetic retinopathy without macular edema E08.
What diagnosis will cover hemoglobin A1c?
The measurement of hemoglobin A1c is recommended for diabetes management, including screening, diagnosis, and monitoring for diabetes and prediabetes. hyperglycemia (Skyler et al., 2017).
What is the ICD-10 code for screening for diabetes?
You would assign ICD-10 code Z13. 1, Encounter for screening for diabetes mellitus. This code can be found under “Screening” in the Alphabetical Index of the ICD-10 book.
What is the ICD code for A1c?
ICD-10-CM Code for Elevated blood glucose level R73.
What are the ICD-10 codes for diabetes?
Coding Diabetes Mellitus in ICD-10-CM: Improved Coding for Diabetes Mellitus Complements Present Medical ScienceE08, Diabetes mellitus due to underlying condition.E09, Drug or chemical induced diabetes mellitus.E10, Type 1 diabetes mellitus.E11, Type 2 diabetes mellitus.E13, Other specified diabetes mellitus.
What is the ICD-10 code for type 2 diabetes?
ICD-Code E11* is a non-billable ICD-10 code used for healthcare diagnosis reimbursement of Type 2 Diabetes Mellitus. Its corresponding ICD-9 code is 250. Code I10 is the diagnosis code used for Type 2 Diabetes Mellitus.
What is the ICD-10 code for screening?
9.
Does Medicare cover hba1c testing?
Hemoglobin A1c Tests: Your doctor might order a hemoglobin A1c lab test. This test measures how well your blood glucose has been controlled over the past 3 months. Medicare may cover this test for anyone with diabetes if it is ordered by his or her doctor.
What is the ICD-10 code for annual physical exam?
Z00.00ICD-10 Code for Encounter for general adult medical examination without abnormal findings- Z00. 00- Codify by AAPC.
What is the CPT code for diabetes screening?
Medicare Diabetes Screening guideline – CPT 82947, 82950 , 82951.
What is the ICd 10 code for a symptom?
R00-R99 Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified R70-R79 Abnormal findings on examination of blood, without diagnosis 2018/2019 ICD-10-CM Diagnosis Code R73.09 2016 2017 2018 2019 Billable/Specific Code R73.09 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2018/2019 edition of ICD-10-CM R73.09 became effective on October 1, 2018. This is the American ICD-10-CM version of R73.09 - other international versions of ICD-10 R73.09 may differ. The following code (s) above R73.09 contain annotation back-references In this context, annotation back-references refer to codes that contain: Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified This chapter includes symptoms, signs, abnormal results of clinical or other investigative procedures, and ill-defined conditions regarding which no diagnosis classifiable elsewhere is recorded. Signs and symptoms that point rather definitely to a given diagnosis have been assigned to a category in other chapters of the classification. In general, categories in this chapter include the less well-defined conditions and symptoms that, without the necessary study of the case to establish a final diagnosis, point perhaps equally to two or more diseases or to two or more systems of the body. Practically all categories in the chapter could be designated 'not otherwise specified', 'unknown etiology' or 'transient'. The Alphabetical Index should be consulted to determine which symptoms and signs are to be allocated here and which to other chapters. The residual subcategories, numbered .8, are generally provided for other relevant symptoms that cannot be allocated elsewhere in the classification. The condition Continue reading >>
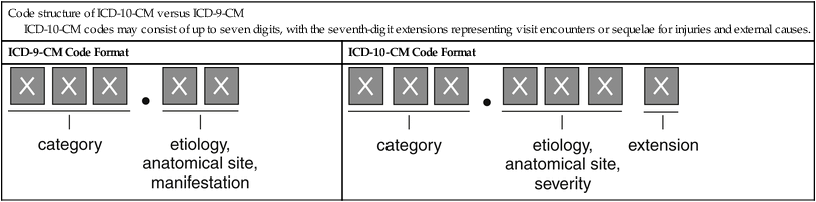
How many ICD-10 codes are there?
The World Health Organization (WHO) has been publishing versions of the ICD since 1948. It is now on the tenth version, ICD-10, which has been adopted for use by over 100 countries, including the U.S. Compared to ICD-9, ICD-10 has more codes and specificity. The former has 14,000 codes, while ICD-10 has over 70,000.
What is the ICd 10 code for diabetes mellitus?
2018/2019 ICD-10-CM Diagnosis Code E11.69 Type 2 diabetes mellitus with other specified complication 2016 2017 2018 2019 Billable/Specific Code E11.69 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2018/2019 edition of ICD-10-CM E11.69 became effective on October 1, 2018. This is the American ICD-10-CM version of E11.69 - other international versions of ICD-10 E11.69 may differ. Certain conditions have both an underlying etiology and multiple body system manifestations due to the underlying etiology. For such conditions the ICD-10-CM has a coding convention that requires the underlying condition be sequenced first followed by the manifestation. Wherever such a combination exists there is a "use additional code" note at the etiology code, and a "code first" note at the manifestation code. These instructional notes indicate the proper sequencing order of the codes, etiology followed by manifestation. In most cases the manifestation codes will have in the code title, "in diseases classified elsewhere." Codes with this title are a component of the etiology/manifestation convention. The code title indicates that it is a manifestation code. "In diseases classified elsewhere" codes are never permitted to be used as first listed or principle diagnosis codes. They must be used in conjunction with an underlying condition code and they must be listed following the underlying condition. The following code (s) above E11.69 contain annotation back-references In this context, annotation back-references refer to codes that contain: Continue reading >>
How to use eCQM patient report?
eCQM Patient Reports can help you identify patient care gaps and improve the performance of your quality measures. Click on the blue result numbers in the eCQM Dashboard to see the patient report for this measure. The eCQM Patient Reports list the individual patients included in the measures population, which measure cohorts the patient is in, and contact information for the patient to streamline any downstream communication that may be needed to fulfill the measure requirements. You can choose to print the patient list for a measure or export it as a CSV. The measure cohorts included in the eCQM Patient Report for CMS 122v5 Diabetes: Hemoglobin A1c (HbA1c) Poor Control (>9%) are: Practice Fusion suggests the following workflow to help ensure that you are able to meet the requirements of this measure within the Practice Fusion EHR. Ensure that patients with diabetes have an appropriate diagnosis, with a start date, recorded in the medical record. Examples of diabetes diagnosis codes that can be used for this measure can be found in Table 1. Receive or record structured lab results for HbA1c tests in the Practice Fusion EHR. HbA1c Test codes that will be included in this measure when manually recording structured lab results in the Practice Fusion EHR or when receiving structured lab results from connected labs can be found in Table 1. Table 1: Examples of Coded Values that can be recorded for CMS 122v5 Hemoglobin A1c/Hemoglobin.total in Blood by HPLC (LOINC code 17856-6) Hemoglobin A1c/Hemoglobin.total in Blood (LOINC code 4548-4) Hemoglobin A1c/Hemoglobin.total in Blood by Electrophoresis (LOINC code4549-2) *Note: Only patients with a diagnosis of Type 1 or Type 2 diabetes will be included in the denominator of this measure; patients with a diagnosis of secondary diab Continue reading >>
When will ICD-10-CM R73.09 be released?
The 2022 edition of ICD-10-CM R73.09 became effective on October 1, 2021.
What does it mean when you have a high blood glucose level?
This condition is seen frequently in diabetes mellitus, but also occurs with other diseases and malnutrition. Pre-diabetes means you have blood glucose levels that are higher than normal but not high enough to be called diabetes. Glucose comes from the foods you eat.
What is the ICd 10 code for diabetes mellitus?
Z13.1 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. This is the American ICD-10-CM version of Z13.1 - other international versions of ICD-10 Z13.1 may differ. Approximate Synonyms Screening for diabetes mellitus Screening for diabetes mellitus done Present On Admission Z13.1 is considered exempt from POA reporting. ICD-10-CM Z13.1 is grouped within Diagnostic Related Group (s) (MS-DRG v35.0): Code History 2016 (effective 10/1/2015): New code (first year of non-draft ICD-10-CM) 2017 (effective 10/1/2016): No change 2018 (effective 10/1/2017): No change Code annotations containing back-references to Z13.1: Reimbursement claims with a date of service on or after October 1, 2015 require the use of ICD-10-CM codes. Continue reading >>
What is the CPT code for hemoglobin A1C?
Point of Care Hemoglobin A1c Testing - CPT Codes 83036 & 83037 by:Charles Root ( [email protected] ) The following two codes are now available for testing A1C in a point-of-care setting: 83036 Hemoglobin; glycosylated (A1c), and 83037 Hemoglobin; glycosylated (A1c) by device cleared by the FDA for home use Since devices cleared for home use are also classified as CLIA waived, in many cases the code will include the -QW modifier. Glycated hemoglobin/protein testing is widely accepted as medically necessary for the management and control of diabetes. It is also valuable to assess hyperglycemia, a history of hyperglycemia or dangerous hypoglycemia. The existing Medicare National Coverage Determination (NCD) for Glycated Hemoglobin/Glycated Protein (190.21) includes detailed information on frequency limitations and diagnosis (ICD-9) codes pertaining to CPT code 83036. As of July 1, 2006, the NCD onlypertained toCPT 83036, however, several Medicare carriers haverecently stated that 83037 will be subject to the same diagnosis and frequency parameters as CPT code 83036. We believe it is only a matter of time until the NCD is updated to include CPT code 83037 as well as 83036. Which Code to Report for Point of Care Testing CPT code 83037 is expected to be reported for tests performed in a physician's office using a device cleared by the FDA for home use, such as a single use test kit with a self-contained analyzer and reporting screen. However, CPT code 83036 may also be reported by a physician's office or or other point-of-care facility using a device NOT approved by the FDA for home use, such as a desk top analyzer. CPT code 83037 mayNOT be reported when the test is performed using a desk top analyzer or other device not approved by the FDA for home use.Carriers will c Continue reading >>
What is the blood glucose level after a glucose tolerance test?
A condition referring to fasting plasma glucose levels being less than 140 mg per deciliter while the plasma glucose levels after a glucose tolerance test being more than 200 mg per deciliter at 30, 60, or 90 minutes. It is observed in patients with diabetes mellitus. Other causes include immune disorders, genetic syndromes, and cirrhosis. A disorder characterized by an inability to properly metabolize glucose. A pathological state in which blood glucose level is less than approximately 140 mg/100 ml of plasma at fasting, and above approximately 200 mg/100 ml plasma at 30-, 60-, or 90-minute during a glucose tolerance test. This condition is seen frequently in diabetes mellitus, but also occurs with other diseases and malnutrition. Pre-diabetes means you have blood glucose levels that are higher than normal but not high enough to be called diabetes. Glucose comes from the foods you eat. Too much glucose in your blood can damage your body over time. If you have pre-diabetes, you are more likely to develop type 2 diabetes, heart disease, and stroke.most people with pre-diabetes don't have any symptoms. Your doctor can test your blood to find out if your blood glucose levels are higher than normal. If you are 45 years old or older, your doctor may recommend that you be tested for pre-diabetes, especially if you are overweight.losing weight - at least 5 to 10 percent of your starting weight - can prevent or delay diabetes or even reverse pre-diabetes. That's 10 to 20 pounds for someone who weighs 200 pounds. You can lose weight by cutting down on the amount of calories and fat you eat and being physically active at least 30 minutes a day. Being physically active makes your body's insulin work better. Your doctor may also prescribe medicine to help control the amount of gluc Continue reading >>
What are the tests for kidney disease?
Detection of CKD can be accomplished with simple tests such as serum creatinine and urine microalbumin. These tests have specific CPT service codes, and are covered by Medicare and by many private health plans. In the Medicare and fee-for-service employer group health plans (EGHPs), laboratory tests can be billed based on physician clinical management under a fee schedule. In other EGHP populations, however, global contracts for areas such as laboratory services may make it difficult to determine exactly which tests are ordered. This is particularly true for the MarketScan dataset, in that the self-insured groups are with companies that hold the funds for services. We have thus limited our analyses of laboratory data in this chapter to the Ingenix i3 dataset. We first evaluate how frequently patients with diabetes, hypertension, or both diagnoses receive a urine microalbumin test. The probability of microalbumin testing within a year in Medicare CKD patients with diabetes has increased since 20012002, reaching 0.32 in 20072008. Among those with hypertension, the probability is now 0.04. Similar rates are noted among those with private insurance. Such data provide important evidence that providers are not screening at-risk patients at intervals recommended by the American Heart Association and the American Diabetes Association. Not surprisingly, the probability of nephrologist referral among Medicare patients with diabetes or hypertension is relatively low, at 616 percent; rates ar Continue reading >>
Is CPT covered by Medicare?
These tests have specific CPT service codes, and are covered by Medicare and by many private health plans. In the Medicare and fee-for-service employer group health plans (EGHPs), laboratory tests can be billed based on physician clinical management under a fee schedule.
What is the ICD-10 code for uncontrolled diabetes?
Under ICD-10 Codes That Support Medical Necessity-Group 2-Secondary Dual Codes-diagnoses that must be used in conjunction with a Group 1 code that indicates a current state of uncontrolled diabetes (hyperglycemia) added E10.21 as it was inadvertently omitted from Group 2.
Can you use CPT in Medicare?
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials of CMS internally within your organization within the United States for the sole use by yourself, employees and agents. Use is limited to use in Medicare, Medicaid or other programs administered by the Centers for Medicare and Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
Is CPT a year 2000?
CPT is provided “as is” without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. AMA warrants that due to the nature of CPT, it does not manipulate or process dates, therefore there is no Year 2000 issue with CPT. AMA disclaims responsibility for any errors in CPT that may arise as a result of CPT being used in conjunction with any software and/or hardware system that is not Year 2000 compliant. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon no upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
Why do contractors need to specify revenue codes?
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination. Complete absence of all Revenue Codes indicates that coverage is not influenced by Revenue Code and the article should be assumed to apply equally to all Revenue Codes.
Can you use CPT in Medicare?
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials of CMS internally within your organization within the United States for the sole use by yourself, employees and agents. Use is limited to use in Medicare, Medicaid or other programs administered by the Centers for Medicare and Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
Is CPT a year 2000?
CPT is provided “as is” without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. AMA warrants that due to the nature of CPT, it does not manipulate or process dates, therefore there is no Year 2000 issue with CPT. AMA disclaims responsibility for any errors in CPT that may arise as a result of CPT being used in conjunction with any software and/or hardware system that is not Year 2000 compliant. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon no upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
What is the diagnosis code for diabetes screening?
The screening diagnosis code V77.1 is required in the header diagnosis section of the claim. MEET. -TS. V77.1.
What is the code for a prediabetic screening test?
To indicate that the purpose of the test (s) is diabetes screening for a beneficiary who meets the *definition of prediabetes. The screening diagnosis code V77.1 is required in the header diagnosis section of the claim and the modifier “TS” (follow-up service) is to be reported on the line item.
What is the HCPCS code for IBT?
The HCPCS Code for IBT is G0447 for Face-to-face behavioral counseling for obesity, 15 minutes. Payment to the provider is currently being made on a fee-for-service basis, with Medicare covering up to 22 IBT encounters in a 12-month period: One face-to-face visit every week for the first month.
What is CMS coding?
Important Note: The Center s for Medicare and Medicaid Services (CMS) monitors the use of its preventive and screening benefits. By correctly coding for diabetes screening and other benefits, providers can help CMS more accurately track the use of these important services and identify opportunities for improvement.
What is the V77.1 code?
V77.1. To indicate that the purpose of the test (s) is diabetes screening for a beneficiary who meets the *definition of prediabetes. The screening diagnosis code V77.1 is required in the header diagnosis section of the claim and the modifier “TS” (follow-up service) is to be reported on the line item.
What is the ICD-10 code for prediabetes?
(HIPAA). The change to ICD-10 does not affect CPT coding for outpatient procedures and physician services. The ICD-10 code for prediabetes is R73.09.
Does Medicare cover diabetes screening?
Medicare recommends and provides coverage for diabetes screening tests through Part B Preventive Services for beneficiaries at risk for diabetes or those diagnosed with prediabetes. For more about preventive services, see Medicare’s Preventive Services (PDF, 106 KB) chart, which includes information about "Diabetes Screening," "Diabetes Self-Management Training," and "Annual Wellness Visit." The Quick Reference Information: The ABCs of Providing the Annual Wellness Visit (PDF, 3.03 MB) provides additional information about this benefit.
What is the ICd 10 code for diabetes mellitus?
Z13.1 is a valid billable ICD-10 diagnosis code for Encounter for screening for diabetes mellitus . It is found in the 2021 version of the ICD-10 Clinical Modification (CM) and can be used in all HIPAA-covered transactions from Oct 01, 2020 - Sep 30, 2021 .
Do you include decimal points in ICD-10?
DO NOT include the decimal point when electronically filing claims as it may be rejected. Some clearinghouses may remove it for you but to avoid having a rejected claim due to an invalid ICD-10 code, do not include the decimal point when submitting claims electronically. See also: Screening (for) Z13.9. diabetes mellitus Z13.1.
Expected Turnaround Time
Turnaround time is defined as the usual number of days from the date of pickup of a specimen for testing to when the result is released to the ordering provider. In some cases, additional time should be allowed for additional confirmatory or additional reflex tests. Testing schedules may vary.
Minimum Volume
Pediatric EDTA whole blood tubes may be used. Please place original labeled capillary tube in a labeled transport tube for shipment to the laboratory. ( Note: This volume does not allow for repeat testing.)
Container
Lavender-top (EDTA) tube, green-top (lithium heparin) tube, or gray-top (sodium fluoride) tube
Collection
The usual precautions in the collection of venipuncture samples should be observed. The sample must be free of clots. Samples with any hematocrit disorders can lead to erroneous results. Send the entire tube to the laboratory.
Limitations
Any cause of shortened erythrocyte survival will reduce exposure of erythrocytes to glucose with a consequent decrease in Hb A 1c (%). Causes of shortened erythrocyte lifetime might be hemolytic anemia or other hemolytic diseases, homozygous sickle cell trait, pregnancy, or recent significant or chronic blood loss.
Additional Information
Factors such as duration of diabetes, adherence to therapy, and age of patient should also be considered in assessing the degree of blood glucose control.
Popular Posts:
- 1. icd 10 code for liver inflammation
- 2. icd 10 code for school problems
- 3. icd 10 code for laceration left shin
- 4. icd 10 code for perforated iud
- 5. icd 10 code for laceration left face
- 6. icd 10 code for severe anemia, status post blood transfusion
- 7. icd 10 code for lip licking dermatitis
- 8. icd 10 code for open wound of tie
- 9. icd 10 code for hydronephrosis newborn
- 10. icd 10 code for left breast throat wound