What is the procedure code for observation?
CPT codes 99218-99220, initial observation care, describe physician visits during a patient's stay in observation status. CPT codes 99234-99236, observation or inpatient care, are used when the patient is placed in observation status or admitted to inpatient status and then discharged on the same date.
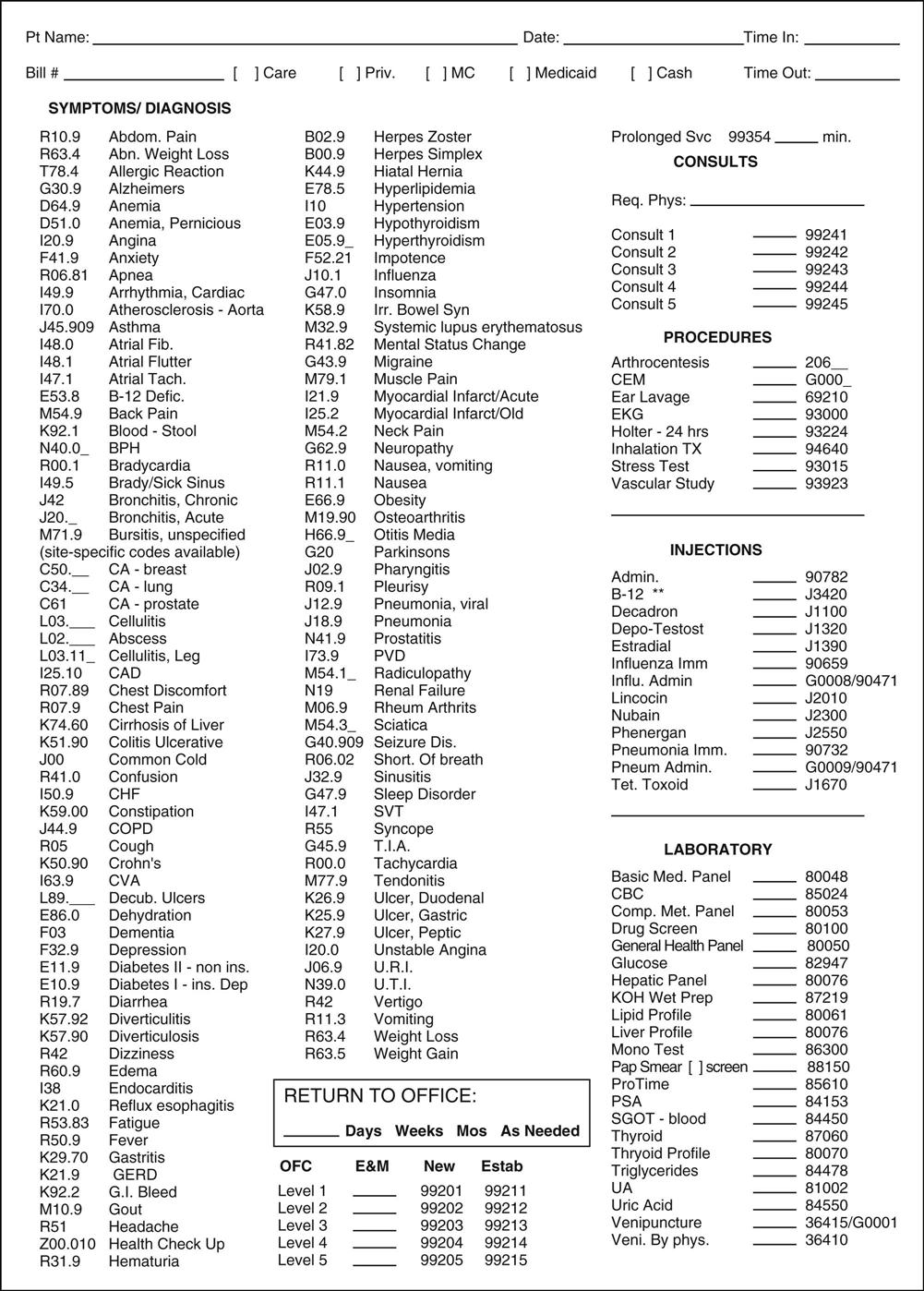
What are the new ICD 10 codes?
- M35.00 (Sjogren syndrome, unspecified)
- M35.01 (Sjogren syndrome with keratoconjunctivitis)
- M35.02 (Sjogren syndrome with lung involvement)
- M35.03 (Sjogren syndrome with myopathy)
- M35.04 (Sjogren syndrome with tubulo-interstitial nephropathy)
- M35.05 (Sjogren syndrome with inflammatory arthritis)
What is the difference between ICD 9 and ICD 10?
- Similar to the diagnosis code set, the alpha characters in ICD 10 code sets are not case-sensitive.
- The letters “O” and “I” are not in the code set. ...
- The 7 characters in the procedure code set help in providing very precise details. ...
- The fourth character identifies the part of the body. ...
What does ICD 10 mean?
ICD-10. ICD-10 is the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD), a medical classification list by the World Health Organization (WHO). It contains codes for diseases, signs and symptoms, abnormal findings, complaints, social circumstances, and external causes of injury or diseases.
How do you code hospital observations?
CPT codes 99234-99236, observation or inpatient care, are used when the patient is placed in observation status or admitted to inpatient status and then discharged on the same date. All services provided on the day of discharge from inpatient status are coded 99238 or 99239.
What is the CPT code for hospital observation?
Observation or Inpatient Hospital Care (including admission and discharge) CPT codes 99234-99236 are used to report observation or initial hospital services for a patient that is admitted and discharged on the same date of service.
How do you code observation status?
If the patient is still in observation status at the time of discharge, use 99217. If the patient is an inpatient, use codes 99238 or 99239. Remember to use observation discharge when the patient's status is observation and use inpatient discharge when the patient's status is inpatient.
What is the POS code for observation?
POS 22If a patient was in observation, then use POS 22. But if the patient was actually admitted and discharged on the same day, then go with POS 21.
What is observation in the hospital?
Observation status, when chosen initially, is when you are placed in a bed anywhere within the hospital, but have an unclear need for longer care or your condition usually responds to less than 48 hours of care.
What is the CPT code for 23 hour observation?
23-hour observation stay According to CPT, 99218–99220 plus 99217 are for admission and discharge on two separates dates of service, and 99234–99236 are for admission and discharge on the same date of service.
When a patient is admitted for observation for a medical condition assign a code for the?
If a patient is admitted for observation for a medical condition, a code is assigned for the medical condition as the first-listed diagnosis. It is acceptable to use codes that describe signs and symptoms when a definitive diagnosis has not been established by the provider.
Does Medicare accept observation codes?
Some commercial payers still recognize outpatient consults, and allow a consulting physician to bill subsequent observation codes. But Medicare does not.
Can you bill critical care in observation?
One physician cannot bill for both ED E/M services and an inpatient or observation admission for the same patient. So if the physician first treated the patient in the ED and then admitted the patient to observation or as an inpatient, he or she can bill only one of those services.
What is the difference between POS 11 and 22?
I think it would be POS 11 even if it is owned by the hospital it is offsite and in an office. 22 POS to me is when a service is performed in the hospital and the patient is never admitted.
What is the difference between POS 19 and 22?
Beginning January 1, 2016, POS code 22 was redefined as “On-Campus Outpatient Hospital” and a new POS code 19 was developed and defined as “Off-Campus Outpatient Hospital.” Effective January 1, 2016, POS 19 must be used on professional claims submitted for services furnished to patients registered as hospital ...
What is the difference between POS 31 and 32?
POS 32. Use POS 31 when the patient is in a skilled nursing facility (SNF), which is a short-term care/rehabilitation facility. Use POS 32 when the patient is in a long-term nursing care facility.
What is the difference between 99238 and 99239?
The only difference between a 99238 and a 99239 is that a 99239 is greater than 30 minutes spent on discharge and a 99238 is thirty minutes or less spent on discharge. Please reference the AMA's CPT 2018 Standard Edition as the definitive authority in CPT® coding, available below and to the right from Amazon.
What does CPT code 99223 mean?
Initial hospital careCPT 99223 is defined as: Initial hospital care, per day, for the evaluation and management of a patient, which requires these three key components: A comprehensive history. A comprehensive exam. Medical decision making of high complexity.
What does CPT code 96374 mean?
CPT® Code 96374 in section: Therapeutic, prophylactic, or diagnostic injection (specify substance or drug)
What does CPT code 99224 mean?
Subsequent observation care, per dayCPT Code Description 99224 Subsequent observation care, per day, for the evaluation and management of a patient, which requires at least 2 of these 3 key components: Problem focused interval history; Problem focused examination; Medical decision making that is straightforward or of low complexity.
General Information
CPT codes, descriptions and other data only are copyright 2021 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Title XVIII of the Social Security Act 1833 (e) prohibits Medicare payment for any claim lacking the necessary documentation to process the claim
Article Guidance
The information in this article contains billing, coding or other guidelines that complement the Local Coverage Determination (LCD) for Outpatient Observation Bed/Room Services L34552.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
What is the code for observation status?
To report services to a patient designated as “observation status” or “inpatient status” and discharged on the same date, use the codes for Observation or Inpatient Care Services [including Admission and Discharge Services, 99234-99236 as appropriate.])
How long does it take to get to observation status?
Usually, the problem (s) requiring admission to “observation status” are of high severity. Typically 70 minutes are spent at the bedside and on the patient’s hospital floor or unit.
Is it necessary to have a patient in an observation area?
A: It is not necessary that the patient be located in an observation area designated by the hospital as long as the medical record indicates that the patient was admitted as observation status and the reason for Observation Care is documented.
What is the code for observation care?
If the duration of observation care is less than eight hours on the same date of service, codes 99218-99220 are appropriate, but do not report the discharge (99217) separately.
When a patient is placed in observation status, do they need to know the documentation guidelines for time?
When a patient is placed in observation status, know the documentation guidelines for time. Occasionally, a physician will need to observe a patient in the hospital for a time beyond that of a single-visit encounter. In these instances, instead of admitting the patient as inpatient status, the physician may admit the patient as observation status ...
What is a 99217 discharge?
When a patient remains in observation beyond an initial date of service, separately report a discharge service on the day of discharge using 99217 Observation care discharge day management. CPT® clarifies that 99217 includes, “all services provided to a patient on discharge from ‘observation status’ if the discharge is on other than the initial date of ‘observation status.’”#N#Continuing with Example 2: If on day 2 Dr. Q deems the 68-year-old, insulin-dependent diabetic (admitted to observation status 10/12/16) ready for discharge, report 99220 for the first day and 99217 for discharge on day 2. If the patient remains in observation throughout day 2 and is released on day 3, however, report 99220 (day 1), 99225 (day 2), and 99217 (day 3 discharge).#N#No documentation of time is warranted for 99217; however, final exam, discussion of stay, and preparation of discharge record are required.
How long is observation status?
When coding observation services, there is a distinction between services lasting beyond 24 hours, and those lasting at least eight hours, but less than 24 hours.
How long does a physician have to provide documentation to report a charge?
If the patient’s condition warrants observation beyond 24 hours , the physician must provide adequate documentation (meeting the required two of the three key elements) to report a charge. The patient is considered “established” at this point.
What happens after day 3 of a patient's stay?
If after day 3 the patient’s condition deteriorates and requires further monitoring, the physician could write orders admitting the patient to inpatient status. As stated above, when the patient is admitted as an inpatient, observation services are not reported for that day.
What is the code for observation care?
Initial Observation Care codes (99218 – 99220) are used to report E&M services provided to patients designated/admitted as “observation status” in a hospital to determine whether they warrant admission, transfer, or discharge.
What is the CPT code for observation?
The observation discharge, CPT code 99217, cannot also be reported.
What is the E&M code for admission and discharge to observation?
Admission and Discharge to Observation, Same Day – E&M codes (99234 – 99236) used to report services for a patient who is admitted and discharged from an observation or inpatient stay on the same calendar date. Patient’s stay must be a minimum of eight hours in order to bill these codes.
Who can bill for observation status?
Physicians other than the physician initiating observation status may bill, as appropriate, office and other outpatient service codes. This code includes all services performed at all sites by the admitting physician that relate to the observation admission.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Title XVIII of the Social Security Act, Section 1833 (e) states that no payment shall be made to any provider of services or other person under this part unless there has been furnished such information as may be necessary in order to determine the amounts due such provider or other person under this part for the period with respect to which the amounts are being paid or for any prior period..
Article Guidance
Medicare rules and regulations regarding acute care inpatient, observation and treatment room services are outlined in the Medicare Internet-Only Manuals (IOMs).
ICD-10-CM Codes that Support Medical Necessity
It is the provider’s responsibility to select codes carried out to the highest level of specificity and selected from the ICD-10-CM code book appropriate to the year in which the service is rendered for the claim (s) submitted.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.

Popular Posts:
- 1. icd 10 code for failed induction of labor by oxytocin 3rd trimester
- 2. icd 10 code for subchorionic hematoma in second trimester
- 3. validity of icd-9-cm diagnosis code for alzheimer's disease
- 4. icd 10 code for in-toeing
- 5. icd 10 code for sprain right latissimus dorsi and dorsal paraspinal groups
- 6. icd 10 code for bilateral femur neck fx unspecified
- 7. icd 10 code for pseudoangiomatous stromal hyperplasia of the breast
- 8. icd 10 code for chronic renal failure stage 5
- 9. icd 10 cm code for pain in right thigh area
- 10. icd 10 code for syphilis screen (rpr)