What is the ICD 10 code for secondary hypercoagulabe state?
I used 289.82 (secondary hypercoagulabe state) and E934.2 when we had a patient with a similar scenario. Or you could use 790.92 (abnormal coagulation profile).
What is the ICD 10 code for hypercoagulable thrombophilia?
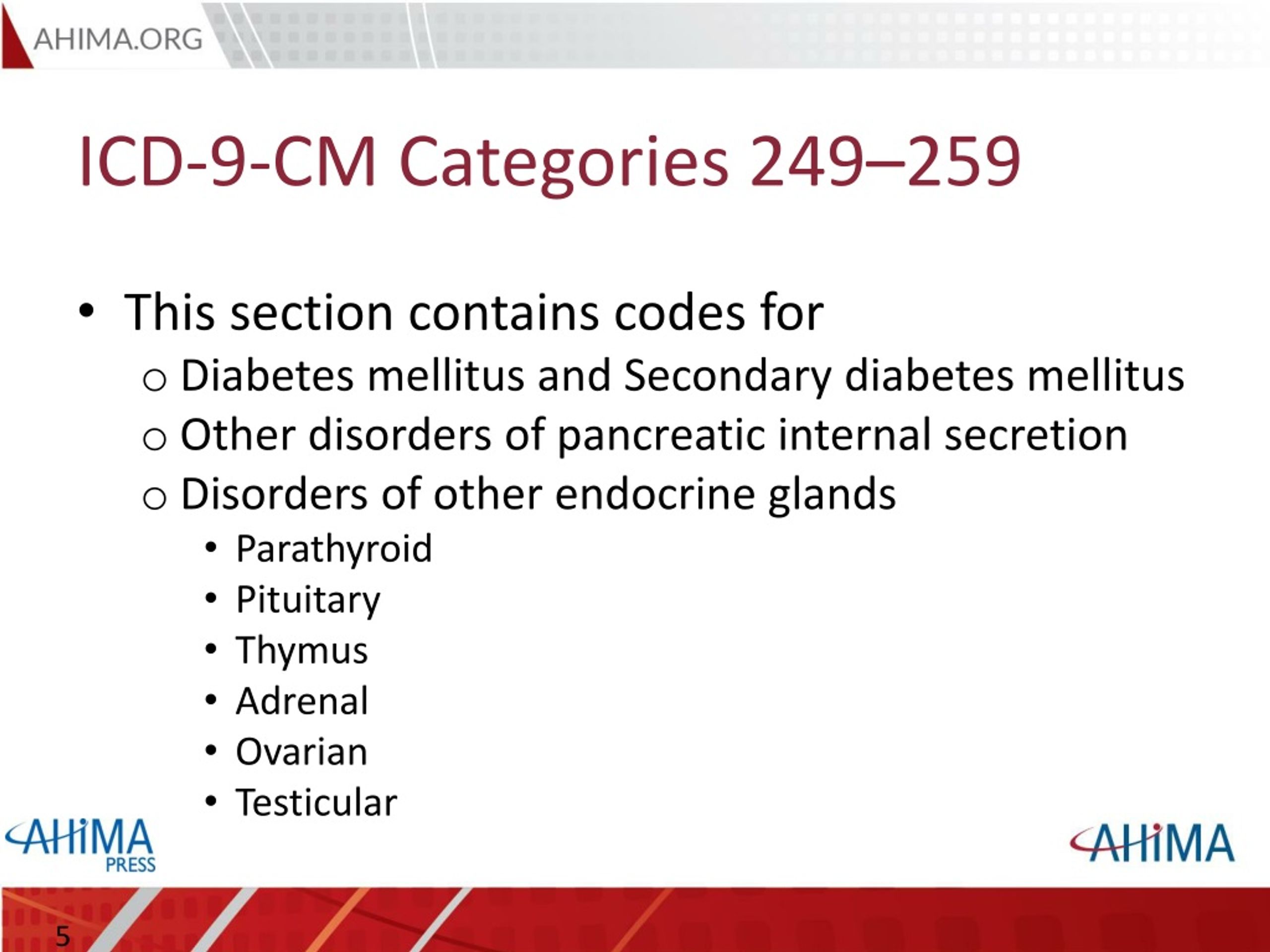
Hypercoagulable state, secondary; Thrombophilia; Hypercoagulable states NEC; Secondary hypercoagulable state NOS ICD-10-CM Diagnosis Code E67.1 [convert to ICD-9-CM]
What is a hypercoagulable patient?
Patients are considered to have a hypercoagulable state if they have laboratory abnormalities or clinical conditions that are associated with increased risk of thrombosis. The hypercoagulable states are a group of acquired and inherited disorders that increase the risk of abnormal development of blood clots.
What are the most common genetic disorders associated with hypercoagulopathy?
Prothrombin G20210A mutation—this is the second most common inherited factor associated hypercoagulopathy Protein C and Protein S deficiency—this is uncommon but these deficiencies fail to regulate the coagulation process properly Antithrombin (or antithrombin III) deficiency—this is a very rare autosomal dominant disorder
What is the ICD-10-CM code for Hypercoagulability?
D68. 69 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM D68. 69 became effective on October 1, 2021.
What does Hypercoagulability mean?
Hypercoagulability describes the pathologic state of exaggerated coagulation or coagulation in the absence of bleeding. Arterial thrombosis, such as in myocardial infarction and stroke, is different from venous thromboses, such as deep venous thrombosis (DVT) and pulmonary embolism (PE).
What is acquired thrombophilia?
Thrombophilia can be an inherited (genetic) or acquired tendency to form blood clots both in arteries and veins. Normally, your body makes a blood clot when you cut your finger with a knife, for example. The blood clot stops the bleeding. Later, your body breaks the clot apart when it's not needed anymore.
What is secondary hypercoagulable state?
Secondary hypercoagulable states are primarily acquired disorders that. predispose to thrombosis through complex and multifactorial mechanisms. These involve blood flow abnormalities or defects in blood composition and of. vessel walls.
What is procoagulant state?
A procoagulant state has been found to exist in diabetes mellitus. There may be activation of the intrinsic coagulation system, decreased fibrinolytic activity, or alterations in platelet function.
How is hypercoagulable state diagnosis?
Diagnosis of hypercoagulability can include blood tests to look at the levels of anticoagulant proteins, as well as genetic testing to identify the most common inherited thrombophilias.
Is thrombophilia the same as hypercoagulability?
Patients with acquired hypercoagulable states or hereditary thrombophilia are more likely to develop clots, venous thrombosis, and arterial thrombosis, than healthy individuals. Venous thrombosis and pulmonary embolism are associated with significant morbidity and mortality.
What does thrombophilia mean?
If you have thrombophilia, it means your blood can form clots too easily. Blood clots can be very serious and need to be treated quickly. Thrombophilia increases your risk of: deep vein thrombosis (DVT), a blood clot in a vein, usually the leg. pulmonary embolism (PE), a blocked blood vessel in your lungs.
What is the difference between hemophilia and thrombophilia?
While people with hemophilia have an increased tendency to bleed, people with thrombophilia have an increased tendency to clot. Just as hemophilia is caused by an abnormality of a blood-clotting factor, some forms of thrombophilia are also caused by an abnormality of a blood-clotting factor.
Is atrial fibrillation a secondary hypercoagulable state?
Examples of conditions that can cause secondary hypercoagulable states are atrial fibrillation, malignancy, pregnancy, trauma, myeloproliferative disorders, and antiphospholipid antibody syndrome.
What is acquired hypercoagulable state?
Abstract. Acquired hypercoagulable states comprise a diverse group of clinical conditions that are associated with an increased risk of thrombosis.
What are hypercoagulable conditions?
Hypercoagulable states are usually genetic (inherited) or acquired conditions. The genetic form of this disorder means a person is born with the tendency to form blood clots.
What is a coagulopathy?
Coagulopathy (clotting or bleeding disorder) Clinical Information. A condition in which there is a deviation from or interruption of the normal coagulation properties of the blood. Condition in which there is a deviation from or interruption of the normal coagulation properties of the blood.
When will the ICd 10 D68.9 be released?
The 2022 edition of ICD-10-CM D68.9 became effective on October 1, 2021.
What are the causes of hemorrhagic and thrombotic disorders?
Hemorrhagic and thrombotic disorders that occur as a consequence of abnormalities in blood coagulation due to a variety of factors such as coagulation protein disorders; blood platelet disorders; blood protein disorders or nutritional conditions.
Which mutation is most common in hypercoagulopathy?
Factor V Leiden mutation—this is the most common inherited factor associated hypercoagulopathy
What is a hypercoagulable state?
Hypercoagulable states are blood disorders that increase the risk of deep vein thrombosis or embolic disease. The state is either inherited or acquired. About 80% of patients with blood clots have been found to have either an inherited or acquired clotting disorder. These blood clots can be lethal and some require life-long therapy. Hypercoagulable state is also known as thrombophilia. The patients that fall into one of these disorders have an increased tendency to develop blood clots. This is due to the presence of either an inherited factor or an acquired factor.
What is the second most common cause of hypercoagulable state?
Malignancy/cancer is the second most common cause of hypercoagulable state and accounts for 10% to 20% of spontaneous venous thromboses
What are the disorders that affect coagulation?
These include the disorders such as protein C and S, heparin cofactor, antithrombin III, fibrinogen, factor XIII, prothrombin, and plasminogen
Does a venous thrombosis need to be documented before coding?
Does this support coding the thrombosis and also the hypercoagulable state? NO! Since there is a thrombus wouldn’t that mean that the patient has a hypercoagulable state? NO! The physician must document the diagnosis before it can be coded. No assumptions can be made. Not all patients with a thrombosis have a hypercoagulable state or disorder.
Can a coder determine if a patient has primary or secondary hypercoagulation?
If only hypercoagulable state is diagnosed, can the coder look at the patient’s other diseases/diagnoses and determine by that if they have primary or secondary? NO! Only the physician can make the link between the cause/effect.
Is hypercoagulable state documented?
The diagnosis of hypercoagulable state is documented, is it coded? That all depends on if it meets one of the criteria for reporting a diagnosis in ICD-10-CM. Chances are, the patient is under medical treatment for the condition or monitoring and follow up is normally required. If documentation is unclear, a query would be needed to clarify if this was clinically significant on the current admission. Most often, primary hypercoagulable state will be reported as these don’t go away. For the secondary hypercoagulable state, if the acquired disorder resolves, so may the hypercoagulable state in most patients.
What is the code for coagulopathy?
COVID-19 associated coagulopathy is reported using codes U07.1, COVID-19, and Other specified coagulation defects (D68.8). If skin failure due to the COVID-19 associated coagulopathy is documented, report COVID-19 (U07.1), Other specified coagulation defects (D68.8), and Other disorders of the skin and subcutaneous tissue in diseases classified elsewhere (L99).
Why is coagulopathy important in documentation?
The first and ultimate reason for excellent documentation is improved patient care through clear communication between providers and an accurate picture of the patient's medical situation and treatment course . It is essential to capture all the comorbidities conditions ...
What anticoagulants are being tested?
Other anticoagulants are being tested, such as antithrombin three, factor 10 A, and complement inhibitors. There is still much to be learned about the COVID-19 associated coagulopathy, but the fast and ongoing collaboration worldwide makes for a hopeful outcome.
Can a virus interfere with coagulation?
On the other hand, the virus can directly or indirectly interfere with coagulation pathways causing systemic thrombosis. Antiviral treatments are generally effective early in the disease course, while treatment strategies targeting coagulation and inflammation might be more promising for patients with severe COVID-19.
Is vascular coagulopathy dysregulated?
The strong association between COVID-19 and vascular coagulopathy may suggest that multiple molecular pathways are dysregulated during the disease s' clinical progression and thus contribute to the associated thrombosis.
What is hypercoagulable state?
The hypercoagulable states are a group of acquired and inherited disorders that increase the risk of abnormal development of blood clots.
What are the mechanisms of activation of the coagulation system following surgery or trauma?
The mechanisms of activation of the coagulation system following surgery or trauma are incompletely understood as of this presentation, but may include decreased venous blood flow in the lower extremities, diminished fibrinolysis, immobilization, the release or exposure of tissue factor, and depletion of endogenous anticoagulants such as antithrombin.
Can you code DVT for HCS?
The prophylactic intervention is regarding VTE. You will not code DVT for example since the patient has not developed it (yet.) You can, however, code the HCS if documented and supported by the provider since the patient has already developed it.
Popular Posts:
- 1. 2017 icd 10 code for stenosis of the left vertebral artery
- 2. icd-10 code for personal history of stroke
- 3. icd 10 cm code for secondary hypertension due to renal artery aneurysm
- 4. what is the icd 10 code for iron deficiency
- 5. icd 10 code for dementia related to brain injury
- 6. icd 10 code for s/p amputation
- 7. icd-10-cm code for sunstroke
- 8. icd 10 code for foraminal lateral recess central stenosis
- 9. icd 10 code for shortness of breath congestive heart failure
- 10. icd 9 code for cecialac disease