What is the ICD 10 code for consultation?
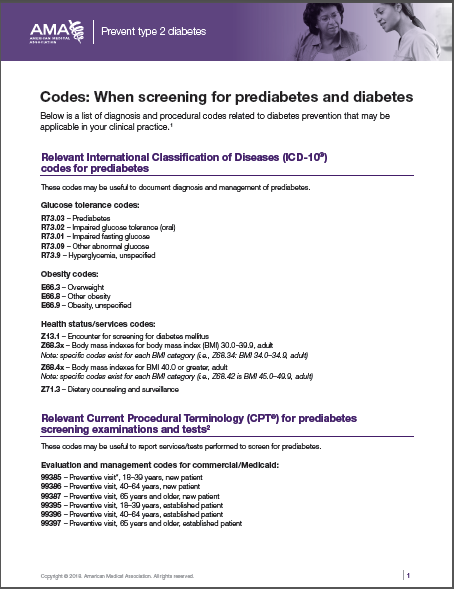
2018/2019 ICD-10-CM Diagnosis Code Z71.0. Person encountering health services to consult on behalf of another person. Z71.0 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
What is the CPT code for inpatient consultation?
In the hospital and nursing facility setting, the consulting physician or other qualified health care professional shall use the appropriate inpatient consultation CPT″ codes 99251-99255 for the initial consultation service. The initial inpatient consultation may be reported only once per consultant per patient per facility admission.
What is the CPT code for initial hospital visit?
Subsequent hospital visits should be coded using 99231-99233 (not discussed explicitly in this writing). Billing CPT Codes for Inpatient Initial Hospital Visits to Medicare: 99221:
What is the ICD 10 code for counseling?
Z71- Persons encountering health services for other counseling and medical advice, not elsewhere classified Z71.0 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2021 edition of ICD-10-CM Z71.0 became effective on October 1, 2020.
What is a medical expert request?
Is an office admission considered part of the initial hospital care?
Does Medicare recognize new or established billing codes?
How do I bill for inpatient consultation?
The correct inpatient consultation codes for a first evaluation are 99221-99223. These codes are used for the inpatient History and Physical (H & P), as well as any specialty consultation (limited to one visit from each specialty)....99222:50 minutes bedside.Comprehensive H & P.Moderate-level medical decision-making.
How do I code inpatient consults?
For non-Medicare patients, if the consultation is done after the patient is admitted to the hospital, consultation services may be reported with the inpatient consultation codes (99251– 99255). Consultation services in observation status are reported with the outpatient consultation codes (99241–99245).
What is the difference between 99223 and 99233?
If a doctor is asked to come in and "consult" and it fits the rules for billing a true consult, then yes you would bill a 99221-99223. However, if the doctor is "consulting" on a problem they will be managing or currently manage then you should bill a 99231-99233.
How do you code a consultation?
In the outpatient setting, if the attending physician requests advice or opinion regarding a problem and documents it in the medical record, the consultant physician can use an office consultation code (99241-99245).
What is an inpatient consultation?
Definitions. Inpatient Consultation An inpatient consultation service provided to a hospital inpatient by a physician whose opinion or advice regarding evaluation and/or management of a specific problem is requested by another physician or other appropriate source.
What is a hospital consultation?
Consultation – an in-depth discussion between you and the Consultant about your medical symptoms or condition. Preparing to visit us. At your outpatient visit, you will meet with the Consultant who will look after you throughout your treatment and, if necessary, your hospital stay.
What is the difference between 99232 and 99233?
Code 99232 identifies patients with minor complications requiring active, continuous management, or patients who aren't responding to treatment adequately. Code 99233 identifies unstable patients, or patients with significant new complications or problems.
Is CPT code 99223 inpatient or outpatient?
CPT 99223 represents the highest level of initial inpatient hospital care. CPT 99223 is defined as: Initial hospital care, per day, for the evaluation and management of a patient, which requires these three key components: A comprehensive history.
Does code 99223 need a modifier?
The documentation corresponds to the highest initial admission service, 99223. Given the recent Medicare billing changes, the attending of record is required to append modifier “AI” (principal physician of record) to the admission service (e.g., 99223–AI).
What is required to bill a consult?
CPT® defines a consultation as “a type of service provided by a physician whose opinion or advice regarding evaluation and/or management of a specific problem is requested by another physician or other appropriate source.” To substantiate a consultation service, documentation must include three elements: a request, a ...
What and how would the consultation be documented?
The entire process of consultation should be documented in the patient's chart: the request for consultation or, in the hospital, an order for the consultation; all physical findings and test results; a clear evaluation and recommendation; the attending physician's evaluation of the consultation and his or her own ...
What codes are used for inpatient billing?
Both ICD-10-CM and ICD-10-PCS coding manuals are used for inpatient coding. ICD-10-PCS is exclusively used for inpatient, hospital settings in the U.S. ICD-10 PCS excludes common procedures, lab tests, and educational sessions that are not unique to the inpatient, hospital setting.
What is the CPT code for hospital consultation?
Outpatient consultations (99241—99245) and inpatient consultations (99251—99255) are still active CPT® codes, and depending on where you are in the country, are recognized by a payer two, or many payers.
What are the three R's for coding consultations?
request, render and replyFrom this basic process comes the three “R's” of consultation coding: request, render and reply.
Are consult codes payable?
In 2010 the Centers for Medicare and Medicaid Services stopped paying for consultation codes. While it continued to recognize the concept of consults, it paid for them using new and established patient visit codes (99202 – 99215).
Can you bill a consult with a procedure?
In addition to admissions, discharge and daily patient care, hospitalists also perform consultations, prolonged services and bedside procedures, and must bill appropriately for these additional services. Physicians can select the appropriate Current Procedural Terminology (CPT) codes to bill for these services.
cpt code 99241, 99242, 99243, 99244, 99245 – Medicare Billing and ...
procedure code and description. 99241 – Office consultation for a new or established patient, which requires these 3 key components: A problem focused history; A problem focused examination; and Straightforward medical decision making. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or ...
2021 Consultation Codes Update | CPT codes 99241-99245, 99251-
Consultation Codes Update, June 2022: The May 2022 CPT Assistant announced there are changes coming to E/M codes in 2023, including consultations.
CPT code 99221, 99223, 99222 and 99233 – Inpatient hospital visits
99221 : Inpatient hospital visits: Initial and subsequent initial hospital care, per day, for the evaluation and management of a patient, which requires these 3 key components: A detailed or comprehensive history; A detailed or comprehensive examination; and Medical decision making that is straightforward or of low complexity. Counseling and/or…
CPT code 99251, 99252 , 99253, 99254, 99255 | Medical Billing and ...
CPT 97151, 97152, 97153, 97158, 0373T – Applied Behavior Analysis (ABA)
CPT 99211, 99212, 99213, 99214, 99215 – Established patient office ...
CPT 99211 Office or other outpatient visit for the evaluation and management of an established patient, that may not require the presence of a physician or other qualified health care professional.Usually, the presenting problem(s) are minimal. Typically, 5 minutes are spent performing or supervising these services. Billing Instructions: Bill 1 unit per visit.
What is a medical expert request?
A request (verbal or written) from the referring physician. The specific opinion or recommendations of the consulting physician. A written report of each service performed or ordered on the advice of the consulting physician. The medical expertise requested is beyond the specialty of the requesting physician.
Is an office admission considered part of the initial hospital care?
All services performed in an office and the resulting hospital admission are reflected (i.e., admission following any evaluation and management (E/M) services received by the patient in an office, emergency room, or nursing facility). If these services are on the same date as admission, they are considered part of the initial hospital care.
Does Medicare recognize new or established billing codes?
Second, the old initial consultation codes (99251-99255) are no longer recognized by Medicare Part B, although many non-Medicare providers still use them if ...
What is the CPT code for a hospital?
Physicians must meet all the requirements of the initial hospital care codes, including “a detailed or comprehensive history” and “a detailed or comprehensive examination” to report CPT code 99221, which are greater than the requirements for consultation codes 99251 and 99252. Physicians may report a subsequent hospital care code for services ...
What is the code for discharge day management?
The Hospital Discharge Day Management services (99238 or 99239) are not to be reported. When a patient has been admitted to inpatient hospital care for a minimum of 8 hours ...
What is the E&M code for admission and discharge?
Admission and Discharge Same Day – E&M codes (99234 – 99236) used to report services for a patient who is admitted and discharged from an observation or inpatient stay on the same calendar date. Patient’s stay must be a minimum of eight hours in order to bill these codes.
What is the CPT code for outpatient consultation?
For office and outpatient services, use new and established patient visit codes (99202—99215) , depending on whether the patient is new or established to the physician, following the CPT rule for new and established patient visits. Use these codes for consultations for patients in observation as well, because observation is an outpatient service.
What is the hospital code for inpatient care?
For an inpatient service, use the initial hospital services codes (99221—99223) . If the documentation doesn’t support the lowest level initial hospital care code, use a subsequent hospital care code (99231—99233). Don’t make the mistake of always using subsequent care codes, even if the patient is known to the physician.
What are the advantages of using a consult code?
The advantages to using the consult are codes are twofold: they are not defined as new or established, and may be used for patients the clinician has seen before, if the requirements for a consult are met and they have higher RVUs and payments. Category of code for payers that don’t recognize consult codes.
What is the CPT code for office consult?
For more information on office consults and Medicare consult codes, or to determine proper usage of CPT® codes 99241-99245, become a member of CodingIntel today.
When did CMS stop recognizing CPT codes?
CMS stopped recognizing consult codes in 2010. Outpatient consultations (99241—99245) and inpatient consultations (99251—99255) are still active CPT ® codes, and depending on where you are in the country, are recognized by a payer two, or many payers.
What is the ED code for observation?
For patients seen in the emergency department and sent home, use ED codes (99281—99285).
Can you crosswalk 99253 to 99255?
Based on the three key components, it is still possible to automatically crosswalk 99253—99255 exactly to 99221—99223. If the service is billed as 99251 or 99252, crosswalk it to a subsequent visit code 99231—99233. Since the requirements are slightly different (all three key components required for consults, and two of three required for a subsequent visit), the crosswalk isn’t automatic.
What is the CPT code for inpatient consultation?
Inpatient consultations are reported with CPT″ codes 99251-99255. The codes are used to report physician or other health care professional consultations provided to hospital inpatients, residents of nursing facilities, or patients in a partial hospital setting.
How many times can an inpatient consultation be reported?
The initial inpatient consultation may be reported only once per consultant per patient per facility admission. 2. In the office or outpatient setting, the consultant should use the appropriate office or outpatient consultation CPT″ codes 99241-99245 for the initial consultation service. 3. A consulting physician or other qualified health care ...
Who may initiate diagnostic services and treatment at the initial consultation service?
3. A consulting physician or other qualified health care professional may initiate diagnostic services and treatment at the initial consultation service or may even take over the patient’s care after the initial consultation.
What is a medical expert request?
A request (verbal or written) from the referring physician. The specific opinion or recommendations of the consulting physician. A written report of each service performed or ordered on the advice of the consulting physician. The medical expertise requested is beyond the specialty of the requesting physician.
Is an office admission considered part of the initial hospital care?
All services performed in an office and the resulting hospital admission are reflected (i.e., admission following any evaluation and management (E/M) services received by the patient in an office, emergency room, or nursing facility). If these services are on the same date as admission, they are considered part of the initial hospital care.
Does Medicare recognize new or established billing codes?
Second, the old initial consultation codes (99251-99255) are no longer recognized by Medicare Part B, although many non-Medicare providers still use them if ...
Popular Posts:
- 1. icd 10 code for abnormal radiologic in pelvis
- 2. icd 10 code for a flu shot
- 3. icd-10-pcs code for mri thyroid gland contrast unspecified
- 4. icd 10 code for psychophysiological dysuria
- 5. icd 9 code for bifurcation aneurysm
- 6. icd 10 code for pressure ulcer on left breast
- 7. icd 10 code for occlusive dvt left subclavian
- 8. icd 10 code for hep c
- 9. icd 9 code for brugada syndrome
- 10. external cause icd 10 code for death