What is skin lesion in ICD 10?
Skin lesion. Skin lesion of face. Skin lesion of foot. Skin lesion of left ear. Skin lesion of nose. Skin lesion of right ear. Skin or subcutaneous tissue disease. ICD-10-CM L98.9 is grouped within Diagnostic Related Group (s) (MS-DRG v38.0): 606 Minor skin disorders with mcc.
What is the ICD 10 code for dermatitis?
The condition is caused by moisture and friction and is characterized by erythema, maceration, burning, and exudation. Superficial dermatitis on opposed skin surfaces. ICD-10-CM L30.4 is grouped within Diagnostic Related Group (s) (MS-DRG v38.0): 606 Minor skin disorders with mcc. 607 Minor skin disorders without mcc.
What is the new ICD 10 for subcutaneous disordered tissue?
Disorder of the skin and subcutaneous tissue, unspecified. The 2019 edition of ICD-10-CM L98.9 became effective on October 1, 2018. This is the American ICD-10-CM version of L98.9 - other international versions of ICD-10 L98.9 may differ.
What is the ICD 10 code for intertrigo?
ICD-10-CM Diagnosis Code L30.9 ICD-10-CM Diagnosis Code L30.9 Erythema, erythematous (infectional) (inflammation) L53.9 ICD-10-CM Diagnosis Code L53.9 Intertrigo L30.4 ICD-10-CM Codes Adjacent To L30.4 Reimbursement claims with a date of service on or after October 1, 2015 require the use of ICD-10-CM codes.
What is the ICD-10 code for moisture associated skin damage?
IRRITANT CONTACT DERMATITIS DUE TO EXPOSURE TO UNSPECIFIED MOISTURE SOURCE (ICD-10-CM CODE L24. A0)
What is the ICD-10 code for skin lesions?
ICD-10 Code for Disorder of the skin and subcutaneous tissue, unspecified- L98. 9- Codify by AAPC.
What is the ICD-10 code for gluteal wound?
S31. 809A - Unspecified open wound of unspecified buttock [initial encounter]. ICD-10-CM.
What is code L98 9?
ICD-10 code: L98. 9 Disorder of skin and subcutaneous tissue, unspecified.
What is the ICD-10 code for benign skin lesion?
D23.9D23. 9 - Other benign neoplasm of skin, unspecified. ICD-10-CM.
What is the ICD-10 code for buttock lesion?
L02. 31 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM L02.
What is the ICD 10 code for right buttock wound?
ICD-10 Code for Unspecified open wound of right buttock- S31. 819- Codify by AAPC.
What is skin shearing?
Friction injury occurs when the epidermis or top layer of skin separates from the dermis or bottom layer of skin. This is what is often referred to as a 'rug burn. ' Shearing is pressure and friction, injuring the skin at the same time. It happens more often than people realize because it is so easy to occur.
What forms the gluteal fold?
The gluteal sulcus is formed by the posterior horizontal skin crease of the hip joint and overlying fat and is not formed by the lower border of the gluteus maximus muscle, which crosses the fold obliquely. It is one of the major defining features of the buttocks.
What is R53 83?
ICD-9 Code Transition: 780.79 Code R53. 83 is the diagnosis code used for Other Fatigue. It is a condition marked by drowsiness and an unusual lack of energy and mental alertness. It can be caused by many things, including illness, injury, or drugs.
What is the ICD-10 code for suspicious lesion?
ICD-10-CM Diagnosis Code B08 B08.
What is the ICD-10 code for skin lesion on neck?
Other benign neoplasm of skin of scalp and neck D23. 4 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM D23. 4 became effective on October 1, 2021.
What is neoplasm of unspecified behavior of bone soft tissue and skin?
A skin neoplasm of uncertain behavior is a skin growth whose behavior can't be predicted. This diagnosis is only reached after your doctor has conducted a biopsy and sent the sample to a pathologist for examination. There's no way to know whether it will develop into cancer or not.
What does a lesion look like?
Skin lesions are areas of skin that look different from the surrounding area. They are often bumps or patches, and many issues can cause them. The American Society for Dermatologic Surgery describe a skin lesion as an abnormal lump, bump, ulcer, sore, or colored area of the skin.
What is ICD 10 code for wound infection?
L08. 9 - Local infection of the skin and subcutaneous tissue, unspecified. ICD-10-CM.
What is subcutaneous fascia?
Subcutaneous fascia is an elastic layer of connective tissue, formed by loosely packed interwoven collagen fibers mixed with abundant elastic fibers [6,8], making it a unique fibroelastic layer that is easily stretched in various directions and then returned to its initial state.
What causes intergluteal clefts?
Experts agreed that linear lesions, also sometimes assessed as fissures, in the intergluteal cleft are caused by moisture, with or without a friction component , and should be classified as intertriginous ( between skin folds) dermatitis (inflammation of the skin).
What causes a full thickness skin ulcer?
As opposed to moisture damaged skin, pressure ulcers are ischemic injuries to the skin and underlying soft tissue that can result in full-thickness tissue damage, and are usually located over bony prominences or sometimes found under medical devices. Pressure and shear factors cause compression of the circulation, distortion of tissue and blood vessels, and reperfusion tissue injury that result in the full thickness skin damage. This was most likely the primary cause of what happened in the patients I observed, along with a trapped moisture component.
What is moisture-associated skin damage?
Moisture-associated skin damage (MASD) is the general term for inflammation or skin erosion caused by prolonged exposure to a source of moisture such as urine , stool, sweat, wound drainage, saliva, or mucus. It is proposed that for MASD to occur, another complicating factor is required in addition to mere moisture exposure. Possibilities include mechanical factors (friction), chemical factors (irritants contained in the moisture source), or microbial factors (microorganisms). The moisture barrier of the skin plays a critical role in maintaining homeostasis within the body, mainly by concurrently slowing the movement of water out of the body ( transepidermal water loss, or TEWL) and regulating the absorption of water and solutes from outside the body. When exposed to excessive amounts of moisture, the skin will soften, swell, and become wrinkled, all of which make the skin more susceptible to damage from one of the complicating factors mentioned above.
How to treat intertriginous dermatitis?
Keep at-risk areas clean and dry. Shower after exercise, then thoroughly pat dry the skin inside the fold. Use a pH-balanced skin cleanser. Promote proper general skin hygiene. The goal of treatment for intertriginous dermatitis is to minimize moisture and friction in the skin fold and to treat any infections.
How to treat periwound moisture dermatitis?
Manage wound exudate with dressings chosen for proper absorbency. Apply a barrier film or skin protectant to the periwound skin when appropriate. The first step in treatment of periwound moisture-associated dermatitis is managing the excessive exudate.
What happens if you have excessive wound exudate?
Excessive amounts of wound exudate can cause the periwound (within 4 cm of wound edge) skin to become macerated and even break down. This type of skin damage is call periwound moisture-associated dermatitis. The chemical composition of the wound exudate greatly affects the potential damage that can be wrought. ...
How does the moisture barrier help maintain homeostasis?
The moisture barrier of the skin plays a critical role in maintaining homeostasis within the body, mainly by concurrently slowing the movement of water out of the body ( transepidermal water loss, or TEWL) and regulating the absorption of water and solutes from outside the body.
What happens when you get too much moisture?
When exposed to excessive amounts of moisture, the skin will soften, swell, and become wrinkled, all of which make the skin more susceptible to damage from one of the complicating factors mentioned above. The four specific types of moisture-associated skin damage that will be discussed here are periwound moisture-associated dermatitis, ...
Is exudate a normal part of wound healing?
The production of exudate is a normal result of the inflammatory stage of wound healing. However, the advent of moist wound healing has brought with it an understanding that moisture balance is the key to optimal outcomes. Excessive amounts of wound exudate can cause the periwound (within 4 cm of wound edge) skin to become macerated and even break down. This type of skin damage is call periwound moisture-associated dermatitis.
Etiology
Symptoms
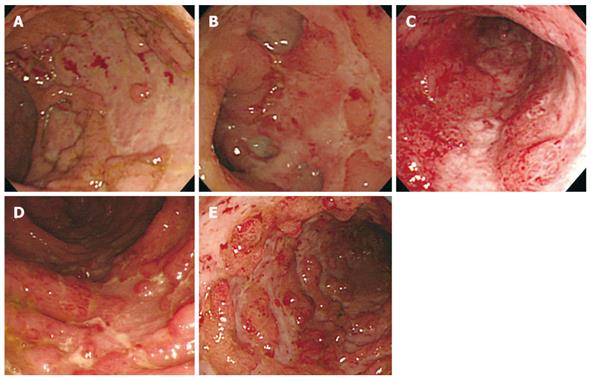
- Periwound moisture-associated dermatitis is marked by erythema (which may be harder to discern in persons with darkly pigmented skin), maceration (white, pale, or gray skin that is softened and/or wrinkled), and irregular or diffuse edges (as opposed to pressure ulcers which typically have distinct edges). Wounds with more viscous exudate are more prone to periwound …
Risk Factors
- The following wounds are more prone to developing periwound moisture-associated dermatitis: 1. Diabetic foot ulcers 2. Venous leg ulcers 3. Pressure ulcers 4. Fungating tumors 5. Full-thickness (third-degree) burns Wound infection will also greatly increase the risk of periwound maceration, as it increases the exudate production.
Treatment & Interventions
- The following precautions can help minimize the risk of developing periwound moisture-associated dermatitis in at-risk patients and to minimize complications in patients already exhibiting symptoms: 1. Monitor the wound area routinely for changes in skin condition. 2. Manage wound exudate with dressings chosen for proper absorbency. 3. Apply a barrier film or …
References
- Alvey B, Beck DE. Peristomal Dermatology. Clin Colon Rectal Surg. 2008;21(1):41-44. doi: 10.1055/s-2008-1055320 Black JM, Gray M, Bliss DZ, Kennedy-Evans KL, Logan S, Baharestani MM, Colwell JC, Goldberg M, Ratliff CR. MASD Part 2: Incontinence-Associated Dermatitis and Intertriginous Dermatitis. J Wound Ostomy Continence Nurs. 2011;38(4):359-370. doi: 10.1097/…
Popular Posts:
- 1. icd 10 code for confusion and disorientation
- 2. 2021 icd 10 code for hypertensive urgency
- 3. icd-10-cm pcs procedure code for decompression thoracic spine stenosis ??
- 4. icd code for accident washing glass at home
- 5. icd 9 diagnosis code for paraovarian cyst
- 6. icd 10 code for limp pain
- 7. icd 10 code for colic in newborn
- 8. icd 10 code for lab disorder nos
- 9. icd 10 code for nut allergy
- 10. icd 10 code for brain tia